Sunday, August 15, 2021 is the last day Americans can apply for special enrollment in health coverage in the federal health insurance exchange in 2021.
Comment On OSHA‘s Midified Aerial Lift Recordkeeping Requirements By 9/9
August 10, 2021September 9, 2021 is the deadline for employers and other interested parties to comment on the Occupational Safety & Health Administration (“OSHA”) information collection requirements regarding its Standard requiring when aerial lifts are ‘‘field modified’’ for uses other than those intended by the manufacturer, the manufacturer or other equivalent entity, such as a nationally recognized testing laboratory, must certify in writing that the modification is in conformity with all applicable provisions of ANSI A92.2–1969 and the OSHA standard and that the modified aerial lift is at least as safe as the equipment was before modification.
Existing standards also require employers to maintain the certification record and make it available to OSHA compliance officers. OSHA believes this certification record provides assurance to employers, workers, and compliance officers that the modified aerial lift is safe for use; thereby, preventing failure while workers are being elevated. The certification record also provides the most efficient means for the compliance officers to determine that an employer is complying with the Standard.
OSHA’s is inviting comments on:
- Whether the collection of information is necessary for the proper performance of the functions of the Department, including whether the information will have practical utility;
- If the information will be processed and used in a timely manner;
- The accuracy of the agency’s estimates of the burden and cost of the collection of information, including the validity of the methodology and assumptions used;
- Ways to enhance the quality, utility and clarity of the information collection; and
- Ways to minimize the burden of the collection of information on those who are to respond, including the use of automated collection techniques or other forms of information.
Heath Center Hit With $273K+ OSHA Fine For COVID-19 Safety Violations
August 5, 2021Lakewood Resource and Referral Center Inc., dba Center for Education Medicine and Dentistry (CHEMED) faces heavy fines for allegedly violating the Occupational Safety & Health Act (“OSHA”) by violating Occupational Safety and Health Administration (“OSH”) COVID-19 safety guidelines in January, 2021.
In a July 23, 2021 citation letter, OSH proposes to fine CHEMED
$273,064.00 for willfully violating OSHA by not providing a medical evaluation to determine each employee’s ability
to use a N95 respirator, before the employee was fit tested or required to use the respirator in the workplace
to protect against SARS-CoV-2 virus while testing suspected COVID-19 individuals.
In addition to the proposed fine, the citation also orders CHEMED to take a series of corrective actions and to post notices in the workplace informing workers of the violation.
Along with the CHEMED citation, OSH also cited a staffing agency contracted to provide nursing staffing to CHEMED, Homecare Therapies for also failing to conduct medical evaluations and fit tests. It received two violations and a proposed fine of $13,653.
The citations and proposed penalties illustrate the risks health industry and other employers face for failing to comply with COVID-19 safety protocols.
To reduce their exposure for similar violations, health care providers and other employers should carefully monitor and comply with all OSH COVID-19 and other safety standards and ensure their staffing and other contractors also meet these conditions.
More Information
This article is republished by permission of the author, Cynthia Marcotte Stamer. To review the original work, see here.
Solutions Law Press, Inc. invites you to receive future updates by registering here and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy. If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. For specific information about the these or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years working as an on demand, special project, consulting, general counsel or other basis with domestic and international business, charitable, community and government organizations of all types, sizes and industries and their leaders on labor and employment and other workforce compliance, performance management, internal controls and governance, compensation and benefits, regulatory compliance, investigations and audits, change management and restructuring, disaster preparedness and response and other operational, risk management and tactical concerns.
Most widely recognized for her work with health care, life sciences, insurance and data and technology organizations, she also has worked extensively with health plan and insurance, employee benefits, financial, transportation, manufacturing, energy, real estate, accounting and other services, public and private academic and other education, hospitality, charitable, civic and other business, government and community organizations. and their leaders.
Ms. Stamer has extensive experience advising, representing, defending, and training domestic and international public and private business, charitable, community and governmental organizations and their leaders, employers, employee benefit plans, their fiduciaries and service providers, insurers, and others has published and spoken extensively on these concerns. As part of these involvements, she has worked, published and spoken extensively on these and other human resources, employee benefits, compensation, worker classification and other workforce and other services; insurance; health care; workers’ compensation and occupational disease; business reengineering, disaster and distress; and many other performance, risk management, compliance, public policy and regulatory affairs, and other operational concerns.
A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally and domestically as an advisor to business, community and government leaders on these and other legislative, regulatory and other legislative and regulatory design, drafting, interpretation and enforcement, as well as regularly advises and represents organizations on the design, administration and defense of workforce, employee benefit and compensation, safety, discipline, reengineering, regulatory and operational compliance and other management practices and actions.
Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and provides insights and thought leadership through her extensive publications, public speaking and volunteer service with a diverse range of organizations including as Chair of the American Bar Association (“ABA”) Intellectual Property Section Law Practice Management Committee, Vice Chair of the International Section Life Sciences and Health Committee, Past ABA RPTE Employee Benefits & Other Compensation Group Chair and Council Representative and current Welfare Benefit Committee Co-Chair, Past Chair of the ABA Managed Care & Insurance Interest Group, past Region IV Chair and national Society of Human Resources Management Consultant Forum Board Member, past Texas Association of Business BACPAC Chair, Regional Chair and Dallas Chapter Chair, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation and many others.
For more information about these concerns or Ms. Stamer’s work, experience, involvements, other publications, or programs, see www.cynthiastamer.com, on Facebook, on LinkedIn or Twitter or e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns.
©2021 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™
Comment On OSHA Electrical Construction Data Collection
August 5, 2021September 7 is the deadline for construction industry employers and other concerned parties to comment on the information collected by the Occupational Safety Administration (“OSHA”) on Electrical Standards for Construction and for General Industry and their necessity for the prevention of inadvertent electrocution of workers.
Comments are invited on: (1) whether the collection of information is necessary for the proper performance of the functions of the Department, including whether the information will have practical utility; (2) if the information will be processed and used in a timely manner; (3) the accuracy of the agency’s estimates of the burden and cost of the collection of information, including the validity of the methodology and assumptions used; (4) ways to enhance the quality, utility and clarity of the information collection; and (5) ways to minimize the burden of the collection of information on those who are to respond, including the use of automated collection techniques or other forms of information technology.
Interested persons should submit any written comments on or before September 7, 2021 to http://www.reginfo.gov/public/do/ PRAMain. Find this particular information collection by selecting ‘‘Currently under 30-day Review—Open for Public Comments’’ or by using the search function.
More Information
This article is republished by permission of the author, Cynthia Marcotte Stamer. To review the original work, see here.
Solutions Law Press, Inc. invites you to receive future updates by registering here and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy. If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. For specific information about the these or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years working as an on demand, special project, consulting, general counsel or other basis with domestic and international business, charitable, community and government organizations of all types, sizes and industries and their leaders on labor and employment and other workforce compliance, performance management, internal controls and governance, compensation and benefits, regulatory compliance, investigations and audits, change management and restructuring, disaster preparedness and response and other operational, risk management and tactical concerns.
Most widely recognized for her work with health care, life sciences, insurance and data and technology organizations, she also has worked extensively with health plan and insurance, employee benefits, financial, transportation, manufacturing, energy, real estate, accounting and other services, public and private academic and other education, hospitality, charitable, civic and other business, government and community organizations. and their leaders.
Ms. Stamer has extensive experience advising, representing, defending, and training domestic and international public and private business, charitable, community and governmental organizations and their leaders, employers, employee benefit plans, their fiduciaries and service providers, insurers, and others has published and spoken extensively on these concerns. As part of these involvements, she has worked, published and spoken extensively on these and other human resources, employee benefits, compensation, worker classification and other workforce and other services; insurance; health care; workers’ compensation and occupational disease; business reengineering, disaster and distress; and many other performance, risk management, compliance, public policy and regulatory affairs, and other operational concerns.
A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally and domestically as an advisor to business, community and government leaders on these and other legislative, regulatory and other legislative and regulatory design, drafting, interpretation and enforcement, as well as regularly advises and represents organizations on the design, administration and defense of workforce, employee benefit and compensation, safety, discipline, reengineering, regulatory and operational compliance and other management practices and actions.
Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and provides insights and thought leadership through her extensive publications, public speaking and volunteer service with a diverse range of organizations including as Chair of the American Bar Association (“ABA”) Intellectual Property Section Law Practice Management Committee, Vice Chair of the International Section Life Sciences and Health Committee, Past ABA RPTE Employee Benefits & Other Compensation Group Chair and Council Representative and current Welfare Benefit Committee Co-Chair, Past Chair of the ABA Managed Care & Insurance Interest Group, past Region IV Chair and national Society of Human Resources Management Consultant Forum Board Member, past Texas Association of Business BACPAC Chair, Regional Chair and Dallas Chapter Chair, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation and many others.
For more information about these concerns or Ms. Stamer’s work, experience, involvements, other publications, or programs, see www.cynthiastamer.com, on Facebook, on LinkedIn or Twitter or e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns.
©2021 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™
Road Contractor To Pay $20.7 Million For Stealing Prevailing Wage Fringe Benefit Contributions
August 3, 2021Road construction giant Glenn O. Hawbaker will pay nearly $20.7 million in restitution to more than 1,200 workers after pleading guilty to stealing fringe benefit contributions the Davis-Bacon Act and the Pennsylvania Prevailing wage law required it pay for employees working on government road or other construction projects.
One of the largest road contractors in Pennsylvania, Glenn O. Hawbaker, Inc. pled no contest to four counts of theft relating to violations of the Pennsylvania Prevailing Wage Act and the federal Davis-Bacon Act filed by Pennsylvania Attorney General Josh Shapiro in April.
The $20,696,453 restitution payment is the largest prevailing wage restitution payment on history. In addition to making restitution, the company will have a court-appointed corporate monitor at company expense monitor it’s compliance while serving its probation.
The Davis-Bacon Act and state prevailing wage laws require contractors and subcontractors serving on government funded construction projects to pay workers prevailing wages and a specified fringe benefit contribution. for each hour worked.
The prosecution serves as a warning to other government contractors to carefully comply with these rules.
U.S. Secretary of Labor Marty Walsh warned other contractors to comply in his the statement on Glenn O. Hawbaker Inc. Plea and sentencing, stating:
“Today’s plea and sentencing of Hawbaker Inc. is a victory for the more than 1,200 workers whose hard-earned money was stolen. Ensuring workers get all the money owed them is a priority for the U.S. Department of Labor, and our partners in state government, when they act with courage and conviction as Pennsylvania Attorney General Josh Shapiro has in this case, can help us secure more just outcomes for workers.
All Employers Face ERISA Risks For Failing To Timely Deposit Contributions
Beyond the prevailing wage violations, withholding but failing to timely deposit pension, health or other fringe benefit contributions also can trigger substantial criminal and civil liability for an employing business and its owners and management under the Employee Retirement Income Security Act (“ERISA”). The Department of Justice and Employee Benefits Security Administration vigorously investigate and enforce these rules including seeking criminal convictions against management or others found to have misappropriated these funds. As these criminal violations are felonies, the Federal Sentencing Guidelines organizational liabilities attach. Accordingly, appropriate internal controls to prevent and auditing to catch and address these violations.
Fiduciaries also can face civil liability from the Employee Benefit Security Administration and private plaintiffs.
Rising Enforcement & Changing Policies Heighten Risks
Risks of these and other workforce liabilities are rising as the current Administration makes investigation and enforcement of wage and other employment, labor and benefit laws a priority.
Employers should keep in mind that the Davis-Bacon and other prevailing wage and wage and hour laws generally place the burden upon the employer to prove the their compliance both with strict pay and recordkeeping requirements.
The Biden-Harris Administration’s revocation of Trump-era rules also are heightening the risk of reclassification of subcontractors or other non-employee workers as employed or joint employees. As reclassification often makes it very difficult to prove compliance, contractors and other employees should reevaluate their non-employee service provider risks and contract to obtain and preserve all evidence relevant to prove compliance for these workers as well as employees.
More Information
This article is republished by permission of the author, Cynthia Marcotte Stamer. To review the original work, see here.
Solutions Law Press, Inc. invites you to receive future updates by registering here and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy. If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. For specific information about the these or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years working as an on demand, special project, consulting, general counsel or other basis with domestic and international business, charitable, community and government organizations of all types, sizes and industries and their leaders on labor and employment and other workforce compliance, performance management, internal controls and governance, compensation and benefits, regulatory compliance, investigations and audits, change management and restructuring, disaster preparedness and response and other operational, risk management and tactical concerns.
Most widely recognized for her work with health care, life sciences, insurance and data and technology organizations, she also has worked extensively with health plan and insurance, employee benefits, financial, transportation, manufacturing, energy, real estate, accounting and other services, public and private academic and other education, hospitality, charitable, civic and other business, government and community organizations. and their leaders.
Ms. Stamer has extensive experience advising, representing, defending, and training domestic and international public and private business, charitable, community and governmental organizations and their leaders, employee benefit plans, their fiduciaries and service providers, insurers, and others has published and spoken extensively on these concerns. As part of these involvements, she has worked, published and spoken extensively on these and other human resources, employee benefits, compensation, worker classification and other workforce and other services; insurance; health care; workers’ compensation and occupational disease; business reengineering, disaster and distress; and many other performance, risk management, compliance, public policy and regulatory affairs, and other operational concerns.
A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally and domestically as an advisor to business, community and government leaders on these and other legislative, regulatory and other legislative and regulatory design, drafting, interpretation and enforcement, as well as regularly advises and represents organizations on the design, administration and defense of workforce, employee benefit and compensation, safety, discipline, reengineering, regulatory and operational compliance and other management practices and actions.
Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and provides insights and thought leadership through her extensive publications, public speaking and volunteer service with a diverse range of organizations including as Chair of the American Bar Association (“ABA”) Intellectual Property Section Law Practice Management Committee, Vice Chair of the International Section Life Sciences and Health Committee, Past ABA RPTE Employee Benefits & Other Compensation Group Chair and Council Representative and current Welfare Benefit Committee Co-Chair, Past Chair of the ABA Managed Care & Insurance Interest Group, past Region IV Chair and national Society of Human Resources Management Consultant Forum Board Member, past Texas Association of Business BACPAC Chair, Regional Chair and Dallas Chapter Chair, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation and many others.
For more information about these concerns or Ms. Stamer’s work, experience, involvements, other publications, or programs, see www.cynthiastamer.com, on Facebook, on LinkedIn or Twitter or e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns.
©2021 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™
Model Notice & Related Guidance For Complying With COVID Bill COBRA Subsidy Rules Released; Send Notices & Begin Compliance ASAP
April 7, 2021Group health plans, their plan administrators and fiduciaries, employer or other sponsors, administrative services providers and insurers should act quickly to distribute required notices using the regulatory guidance just released today (April 7, 2021) and take other actions needed to comply with the Consolidated Omnibus Reconciliation Act of 1985 (“COBRA”) coverage and premium subsidy notification, enrollment and coverage continuation requirements created by Section 9501 (the “COBRA Premium Assistance Rules”) of the American Rescue Plan Act of 2021 (“ARP ”) enacted last month.
The guidance package released today by the Employee Benefit Security Administration includes model notices and other preliminary guidance on the COBRA Premium Assistance Rules, which among other things require group health plans to notify “assistance eligible individuals” no later than May 31, 2021 of right under ARP Section 9501 to enroll in free COBRA Coverage during the ARP Premium Subsidy Period that began April 1, 2021.
As the deadline for providing notification to qualified beneficiaries is May 31, 2021 and the 60 day period for enrolling in COBRA coverage under the ARP COBRA Subsidy Rules does not begin until proper notification is provided, group health plan should move quickly to prepare and distribute the notifications and make other necessary plan arrangements.
This article provides an general overview of the ARP COBRA Premium Subsidy Rules and the Model Notices published by the Department of Labor Employee Benefit Security Administration (“EBSA”) on April 7, 2021 to assist group health plans and their administrators to comply with their notification obligations under these Rules. For a more comprehensive discussion of these requirements, see here.
New COVID COBRA Premium Subsidy Rules Overview
Section 9501 of the ARP seeks to help “assistance eligible individuals” continue their health benefits by providing assistance to maintain enrollment in covered group health plans by allowing them to enroll and maintain COBRA coverage under those plans without paying their COBRA continuation coverage premiums.
Covered group health plans generally include all group health plans sponsored by private-sector employers or employee organizations (unions) subject to the COBRA rules under the Employee Retirement Income Security Act of 1974 (ERISA); group health plans sponsored by State or local governments subject to the continuation provisions under the Public Health Service Act and group health insurance required to comply with state mini-COBRA laws.
In addition to mandating the provision of COBRA Coverage at no cost, no later than May 31, 2021, the ARP requires covered group health plans to notify certain former covered employees or dependents that qualify to enroll in COBRA coverage as “assistance eligible individuals” of their right within 60 days of notification to enroll in COBRA Coverage under the group health plan at no cost from April 1, 2021 through September 30, 2021 or, if earlier, the date their COBRA eligibility otherwise end (the “Premium Subsidy Period”).
From April 1 to September 31, 2021, group health plans cannot require an assistance eligible individual to pay any premiums for COBRA Coverage during his Premium Subsidy Period. ARP requires group health plans to provide COBRA Coverage without charge to assistance eligible individuals who qualify for and elect to enroll in COBRA Coverage with premium subsidy unless individual’s eligibility for COBRA or COBRA premium assistance ends before that date. Specific notifications to qualified beneficiaries also are required.
To implement these rules, ARP also requires that no later than May 31, 2021, covered group health plan administrators notify eligible qualified beneficiaries eligible to obtain COBRA coverage with premium assistance by applying for enrollment within the 60 day period following notification.
Assistance eligible individuals who timely enroll in COBRA Coverage with premium assistance generally must receive COBRA Coverage free of charge from the group health plan for any coverage period during the period that begins on or after April 1, 2021 until the earliest of the following dates (the “Premium Subsidy Period”):[1]
- The date the qualified beneficiary is eligible[2] for coverage under any other group health plan (other than coverage consisting of only excepted benefits,[3] coverage under a health flexible spending arrangement under Code Section 106(c)(2), coverage under a qualified small employer health reimbursement arrangement under Code Section 9831(d)(2) or eligible for benefits under the Medicare program under title XVIII of the Social Security Act;
- The date of the expiration of the otherwise applicable maximum period of COBRA continuation coverage under Code Section 4980B (other than due to a failure to elect or discontinuation of coverage for nonpayment of COBRA premium that occurred before April 1, 2021).
Assistance eligible individuals generally are qualified beneficiaries who lost coverage under the group health plan due to an involuntary reduction in hours or termination of employment enrolled in COBRA Coverage between April 1, 2021 and September 31, 2021 including those qualifying event was an involuntary employment loss occurring during the 18-month period (29-months for individuals qualifying for extended COBRA eligibility due to disability) prior to April 1, 2021 not enrolled in COBRA as of April 1, 2021. This generally includes COBRA qualified beneficiaries whose loss of group health coverage results from an involuntary employment reduction or loss for a reason other than gross misconduct after ARP’s enactment on March 11, 2021 as well as qualified beneficiaries whose involuntary employment loss happened before the effective date who but for their previous failure to elect COBRA or to maintain COBRA Coverage would still be entitled to COBRA Coverage because less than 18 months (29 months for qualified beneficiaries disabled on the date of coverage loss who qualify for extension of the disability coverage period) has elapsed since their employment loss and an event has not occurred following the coverage termination that would terminate their COBRA eligibility before the end of such otherwise applicable maximum COBRA eligibility period. Group health plans must offer a second opportunity to enroll in COBRA Coverage with COBRA premium assistance to qualified beneficiaries eligible for premium assistance not enrolled in COBRA Coverage as of April 1, 2021.
Sponsoring employers or other plan sponsors may qualify to claim an employment tax credit for COBRA premiums paid on behalf of assistance eligible individuals. Guidance on these tax rules is pending.
Required Group Health Plan Notifications To Assistance Eligible Individuals
ARP requires group health plans to provide certain written notifications to qualified beneficiaries entitled to qualify to enroll in COBRA coverage with premium assistance. This generally includes a requirement to provide an initial notification of the availability of premium assistance for COBRA coverage to assistance eligible individuals by the later of May 31, 2021 and subsequently to provide notice of the impending termination of eligibility for the COBRA Premium Subsidy during the 30 day period that begins 45 days before eligibility for COBRA Premium Subsidy ends. ARP dictates the minimum required content of such notices. Failure to provide the required notification is a failure to meet the notice requirements under the applicable COBRA continuation provision that subjects the group health plan administer and its sponsor to liability.
While ARP allows plan administrators the option of designing their own notices and forms to fulfill this requirement, it also directed the Department of Labor in consultation with the Secretary of the Treasury and the Secretary of Health and Human Services to develop model notices for plans to use for this purpose. In response to this directive, the Department of Labor EBSA on April 7, 2021 published the following model notices and forms for group health plans to use to fulfill their ARP COBRA Premium Subsidy Rule notification requirements:
- General Notice and Election Notice
- Notice in Connection with Extended Election Period
- Alternative Notice;
- Summary of the COBRA Premium Assistance Provisions;and
- Notice of Expiration of Premium Assistance.
More Information
The ARP COBRA Premium Subsidy Rules are only one of a plethora of COVID health care emergency driven regulatory and enforcement changes impacting employers and their employee benefit plans. If you need assistance or would like additional information about these or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. also invites you receive future updates by registering here and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy. If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. For specific information about the these or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years working as an on demand, special project, consulting, general counsel or other basis with domestic and international business, charitable, community and government organizations of all types, sizes and industries and their leaders on labor and employment and other workforce compliance, performance management, internal controls and governance, compensation and benefits, regulatory compliance, investigations and audits, change management and restructuring, disaster preparedness and response and other operational, risk management and tactical concerns.
Most widely recognized for her work with workforce, health care, life sciences, insurance and data and technology organizations, she also has worked extensively with health plan and insurance, employee benefits, financial, transportation, manufacturing, energy, real estate, accounting and other services, public and private academic and other education, hospitality, charitable, civic and other business, government and community organizations. and their leaders.
Ms. Stamer has extensive experience advising, representing, defending and training domestic and international public and private business, charitable, community and governmental organizations and their leaders, employee benefit plans, their fiduciaries and service providers, insurers, and others has published and spoken extensively on these concerns. As part of these involvements, she has worked, published and spoken extensively on these and other federal and state wage and hour and other compensation, discrimination, performance management, and other related human resources, employee benefits and other workforce and services; insurance; workers’ compensation and occupational disease; business reengineering, disaster and distress; and many other risk management, compliance, public policy and performance concerns.
A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally and domestically as an advisor to business, community and government leaders on these and other legislative, regulatory and other legislative and regulatory design, drafting, interpretation and enforcement, as well as regularly advises and represents organizations on the design, administration and defense of workforce, employee benefit and compensation, safety, discipline, reengineering, regulatory and operational compliance and other management practices and actions.
Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and provides insights and thought leadership through her extensive publications, public speaking and volunteer service with a diverse range of organizations including as Chair of the American Bar Association (“ABA”) Intellectual Property Section Law Practice Management Committee, Vice Chair of the International Section Life Sciences and Health Committee, Past ABA RPTE Employee Benefits & Other Compensation Group Chair and Council Representative and current Welfare Benefit Committee Co-Chair, Past Chair of the ABA Managed Care & Insurance Interest Group, past Region IV Chair and national Society of Human Resources Management Consultant Forum Board Member, past Texas Association of Business BACPAC Chair, Regional Chair and Dallas Chapter Chair, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation and many others.
For more information about these concerns or Ms. Stamer’s work, experience, involvements, other publications, or programs, see www.cynthiastamer.com or contact Ms. Stamer via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns.
©2021 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™
Group health plans, their plan administrators and fiduciaries, employer or other sponsors, administrative services providers and insurers should act quickly to distribute required notices using the regulatory guidance just released today (April 7, 2021) and take other actions needed to comply with the Consolidated Omnibus Reconciliation Act of 1985 (“COBRA”) coverage and premium subsidy notification, enrollment and coverage continuation requirements created by Section 9501 (the “COBRA Premium Assistance Rules”) of the American Rescue Plan Act of 2021 (“ARP ”) enacted last month.
The guidance package released today by the Employee Benefit Security Administration includes model notices and other preliminary guidance on the COBRA Premium Assistance Rules, which among other things require group health plans to notify “assistance eligible individuals” no later than May 31, 2021 of right under ARP Section 9501 to enroll in free COBRA Coverage during the ARP Premium Subsidy Period that began April 1, 2021.
As the deadline for providing notification to qualified beneficiaries is May 31, 2021 and the 60 day period for enrolling in COBRA coverage under the ARP COBRA Subsidy Rules does not begin until proper notification is provided, group health plan should move quickly to prepare and distribute the notifications and make other necessary plan arrangements.
This article provides an general overview of the ARP COBRA Premium Subsidy Rules and the Model Notices published by the Department of Labor Employee Benefit Security Administration (“EBSA”) on April 7, 2021 to assist group health plans and their administrators to comply with their notification obligations under these Rules. For a more comprehensive discussion of these requirements, see here.
New COVID COBRA Premium Subsidy Rules Overview
Section 9501 of the ARP seeks to help “assistance eligible individuals” continue their health benefits by providing assistance to maintain enrollment in covered group health plans by allowing them to enroll and maintain COBRA coverage under those plans without paying their COBRA continuation coverage premiums.
Covered group health plans generally include all group health plans sponsored by private-sector employers or employee organizations (unions) subject to the COBRA rules under the Employee Retirement Income Security Act of 1974 (ERISA); group health plans sponsored by State or local governments subject to the continuation provisions under the Public Health Service Act and group health insurance required to comply with state mini-COBRA laws.
In addition to mandating the provision of COBRA Coverage at no cost, no later than May 31, 2021, the ARP requires covered group health plans to notify certain former covered employees or dependents that qualify to enroll in COBRA coverage as “assistance eligible individuals” of their right within 60 days of notification to enroll in COBRA Coverage under the group health plan at no cost from April 1, 2021 through September 30, 2021 or, if earlier, the date their COBRA eligibility otherwise end (the “Premium Subsidy Period”).
From April 1 to September 31, 2021, group health plans cannot require an assistance eligible individual to pay any premiums for COBRA Coverage during his Premium Subsidy Period. ARP requires group health plans to provide COBRA Coverage without charge to assistance eligible individuals who qualify for and elect to enroll in COBRA Coverage with premium subsidy unless individual’s eligibility for COBRA or COBRA premium assistance ends before that date. Specific notifications to qualified beneficiaries also are required.
To implement these rules, ARP also requires that no later than May 31, 2021, covered group health plan administrators notify eligible qualified beneficiaries eligible to obtain COBRA coverage with premium assistance by applying for enrollment within the 60 day period following notification.
Assistance eligible individuals who timely enroll in COBRA Coverage with premium assistance generally must receive COBRA Coverage free of charge from the group health plan for any coverage period during the period that begins on or after April 1, 2021 until the earliest of the following dates (the “Premium Subsidy Period”):[1]
- The date the qualified beneficiary is eligible[2] for coverage under any other group health plan (other than coverage consisting of only excepted benefits,[3] coverage under a health flexible spending arrangement under Code Section 106(c)(2), coverage under a qualified small employer health reimbursement arrangement under Code Section 9831(d)(2) or eligible for benefits under the Medicare program under title XVIII of the Social Security Act;
- The date of the expiration of the otherwise applicable maximum period of COBRA continuation coverage under Code Section 4980B (other than due to a failure to elect or discontinuation of coverage for nonpayment of COBRA premium that occurred before April 1, 2021).
Assistance eligible individuals generally are qualified beneficiaries who lost coverage under the group health plan due to an involuntary reduction in hours or termination of employment enrolled in COBRA Coverage between April 1, 2021 and September 31, 2021 including those qualifying event was an involuntary employment loss occurring during the 18-month period (29-months for individuals qualifying for extended COBRA eligibility due to disability) prior to April 1, 2021 not enrolled in COBRA as of April 1, 2021. This generally includes COBRA qualified beneficiaries whose loss of group health coverage results from an involuntary employment reduction or loss for a reason other than gross misconduct after ARP’s enactment on March 11, 2021 as well as qualified beneficiaries whose involuntary employment loss happened before the effective date who but for their previous failure to elect COBRA or to maintain COBRA Coverage would still be entitled to COBRA Coverage because less than 18 months (29 months for qualified beneficiaries disabled on the date of coverage loss who qualify for extension of the disability coverage period) has elapsed since their employment loss and an event has not occurred following the coverage termination that would terminate their COBRA eligibility before the end of such otherwise applicable maximum COBRA eligibility period. Group health plans must offer a second opportunity to enroll in COBRA Coverage with COBRA premium assistance to qualified beneficiaries eligible for premium assistance not enrolled in COBRA Coverage as of April 1, 2021.
Sponsoring employers or other plan sponsors may qualify to claim an employment tax credit for COBRA premiums paid on behalf of assistance eligible individuals. Guidance on these tax rules is pending.
Required Group Health Plan Notifications To Assistance Eligible Individuals
ARP requires group health plans to provide certain written notifications to qualified beneficiaries entitled to qualify to enroll in COBRA coverage with premium assistance. This generally includes a requirement to provide an initial notification of the availability of premium assistance for COBRA coverage to assistance eligible individuals by the later of May 31, 2021 and subsequently to provide notice of the impending termination of eligibility for the COBRA Premium Subsidy during the 30 day period that begins 45 days before eligibility for COBRA Premium Subsidy ends. ARP dictates the minimum required content of such notices. Failure to provide the required notification is a failure to meet the notice requirements under the applicable COBRA continuation provision that subjects the group health plan administer and its sponsor to liability.
While ARP allows plan administrators the option of designing their own notices and forms to fulfill this requirement, it also directed the Department of Labor in consultation with the Secretary of the Treasury and the Secretary of Health and Human Services to develop model notices for plans to use for this purpose. In response to this directive, the Department of Labor EBSA on April 7, 2021 published the following model notices and forms for group health plans to use to fulfill their ARP COBRA Premium Subsidy Rule notification requirements:
- General Notice and Election Notice
- Notice in Connection with Extended Election Period
- Alternative Notice;
- Summary of the COBRA Premium Assistance Provisions;and
- Notice of Expiration of Premium Assistance.
More Information
The ARP COBRA Premium Subsidy Rules are only one of a plethora of COVID health care emergency driven regulatory and enforcement changes impacting employers and their employee benefit plans. If you need assistance or would like additional information about these or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. also invites you receive future updates by registering here and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy. If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. For specific information about the these or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years working as an on demand, special project, consulting, general counsel or other basis with domestic and international business, charitable, community and government organizations of all types, sizes and industries and their leaders on labor and employment and other workforce compliance, performance management, internal controls and governance, compensation and benefits, regulatory compliance, investigations and audits, change management and restructuring, disaster preparedness and response and other operational, risk management and tactical concerns.
Most widely recognized for her work with workforce, health care, life sciences, insurance and data and technology organizations, she also has worked extensively with health plan and insurance, employee benefits, financial, transportation, manufacturing, energy, real estate, accounting and other services, public and private academic and other education, hospitality, charitable, civic and other business, government and community organizations. and their leaders.
Ms. Stamer has extensive experience advising, representing, defending and training domestic and international public and private business, charitable, community and governmental organizations and their leaders, employee benefit plans, their fiduciaries and service providers, insurers, and others has published and spoken extensively on these concerns. As part of these involvements, she has worked, published and spoken extensively on these and other federal and state wage and hour and other compensation, discrimination, performance management, and other related human resources, employee benefits and other workforce and services; insurance; workers’ compensation and occupational disease; business reengineering, disaster and distress; and many other risk management, compliance, public policy and performance concerns.
A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally and domestically as an advisor to business, community and government leaders on these and other legislative, regulatory and other legislative and regulatory design, drafting, interpretation and enforcement, as well as regularly advises and represents organizations on the design, administration and defense of workforce, employee benefit and compensation, safety, discipline, reengineering, regulatory and operational compliance and other management practices and actions.
Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and provides insights and thought leadership through her extensive publications, public speaking and volunteer service with a diverse range of organizations including as Chair of the American Bar Association (“ABA”) Intellectual Property Section Law Practice Management Committee, Vice Chair of the International Section Life Sciences and Health Committee, Past ABA RPTE Employee Benefits & Other Compensation Group Chair and Council Representative and current Welfare Benefit Committee Co-Chair, Past Chair of the ABA Managed Care & Insurance Interest Group, past Region IV Chair and national Society of Human Resources Management Consultant Forum Board Member, past Texas Association of Business BACPAC Chair, Regional Chair and Dallas Chapter Chair, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation and many others.
For more information about these concerns or Ms. Stamer’s work, experience, involvements, other publications, or programs, see www.cynthiastamer.com or contact Ms. Stamer via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns.
©2021 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™
Avoid Internship FLSA Minimum Wage & Overtime Traps
March 3, 2021Is your organization considering offering or receiving requests from students or others seeking paid or unpaid internships? Properly structured internships can prove highly beneficial for both the sponsoring employer and the intern. Before you jump in, make sure you’ve considered and covered the Fair Labor Standards Act (“FLSA”) traps.
The FLSA generally requires “for-profit” employers to pay interns in accordance with the minimum wage and overtime requirements of the FLSA if the internship results in the intern providing services as an “employee” within the meaning of the FLSA. An employer fails to pay an intern who is an employee for FLSA purposes at least minimum wage for regular hours of work or time and a half for any overtime worked risks being required to pay back pay, interest, and liquidated damages plus attorneys fees and costs of enforcement in the case of private enforcement or administrative penalties in the case of enforcement by the Department of Labor Wage and Hour Division.
As is generally the case under the FLSA, an employer that violates the FLSA by failing to pay an intern who is an employee at least minimum wage for regular hours of work or time and a half for any overtime worked risks being required to pay back pay, interest, and liquidated damages plus attorneys fees and costs of enforcement in the case of private enforcement or administrative penalties in the case of enforcement by the Department of Labor Wage and Hour Division.
One clear way a business can sidestep these FLSA risks is to pay any intern at least minimum wage for regular hours of work and time and time and a half for any overtime hours of work.
Where an employer is unwilling to pay an intern at least the minimum amounts required by wage and hour law, the employer should confirm and preserve evidence to prove the intern and not the organization was the primary beneficiary of the relationship taking into account all of the economic realities of the relationship.
Employers should keep in mind that the FLSA places the burden upon the employer to prove the justification for not treating and paying an intern as an employee under the FLSA by showing that the intern and not the employer is the “primary beneficiary” of the internship. While no single factor is determinative, some of the factors identified by the courts as as relevant for purposes of determining the economic reality of the relationship include:
- The extent to which the intern and the employer clearly understand that there is no expectation of compensation. Any promise of compensation, express or implied, suggests that the intern is an employee—and vice versa.
- The extent to which the internship provides training that would be similar to that which would be given in an educational environment, including the clinical and other hands-on training provided by educational institutions.
- The extent to which the internship is tied to the intern’s formal education program by integrated coursework or the receipt of academic credit.
- The extent to which the internship accommodates the intern’s academic commitments by corresponding to the academic calendar.
- The extent to which the internship’s duration is limited to the period in which the internship provides the intern with beneficial learning.
- The extent to which the intern’s work complements, rather than displaces, the work of paid employees while providing significant educational benefits to the intern.
- The extent to which the intern and the employer understand that the internship is conducted without entitlement to a paid job at the conclusion of the internship.
Because of the potential risks of misclassification of the relationship, an employer contemplating involvement in an unpaid or below minimum wage internship arrangement should carefully document and preserve all evidence relevant to prove that the internship was not employment under the economic realities. Because of the heightened requirements and liability exposures, this is even more critical when providing internships to an individual who could be covered by child labor laws.
To reduce the risk of missteps or unexpected consequences, employers also may wish to ask legal counsel experienced in the FLSA and other workforce laws to provide guidance about the proposed relationship under the FLSA and other laws. Employers should keep in mind that state minimum wage and other pay laws, OSHA and other safety, tax and other law may apply different definitions for purposes of deciding their treatment of an internship relationship. The business will want to understand and preserve analysis and relevant evidence to help support its characterization under the FLSA and other laws.
Additionally, whether paid or unpaid, employers also should carefully document the understanding between the parties about the relationship and its terms. Employers also keep careful time and other records needed to show or defend compliance and other elements of the relationship. Even where the relationship is not characterized as an employment one, employers also will want to use care not to skip or cut corners on background checks, privacy, security, intellectual property, safety, or other requirements. If the relationship is not one of employment, the employer also should consult with its insurance broker about the availability of or advisability of securing coverage for injuries or other actions or events involving the intern.
More Information
This article is republished by permission of the author, Cynthia Marcotte Stamer. To review the original work, see here.
Solutions Law Press, Inc. invites you to receive future updates by registering here and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy. If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. For specific information about the these or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years working as an on demand, special project, consulting, general counsel or other basis with domestic and international business, charitable, community and government organizations of all types, sizes and industries and their leaders on labor and employment and other workforce compliance, performance management, internal controls and governance, compensation and benefits, regulatory compliance, investigations and audits, change management and restructuring, disaster preparedness and response and other operational, risk management and tactical concerns.
Most widely recognized for her work with health care, life sciences, insurance and data and technology organizations, she also has worked extensively with health plan and insurance, employee benefits, financial, transportation, manufacturing, energy, real estate, accounting and other services, public and private academic and other education, hospitality, charitable, civic and other business, government and community organizations. and their leaders.
Ms. Stamer has extensive experience advising, representing, defending, and training domestic and international public and private business, charitable, community and governmental organizations and their leaders, employee benefit plans, their fiduciaries and service providers, insurers, and others has published and spoken extensively on these concerns. As part of these involvements, she has worked, published and spoken extensively on these and other human resources, employee benefits, compensation, worker classification and other workforce and other services; insurance; health care; workers’ compensation and occupational disease; business reengineering, disaster and distress; and many other performance, risk management, compliance, public policy and regulatory affairs, and other operational concerns.
A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally and domestically as an advisor to business, community and government leaders on these and other legislative, regulatory and other legislative and regulatory design, drafting, interpretation and enforcement, as well as regularly advises and represents organizations on the design, administration and defense of workforce, employee benefit and compensation, safety, discipline, reengineering, regulatory and operational compliance and other management practices and actions.
Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and provides insights and thought leadership through her extensive publications, public speaking and volunteer service with a diverse range of organizations including as Chair of the American Bar Association (“ABA”) Intellectual Property Section Law Practice Management Committee, Vice Chair of the International Section Life Sciences and Health Committee, Past ABA RPTE Employee Benefits & Other Compensation Group Chair and Council Representative and current Welfare Benefit Committee Co-Chair, Past Chair of the ABA Managed Care & Insurance Interest Group, past Region IV Chair and national Society of Human Resources Management Consultant Forum Board Member, past Texas Association of Business BACPAC Chair, Regional Chair and Dallas Chapter Chair, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation and many others.
For more information about these concerns or Ms. Stamer’s work, experience, involvements, other publications, or programs, see www.cynthiastamer.com, on Facebook, on LinkedIn or Twitter or e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns.
©2021 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™
Businesses Face Increased Wage Costs & Risks From American Rescue Plan Act Of 2021 FLSA Minimum Wage Changes
March 2, 2021U.S businesses will face sharply increased wage costs if Senate Democrats succeed in their plan to pass as soon as this week the American Rescue Plan Act of 2021 (the “Act”) passed by the House of Representatives on Friday, February 24, 2021.
One of many provisions impacting employers and their employee benefit plans in the Act that Congressional Democrats are pushing through as a COVID-19 relief package, Section 2101 of the Act amends the Fair Labor Standards Act of 1938 (“FLSA”) to increase immediately upon enactment the federal minimum wage employers covered by the FLSA must pay to most non-exempt employees (“regular rate”) by $2.25 per hour from the current rate of $7.25 to $9.50 per hour, then provides for additional annual increases the gradual increase of the federal minimum wage that will raise the regular rate to $15.00 per hour over the next four years. Beginning in 2026, the Act also provides for annual increases in the regular rate based on the median hourly wage of all employees as determined by the Bureau of Labor Statistics rounded up to the nearest multiple of $0.05. This means the regular minimum wage employers must pay most hourly employees would more than double by 2025 and continue to increase thereafter.
In addition, the Act also phases out current rules allowing employers to pay tipped employees, new employees under age 20 and handicapped employees less than the regular minimum wage over the next five years and raises the minimum wage the FLSA allows employers to pay those employees gradually over the intervening period, with the initial increases slated to take effect upon enactment.
As Senate Majority Leader Chuck Schumer has announced plans to bring the Act before the Senate for a vote as early as this week and President Biden committed to promptly sign the Act that is the centerpiece of the Democrats latest COVID-19 relief package, businesses are likely to feel the impact of the increased minimum wage and other mandates within days if not by month’s end.
These amendments will directly and immediately increase labor costs for non-exempt workers as well as employee benefit and fringe benefit costs and obligations tied to compensation or based on FLSA classifications. Other Biden-Harris Administration policies expanding the scope of the FLSA and other federal laws through revisions and enforcement of rules for characterizing workers as employees rather than independent contractors and enforcing expansive joint employer liability rules as well as other announced or expected Biden-Harris Administration proworker regulatory and enforcement changes almost certainly will expand the reach and implications of these changes. The Biden-Harris Administration’s January 20, 2021 Memorandum on Regulatory Freeze Pending Review suspended the implementation of the Trump Administration led Labor Department’s Final Rule: Independent Contractor Status under the Fair Labor Standards Act slated to take effect on March 8, 2021, which sought to restore and clarify historical more employer friendly policies for distinguishing employee versus independent contractor relationships for purposes of the FLSA, the WHD’s withdrawal of previously issued Trump Administration era opinions that applied that Administration’s more expansive view of independent contractor status, and WHD’s issuance of new opinions articulating and apply applying significantly narrower definitions of independent contractor and broader definitions of employees.
Based on the agenda announced by the Biden-Harris Administration, businesses also should expect the Biden-Harris Administration and private plaintiffs to use these more employee friendly interpretation and enforcement policies to attack employer characterizations of workers as contractors to justify nonpayment of minimum wage and overtime to those workers. Along with being forced to pay unpaid wages and overtime with interest, businesses unsuccessful in defending their worker classification characterizations can expect to face liquidated damage awards to private litigants equal to two times the amount of the back pay liability or in the case of WHD enforcement for repeated or willful violations, civil monetary penalties.
In assessing and managing these risks, businesses should evaluate their potential joint employer exposure to liability for unpaid minimum wage and overtime violations by other businesses providing labor or other services as the Biden-Harris Administration also is expected to seek to apply the much more expansive interpretation of joint employment applied during the Obama Administration abandoned during the Trump Administration.
These misclassification mistakes can be particularly costly. FLSA liabilities arising from misclassification of workers as independent contractors carry significant risk both because businesses often fail to pay required minimum wages or overtime as well as don’t keep required time records. The Biden-Harris Administration has made clear that it plans to move quickly to reimplement the regulatory and enforcement practices used during the Obama Administration to aggressively challenge employers’ characterization of workers as exempt from the FLSA’s minimum wage and overtime rules as independent contractors.
Considering these developments, all U.S. businesses and business leaders are well-advised both to begin preparing to comply with anticipated increases in federal minimum wage rates, as well as well as assess and take appropriate steps to mitigate their exposure to anticipated aggressive efforts to reclassify service providers considered to perform work as independent contractors, as contractors or employees of subcontractors or other businesses or both.
More Information
The FLSA reforms are only one of a number of provisions of the Act impacting employers and their employee benefit plans. For more a more comprehensive discussion of the FLSA amendments included in the Act, see here.
Solutions Law Press, Inc. also invites you receive future updates by registering here and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy. If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. For specific information about the these or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years working as an on demand, special project, consulting, general counsel or other basis with domestic and international business, charitable, community and government organizations of all types, sizes and industries and their leaders on labor and employment and other workforce compliance, performance management, internal controls and governance, compensation and benefits, regulatory compliance, investigations and audits, change management and restructuring, disaster preparedness and response and other operational, risk management and tactical concerns.
Most widely recognized for her work with workforce, health care, life sciences, insurance and data and technology organizations, she also has worked extensively with health plan and insurance, employee benefits, financial, transportation, manufacturing, energy, real estate, accounting and other services, public and private academic and other education, hospitality, charitable, civic and other business, government and community organizations. and their leaders.
Ms. Stamer has extensive experience advising, representing, defending and training domestic and international public and private business, charitable, community and governmental organizations and their leaders, employee benefit plans, their fiduciaries and service providers, insurers, and others has published and spoken extensively on these concerns. As part of these involvements, she has worked, published and spoken extensively on these and other federal and state wage and hour and other compensation, discrimination, performance management, and other related human resources, employee benefits and other workforce and services; insurance; workers’ compensation and occupational disease; business reengineering, disaster and distress; and many other risk management, compliance, public policy and performance concerns.
A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally and domestically as an advisor to business, community and government leaders on these and other legislative, regulatory and other legislative and regulatory design, drafting, interpretation and enforcement, as well as regularly advises and represents organizations on the design, administration and defense of workforce, employee benefit and compensation, safety, discipline, reengineering, regulatory and operational compliance and other management practices and actions.
Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and provides insights and thought leadership through her extensive publications, public speaking and volunteer service with a diverse range of organizations including as Chair of the American Bar Association (“ABA”) Intellectual Property Section Law Practice Management Committee, Vice Chair of the International Section Life Sciences and Health Committee, Past ABA RPTE Employee Benefits & Other Compensation Group Chair and Council Representative and current Welfare Benefit Committee Co-Chair, Past Chair of the ABA Managed Care & Insurance Interest Group, past Region IV Chair and national Society of Human Resources Management Consultant Forum Board Member, past Texas Association of Business BACPAC Chair, Regional Chair and Dallas Chapter Chair, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation and many others.
For more information about these concerns or Ms. Stamer’s work, experience, involvements, other publications, or programs, see www.cynthiastamer.com or contact Ms. Stamer via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns.
©2021 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™
To 2/18 Complimentary Update On Proposed COVID Relief Provisions Impacting Employers & Employee Benefit Plans
February 12, 2021
Solutions Law Press, Inc.™ invites employers, employee benefit plan fiduciaries and vendors and other impacted business leaders participate in a complimentary briefing on the employer and employee benefit requirements of the H.R. 6379, Take Responsibility for Workers and Families Act as approved by the Ways & Means Committee as of February 12, 2021. The live Zoom briefing now will begin at 9:00 a.m. Central Time on Thursday, February 18, 2021 to avoid potential weather-related power and other disruptions associated with winter storms at its originally scheduled presentation time on Monday, February 15.
Employers and employee benefit plan fiduciaries and vendors should get up to speed on a new mandate to subsidize health coverage continuation and other requirements of the Act that the House Ways & Means Committee voted on February 11, 2021 to include in the lasted COVID-19 relief package the Democrat Majority plans to fast track through Congress. By the end of February if not before, Congress is expected to pass a final COVID-19 relief package including these employer and employee benefit plan mandates in substantially the same form as approved by the Ways and Means Committee. As these provisions will require quick action by employers and plans, employers, employee benefit plans, their fiduciaries and plan vendors should begin preparing now to comply with the anticipated new requirements
Registration & Program Details
Solutions Law Press, Inc. will host the 30-minute Zoom briefing beginning at 9:00 a.m. Central Time on Thursday, February 18, 2021 on the current provisions of the Act. The briefing will be conducted attorney Cynthia Marcotte Stamer. Participation is complimentary, but space is limited. Accordingly, registration is required and registration and participation will be granted on a first come, first serve basis here.
About Presenter Cynthia Marcotte Stamer
A Fellow in the American College of Employee Benefits Counsel, Board Certified in Labor and Employment Law by the Texas Board of Legal Specialization and recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney, 30+ years working as an on demand, special project, consulting, general counsel or other basis with domestic and international business, employee benefit plan, health care, insurance, financial service, charitable, community and government organizations of all types, sizes and industries and their leaders on labor and employment and other workforce, employee benefits and compensation, performance management, internal controls, governance, regulatory and operational compliance, investigations and audits, change management and restructuring, disaster preparedness and response and other operational, risk management and tactical concerns. Best known for her leading edge work and thought leadership on workforce management and reengineering and health and other employee benefits concerns, Ms. Stamer regularly advises and represents organizations on the design, administration and defense of workforce, employee benefit and compensation, safety, discipline, reengineering, regulatory and operational compliance and other management practices and actions. Along with advising and representing management organizations, Ms. Stamer also has worked continuously throughout her career internationally and domestically as an advisor to business, community and government leaders on health care, savings and retirement, workforce, and other legislative and regulatory design, drafting, interpretation, enforcement and other domestic and international public policy.
Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and provides insights and thought leadership through her extensive publications, public speaking and volunteer service with a diverse range of organizations including as Chair of the American Bar Association (“ABA”) Intellectual Property Section Law Practice Management Committee, Vice Chair of the International Section Life Sciences and Health Committee, Past ABA RPTE Employee Benefits & Other Compensation Group Chair and Council Representative and current Welfare Benefit Committee Co-Chair, Past Chair of the ABA Managed Care & Insurance Interest Group, past Region IV Chair and national Society of Human Resources Management Consultant Forum Board Member, past Texas Association of Business BACPAC Chair, Regional Chair and Dallas Chapter Chair, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation and many others.
For more information about these concerns or Ms. Stamer’s work, experience, involvements, other publications, or programs, see www.cynthiastamer.com or contact Ms. Stamer via e-mailhere.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy Group.
Ways & Means Committee Approves New COVID Relief Employer COBRA Subsidy Mandate
February 11, 2021Register For 2/15 Zoom Briefing
Register For 2/15 Zoom Briefing
Employers and employee benefit plan fiduciaries and vendors should prepare to face a new mandate to subsidize health coverage continuation and other requirements included in the H.R. 6379, Take Responsibility for Workers and Families Act that the House Ways & Means Committee approved for inclusion in the COVID-19 relief package the Democrat Majority plans to fast track to enactment.
The proposed COBRA subsidy mandate is one of several COVID-19 relief provisions impacting employers and their benefit programs the Ways & Means Committee marked up and reported out of committee the week ending February 12, 2021. Other provisions include:
- Additional direct assistance that would increase the COVID direct payment for qualifying working families by an additional direct payment of $1,400 per person, bringing their total relief to $2,000 per person;
- Extend temporary federal unemployment and benefits with increased weekly benefits;
- Significantly enhanced Earned Income Tax Credits for workers without children;
- Raising the Child Tax Credit to $3,000 per child ($3,600 for children under 6), and makes it fully refundable and advanceable;
- Expanding the Child and Dependent Tax Credit (CDCTC) to allow families to claim up to half of their child care expenses;
- Reducing health care premiums for low- and middle-income families by increasing the Affordable Care Act’s (ACA) premium tax credits for 2021 and 2022;
- Creating health care subsidies for unemployed workers who are ineligible for COBRA;
- A program to bail out insolvent and distressed multiemployer (union) pension plans; and
- More.
Revised legislative language of these and other proposals before the Ways and Means Committee markup this week is emerging and could face further changes as Congressional Democrats continue to work to enact their latest COVID-Relief package. Employers and employee benefit leaders and advisors should monitor carefully and begin preparing to respond to these proposals.
Register & Attend Complimentary 2/15 Briefing
Solutions Law Press, Inc. will host the 30-minute Zoom briefing beginning at 9:00 a.m. Central Time on Monday, February 15, 2020 on the current provisions of the Act. The briefing will be conducted attorney Cynthia Marcotte Stamer. Participation is complimentary, but space is limited. Accordingly, registration is required and registration and participation will be granted on a first come, first serve basis here.
For more information contact the author of this update, Texas Board of Legal Specialization Board Certified Labor and Employment Lawyer, Cynthia Marcotte Stamer here.
More Information
We hope this update is helpful. For more information about the these or other health or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years working as an on demand, special project, consulting, general counsel or other basis with domestic and international business, charitable, community and government organizations of all types, sizes and industries and their leaders on labor and employment and other workforce compliance, performance management, internal controls and governance, compensation and benefits, regulatory compliance, investigations and audits, change management and restructuring, disaster preparedness and response and other operational, risk management and tactical concerns.
Most widely recognized for her work with health care, life sciences, insurance and data and technology organizations, she also has worked extensively with health plan and insurance, employee benefits, financial, transportation, manufacturing, energy, real estate, accounting and other services, public and private academic and other education, hospitality, charitable, civic and other business, government and community organizations. and their leaders.
Ms. Stamer has extensive experience advising, representing, defending and training domestic and international public and private business, charitable, community and governmental organizations and their leaders, employee benefit plans, their fiduciaries and service providers, insurers, and others has published and spoken extensively on these concerns. As part of these involvements, she has worked, published and spoken extensively on these and federal and state discrimination, affirmative action and accommodation and other related human resources, employee benefits and other workforce and services; insurance; workers’ compensation and occupational disease; business reengineering, disaster and distress; and many other risk management and compliance concerns.
A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally and domestically as an advisor to business, community and government leaders on these and other legislative, regulatory and other legislative and regulatory design, drafting, interpretation and enforcement, as well as regularly advises and represents organizations on the design, administration and defense of workforce, employee benefit and compensation, safety, discipline, reengineering, regulatory and operational compliance and other management practices and actions.
Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and provides insights and thought leadership through her extensive publications, public speaking and volunteer service with a diverse range of organizations including as Chair of the American Bar Association (“ABA”) Intellectual Property Section Law Practice Management Committee, Vice Chair of the International Section Life Sciences and Health Committee, Past ABA RPTE Employee Benefits & Other Compensation Group Chair and Council Representative and current Welfare Benefit Committee Co-Chair, Past Chair of the ABA Managed Care & Insurance Interest Group, past Region IV Chair and national Society of Human Resources Management Consultant Forum Board Member, past Texas Association of Business BACPAC Chair, Regional Chair and Dallas Chapter Chair, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation and many others.
For more information about these concerns or Ms. Stamer’s work, experience, involvements, other publications, or programs, see www.cynthiastamer.com or contact Ms. Stamer via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns.
Solutions Law Press, Inc. invites you receive future updates by registering here and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy. If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. ©2021 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™
Prepare To Respond To Biden-Harris Plan To Beat COVID-19 & Other Administration Policy & Enforcement Priorities
January 21, 2021Newly sworn in President Joe Biden chose to make an executive order outlining the core principles for his Administration’s policy for fighting COVID-19 the first signed in his new Administration shortly after he was sworn in as President as well as made public the Biden-Harris Administration’s other key policy priorities upon taking office which promise to significantly impact business and other organizations, taxpayers and others. As the Administration and new Congress get to work on these and other policies, American businesses and citizens should stay informed and provide clear and consistent input to the Administration and members of Congress about the policy and enforcement proposals and actions to help shape the law and prepare to deal with the new rules and priorities.
Key Biden-Harris Administration Policy Priorities
President Biden will deliver bold action and immediate relief for American families as the country grapples with converging crises. This will include actions to control the COVID-19 pandemic, provide economic relief, tackle climate change, and advance racial equity and civil rights, as well as immediate actions to reform our immigration system and restore America’s standing in the world.
COVID-19
President Biden will move quickly to contain the COVID-19 crisis by expanding testing, safely reopening schools and businesses, and taking science-driven steps to address the communities — especially communities of color — who have been hardest hit by this virus. And, President Biden will launch a national vaccination program to inoculate the U.S. population efficiently and equitably.
Read more about the Biden-Harris plan to beat COVID-19 [See below].
Climate
President Biden will take swift action to tackle the climate emergency. The Biden Administration will ensure we meet the demands of science, while empowering American workers and businesses to lead a clean energy revolution.
Racial Equity
The promise of our nation is that every American has an equal chance to get ahead, yet persistent systemic racism and barriers to opportunity have denied this promise for so many. President Biden is putting equity at the center of the agenda with a whole of government approach to embed racial justice across Federal agencies, policies, and programs. And President Biden will take bold action to advance a comprehensive equity agenda to deliver criminal justice reform, end disparities in healthcare access and education, strengthen fair housing, and restore Federal respect for Tribal sovereignty, among other actions, so that everyone across America has the opportunity to fulfill their potential.
Economy
President Biden will take bold steps to address the inequities in our economy and provide relief to those who are struggling during the COVID-19 pandemic. The President will also work with Congress to pass the American Rescue Plan to change the course of the pandemic, build a bridge towards economic recovery, and invest in racial justice. And, he will build our economy back better from the pandemic and create millions of jobs by strengthening small businesses and investing in the jobs of the future.
Health Care
President Biden will make a renewed commitment to protect and expand Americans’ access to quality, affordable health care. He will build on the Affordable Care Act to meet the health care needs created by the pandemic, reduce health care costs, and make our health care system less complex to navigate.
Immigration
President Biden will reform our long-broken and chaotic immigration system. President Biden’s strategy is centered on the basic premise that our country is safer, stronger, and more prosperous with a fair and orderly immigration system that welcomes immigrants, keeps families together, and allows people across the country—both newly arrived immigrants and people who have lived here for generations—to more fully contribute to our country.
Restoring America’s Global Standing
President Biden will take steps to restore America’s standing in the world, strengthening the U.S. national security workforce, rebuilding democratic alliances across the globe, championing America’s values and human rights, and equipping the American middle class to succeed in a global economy.
COVID-19 Plan To Beat COVID-19
The first Executive Order signed by President Biden in furtherance of these initiatives was his COVID-19: The Biden-Harris plan to beat COVID-19 Executive Oder, the text of which reads as follows:
The American people deserve an urgent, robust, and professional response to the growing public health and economic crisis caused by the coronavirus (COVID-19) outbreak. President Biden believes that the federal government must act swiftly and aggressively to help protect and support our families, small businesses, first responders, and caregivers essential to help us face this challenge, those who are most vulnerable to health and economic impacts, and our broader communities – not to blame others or bail out corporations.
The Biden-Harris administration will always:
Listen to science
Ensure public health decisions are informed by public health professionals
Promote trust, transparency, common purpose, and accountability in our government
President Biden and Vice President Harris have a seven-point plan to beat COVID-19.
Ensure all Americans have access to regular, reliable, and free testing.
Double the number of drive-through testing sites.
Invest in next-generation testing, including at home tests and instant tests, so we can scale up our testing capacity by orders of magnitude.
Stand up a Pandemic Testing Board like Roosevelt’s War Production Board. It’s how we produced tanks, planes, uniforms, and supplies in record time, and it’s how we will produce and distribute tens of millions of tests.
Establish a U.S. Public Health Jobs Corps to mobilize at least 100,000 Americans across the country with support from trusted local organizations in communities most at risk to perform culturally competent approaches to contact tracing and protecting at-risk populations.
Fix personal protective equipment (PPE) problems for good.
President Biden is taking responsibility and giving states, cities, tribes, and territories the critical supplies they need.
Fully use the Defense Production Act to ramp up production of masks, face shields, and other PPE so that the national supply of personal protective equipment exceeds demand and our stores and stockpiles — especially in hard-hit areas that serve disproportionately vulnerable populations — are fully replenished.
Build immediately toward a future, flexible American-sourced and manufactured capability to ensure we are not dependent on other countries in a crisis.
Provide clear, consistent, evidence-based guidance for how communities should navigate the pandemic – and the resources for schools, small businesses, and families to make it through.
Social distancing is not a light switch. It is a dial. President Biden will direct the CDC to provide specific evidence-based guidance for how to turn the dial up or down relative to the level of risk and degree of viral spread in a community, including when to open or close certain businesses, bars, restaurants, and other spaces; when to open or close schools, and what steps they need to take to make classrooms and facilities safe; appropriate restrictions on size of gatherings; when to issue stay-at-home restrictions.
Establish a renewable fund for state and local governments to help prevent budget shortfalls, which may cause states to face steep cuts to teachers and first responders.
Call on Congress to pass an emergency package to ensure schools have the additional resources they need to adapt effectively to COVID-19.
Provide a “restart package” that helps small businesses cover the costs of operating safely, including things like plexiglass and PPE.
Plan for the effective, equitable distribution of treatments and vaccines — because development isn’t enough if they aren’t effectively distributed.
Invest $25 billion in a vaccine manufacturing and distribution plan that will guarantee it gets to every American, cost-free.
Ensure that politics plays no role in determining the safety and efficacy of any vaccine. The following 3 principles will guide the Biden-Harris administration: Put scientists in charge of all decisions on safety and efficacy; publicly release clinical data for any vaccine the FDA approves; and authorize career staff to write a written report for public review and permit them to appear before Congress and speak publicly uncensored.
Ensure everyone — not just the wealthy and well-connected — in America receives the protection and care they deserve, and consumers are not price gouged as new drugs and therapies come to market.
Protect older Americans and others at high risk.
President Biden understands that older Americans and others at high-risk are most vulnerable to COVID-19.
Establish a COVID-19 Racial and Ethnic Disparities Task Force, as proposed by Vice President Harris, to provide recommendations and oversight on disparities in the public health and economic response. At the end of this health crisis, it will transition to a permanent Infectious Disease Racial Disparities Task Force.
Create the Nationwide Pandemic Dashboard that Americans can check in real-time to help them gauge whether local transmission is actively occurring in their zip codes. This information is critical to helping all individuals, but especially older Americans and others at high risk, understand what level of precaution to take.
Rebuild and expand defenses to predict, prevent, and mitigate pandemic threats, including those coming from China.
Immediately restore the White House National Security Council Directorate for Global Health Security and Biodefense, originally established by the Obama-Biden administration.
Immediately restore our relationship with the World Health Organization, which — while not perfect — is essential to coordinating a global response during a pandemic.
Re-launch and strengthen U.S. Agency for International Development’s pathogen-tracking program called PREDICT.
Expand the number of CDC’s deployed disease detectives so we have eyes and ears on the ground, including rebuilding the office in Beijing.
Implement mask mandates nationwide by working with governors and mayors and by asking the American people to do what they do best: step up in a time of crisis.
Experts agree that tens of thousands of lives can be saved if Americans wear masks. President Biden will continue to call on:
Every American to wear a mask when they are around people outside their household.
Every Governor to make that mandatory in their state.
Local authorities to also make it mandatory to buttress their state orders.
Once we succeed in getting beyond this pandemic, we must ensure that the millions of Americans who suffer long-term side effects from COVID don’t face higher premiums or denial of health insurance because of this new pre-existing condition. The Biden-Harris Administration will work to ensure that the protections for those with pre-existing conditions that were won with Obamacare are protected. And, they will work to lower health care costs and expand access to quality, affordable health care through a Medicare-like public option.
Monitor & Respond To Emerging Developments & Proposals
As the new Administration and Congress get down to work, all U.S. organizations and communities, their leaders, and individual employees and citizens should carefully follow, and share their input to the Administration, members of Congress, and other federal, state and local officials on the actions and proposals taken to implement this and other policy that impact their interests.
More Information
We hope this update is helpful. For more information about the these or other health or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is nationally recognized for her work and thought leadership on health and other health and employee benefit issues.
An attorney board certified in labor and employment law by the Texas Board of Legal Specialization and Fellow in the American College of Employee Benefit Counsel, Ms. Stamer has worked as an on demand, special project, consulting, general counsel or other basis with health and other employee benefit plans, their sponsors, insurers, administrators, providers and others and others has published and spoken extensively on these concerns.
A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally and domestically as an advisor and advocate for employer and other plan sponsors, fiduciaries, administrators, insurers, technology and other service providers, managed care organizations, direct primary care and other health care providers and others on these and other legislative, regulatory and other legislative and regulatory design, drafting, interpretation and enforcement, as well as regularly advises and represents organizations on the design, administration and defense of workforce, employee benefit and compensation, safety, discipline, reengineering, regulatory and operational compliance and other management practices and actions.
Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and provides insights and thought leadership through her extensive publications, public speaking and volunteer service with a diverse range of organizations including as Chair of the American Bar Association (“ABA”) Intellectual Property Section Law Practice Management Committee, Vice Chair of the International Section Life Sciences and Health Committee, Past ABA RPTE Employee Benefits & Other Compensation Group Chair and Council Representative and current Welfare Benefit Committee Co-Chair, Past Chair of the ABA Managed Care & Insurance Interest Group, past Region IV Chair and national Society of Human Resources Management Consultant Forum Board Member, past Texas Association of Business BACPAC Chair, Regional Chair and Dallas Chapter Chair, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation and many others.
For more information about these concerns or Ms. Stamer’s work, experience, involvements, other publications, or programs, see www.cynthiastamer.com or contact Ms. Stamer via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- Employers Sponsoring Health Plans Should Audit Compliance Now To Avoid Excise Tax, Other Liability
- Guard Against COVID-19 Fraud Scams
- Proposed Privacy Rules Grant Health Plans New Flexibility, Add New Obligations
- Kickin’ COVID-19: Reopening Texas Summit October 8 On Facebook Live
- Employer Option To Defer Paying Some Employee Payroll Taxes Until 2021
- Free CDC COVID-19 Communication Resources
- DOL Invests $80.6 million in Apprenticeship Expansion Grants
- Businesses Should Confirm Using Benefits, Meeting Mandates Of Special COVID-19 Tax Rules
- Ezekiel Elliott COVID-19 Diagnosis Disclosure Outrage Highlights Need To Handle COVID-19 & Other Medical Information With Care
- Proposed Regulations Would Treat Direct Primary Care and Health Care Sharing Ministries Membership Dues As Qualifying Medical Expenses For Medical Deduction & HSA Reimbursement Purposes
- Wish Tax Guidance Were Clearer? Tell IRS/Treasury Your Suggested Topics For 2020-2021 Treasury Priority Guidance Plan
- New IRS Increased Health FSA Carryover, Gives COVID Health FSA Election Relief
- IRS Shares Initial CARES Act Plan Loan & Distribution Relief Guidance
- Employer Sponsors & Health Plans Face Rising Risk From Mental Health & Substance Abuse Coverage Violations
- Use Prudent Process To Manage Workforce & Other Business Changes To Help Minimize Business & Management Liabilities & Protect Future Recovery
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. ©2021 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™
Employers Sponsoring Health Plans Should Audit Compliance Now To Avoid Excise Tax, Other Liability
January 11, 2021Employers with more than 49 employees sponsoring health coverage should audit their 2020 health plan administration to confirm compliance with 40 federal requirements that if violated trigger an employer duty to pay excise taxes under Internal Revenue Code (“IRC”) Section 6939D if not caught and corrected before the original due date of the employer’s tax return along with other liabilities arising from those violations under the Employee Retirement Income Security Act (“ERISA”).
IRC Section 6039D requires an employer with 50 employees that sponsors a health plan to self report, self assess and pay excise tax penalties for those violations not caught and corrected before the original due date of businesses’ 2020 business tax return in addition to any benefit, fiduciary and other liabilities triggered for the plan and its fiduciaries under ERISA. The excise tax triggering violations include most Patient Protection and Affordable Care (“Obama Care”) adverse benefit determination and coverage requirements, the eligibility and nondiscrimination requirements of the Health Insurance Portability & Accountability Act (“HIPAA”), mental health parity, Consolidated Omnibus Reconciliation Act (“COBRA”) medical coverage continuation and others.
Employers should take well documented actions to audit compliance rather than presume the proper administration of their programs now to allow sufficient time to take corrective action before their original 2020 business tax filing deadline. While employers often are temped to presume or rely upon unaudited assurance from their insurer or third party administrator, sanctions imposed against major insurers by various regulatory agencies, complaints filed with the Department of Labor and state insurance departments and other audits reveal errors in administration frequently happen. Special COVID-19 rules and relief issued in response to the COVID-19 health care emergency enhance the likelihood of administrative errors during 2020. Given sensitive time deadlines and the information, employers ideally will want to complete this audit within the scope of attorney-client privilege sufficiently in advance of the earlier of the original due date of their business tax return or for self-insured health plans, the end of the stop loss run out period to allow sufficient time for necessary correction or other response. Paragraph
For more information about these or other employee benefit, heath and managed care, insurance or workforce issues, register and participate in the January Solutions Law Press, Inc. briefing on the 40 federal health plan rules covered by IRC Section 6039D e-mail the author of this update, attorney Cynthia Marcotte Stamer.
More Information
We hope this update is helpful. For more information about the these or other health or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is nationally recognized for her work and thought leadership on health and other health and employee benefit issues.
An attorney board certified in labor and employment law by the Texas Board of Legal Specialization and Fellow in the American College of Employee Benefit Counsel, Ms. Stamer has worked as an on demand, special project, consulting, general counsel or other basis with health and other employee benefit plans, their sponsors, insurers, administrators, providers and others and others has published and spoken extensively on these concerns.
A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally and domestically as an advisor and advocate for employer and other plan sponsors, fiduciaries, administrators, insurers, technology and other service providers, managed care organizations, direct primary care and other health care providers and others on these and other legislative, regulatory and other legislative and regulatory design, drafting, interpretation and enforcement, as well as regularly advises and represents organizations on the design, administration and defense of workforce, employee benefit and compensation, safety, discipline, reengineering, regulatory and operational compliance and other management practices and actions.
Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and provides insights and thought leadership through her extensive publications, public speaking and volunteer service with a diverse range of organizations including as Chair of the American Bar Association (“ABA”) Intellectual Property Section Law Practice Management Committee, Vice Chair of the International Section Life Sciences and Health Committee, Past ABA RPTE Employee Benefits & Other Compensation Group Chair and Council Representative and current Welfare Benefit Committee Co-Chair, Past Chair of the ABA Managed Care & Insurance Interest Group, past Region IV Chair and national Society of Human Resources Management Consultant Forum Board Member, past Texas Association of Business BACPAC Chair, Regional Chair and Dallas Chapter Chair, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation and many others.
For more information about these concerns or Ms. Stamer’s work, experience, involvements, other publications, or programs, see www.cynthiastamer.com or contact Ms. Stamer via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- Guard Against COVID-19 Fraud Scams
- Proposed Privacy Rules Grant Health Plans New Flexibility, Add New Obligations
- Kickin’ COVID-19: Reopening Texas Summit October 8 On Facebook Live
- Employer Option To Defer Paying Some Employee Payroll Taxes Until 2021
- Free CDC COVID-19 Communication Resources
- DOL Invests $80.6 million in Apprenticeship Expansion Grants
- Businesses Should Confirm Using Benefits, Meeting Mandates Of Special COVID-19 Tax Rules
- Ezekiel Elliott COVID-19 Diagnosis Disclosure Outrage Highlights Need To Handle COVID-19 & Other Medical Information With Care
- Proposed Regulations Would Treat Direct Primary Care and Health Care Sharing Ministries Membership Dues As Qualifying Medical Expenses For Medical Deduction & HSA Reimbursement Purposes
- Wish Tax Guidance Were Clearer? Tell IRS/Treasury Your Suggested Topics For 2020-2021 Treasury Priority Guidance Plan
- New IRS Increased Health FSA Carryover, Gives COVID Health FSA Election Relief
- IRS Shares Initial CARES Act Plan Loan & Distribution Relief Guidance
- Employer Sponsors & Health Plans Face Rising Risk From Mental Health & Substance Abuse Coverage Violations
- Use Prudent Process To Manage Workforce & Other Business Changes To Help Minimize Business & Management Liabilities & Protect Future Recovery
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. ©2021 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™
Religious Organizations May Enjoy New Flexibility Under OFCCP Final Religious Exemption Regulation
January 11, 2021Federal contractors or subcontractors (“government contractors”) that consider themselves religious organizations may wish to reevaluate their status as religious organizations and other implications of the new U.S. Department of Labor’s Office of Federal Contract Compliance Programs (OFCCP) Final Rule “Implementing Legal Requirements Regarding the Equal Opportunity Clause’s Religious Exemption” (“Final Rule”) that took effect January 8, 2020 while keeping a close eye out for further modifications or refinement to the rules by the incoming Biden Administration and the courts.
Executive Order 11246, Section 503 of the Rehabilitation Act of 1973 and the Vietnam Era Veterans’ Readjustment Assistance Act of 1974, as amended, generally prohibit federal contractors to discriminate in employment because of race, color, religion, sex, sexual orientation, gender identity, national origin, disability, or status as a protected veteran. In addition, contractors and subcontractors are prohibited from discriminating against applicants or employees because they have inquired about, discussed, or disclosed their compensation or the compensation of others subject to certain limitations, and may not retaliate against applicants or employees for engaging in protected activities. These laws also require that federal contractors provide equal employment opportunity through affirmative action and report data about their employment practices.
While generally prohibiting religious discrimination in employment, Executive Order 11246, also acknowledges Constitutional religious freedom protections by providing religious organizations may prefer in employment “individuals of a particular religion,” to maintain their religious identity and integrity. The Final Rule announced by the Trump Administration on December 7, 2020 does not change the vast majority of federal contractors’ responsibilities to comply with their equal employment opportunity and affirmative action obligations under Executive Order 11246. However, it does seek to clarify and maximize the legal protection of religious exercise permitted by the Constitution and law taking into account the Religious Freedom Restoration Act by adding a rule of construction, definitions of key terms and several examples within the definition of “religious corporation, association, educational institution, or society” to better illustrate which organizations may qualify for the religious exemption.
Federal contractors that believe they qualify for coverage by the new Final Rule should document their qualification, keeping in mind that its applicability turns on a highly fact specific, evidence based test. Those relying on the rules should work with experienced legal counsel to evaluate and preserve evidence demonstrating the basis of qualification and other risk management strategies, while simultaneously watching for potential refinements to the rules by the incoming Biden Administration, the courts or both.
For more information about the Final Rule or other federal employment discrimination and affirmative action rules, e-mail the author of this update, Texas Board of Legal Specialization Board Certified Labor and Employment Lawyer, Cynthia Marcotte Stamer.
More Information
We hope this update is helpful. For more information about the these or other health or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years working as an on demand, special project, consulting, general counsel or other basis with domestic and international business, charitable, community and government organizations of all types, sizes and industries and their leaders on labor and employment and other workforce compliance, performance management, internal controls and governance, compensation and benefits, regulatory compliance, investigations and audits, change management and restructuring, disaster preparedness and response and other operational, risk management and tactical concerns.
Most widely recognized for her work with health care, life sciences, insurance and data and technology organizations, she also has worked extensively with health plan and insurance, employee benefits, financial, transportation, manufacturing, energy, real estate, accounting and other services, public and private academic and other education, hospitality, charitable, civic and other business, government and community organizations. and their leaders.
Ms. Stamer has extensive experience advising, representing, defending and training domestic and international public and private business, charitable, community and governmental organizations and their leaders, employee benefit plans, their fiduciaries and service providers, insurers, and others has published and spoken extensively on these concerns. As part of these involvements, she has worked, published and spoken extensively on these and federal and state discrimination, affirmative action and accommodation and other related human resources, employee benefits and other workforce and services; insurance; workers’ compensation and occupational disease; business reengineering, disaster and distress; and many other risk management and compliance concerns.
A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally and domestically as an advisor to business, community and government leaders on these and other legislative, regulatory and other legislative and regulatory design, drafting, interpretation and enforcement, as well as regularly advises and represents organizations on the design, administration and defense of workforce, employee benefit and compensation, safety, discipline, reengineering, regulatory and operational compliance and other management practices and actions.
Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and provides insights and thought leadership through her extensive publications, public speaking and volunteer service with a diverse range of organizations including as Chair of the American Bar Association (“ABA”) Intellectual Property Section Law Practice Management Committee, Vice Chair of the International Section Life Sciences and Health Committee, Past ABA RPTE Employee Benefits & Other Compensation Group Chair and Council Representative and current Welfare Benefit Committee Co-Chair, Past Chair of the ABA Managed Care & Insurance Interest Group, past Region IV Chair and national Society of Human Resources Management Consultant Forum Board Member, past Texas Association of Business BACPAC Chair, Regional Chair and Dallas Chapter Chair, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation and many others.
For more information about these concerns or Ms. Stamer’s work, experience, involvements, other publications, or programs, see www.cynthiastamer.com or contact Ms. Stamer via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- Guard Against COVID-19 Fraud Scams
- Proposed Privacy Rules Grant Health Plans New Flexibility, Add New Obligations
- Kickin’ COVID-19: Reopening Texas Summit October 8 On Facebook Live
- Employer Option To Defer Paying Some Employee Payroll Taxes Until 2021
- Free CDC COVID-19 Communication Resources
- DOL Invests $80.6 million in Apprenticeship Expansion Grants
- Businesses Should Confirm Using Benefits, Meeting Mandates Of Special COVID-19 Tax Rules
- Ezekiel Elliott COVID-19 Diagnosis Disclosure Outrage Highlights Need To Handle COVID-19 & Other Medical Information With Care
- Proposed Regulations Would Treat Direct Primary Care and Health Care Sharing Ministries Membership Dues As Qualifying Medical Expenses For Medical Deduction & HSA Reimbursement Purposes
- Wish Tax Guidance Were Clearer? Tell IRS/Treasury Your Suggested Topics For 2020-2021 Treasury Priority Guidance Plan
- New IRS Increased Health FSA Carryover, Gives COVID Health FSA Election Relief
- IRS Shares Initial CARES Act Plan Loan & Distribution Relief Guidance
- Employer Sponsors & Health Plans Face Rising Risk From Mental Health & Substance Abuse Coverage Violations
- Use Prudent Process To Manage Workforce & Other Business Changes To Help Minimize Business & Management Liabilities & Protect Future Recovery
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. ©2021 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™
Guard Against COVID-19 Fraud Scams
January 8, 2021Businesses should raise their guard and warn employees and other business connections about avoiding potentially fraudulent COVID-19 related scams.
The U.S. Department of Health and Human Services Office of Inspector General is alerting the public about fraud schemes related to the novel coronavirus (COVID-19). Scammers are using telemarketing calls, text messages, social media platforms, and door-to-door visits to perpetrate COVID-19-related scams.
Fraudsters are offering COVID-19 tests, HHS grants, and Medicare prescription cards in exchange for personal details, including Medicare information. However, these services are unapproved and illegitimate.
These scammers use the coronavirus pandemic to benefit themselves, and beneficiaries face potential harm. The personal information collected can be used to fraudulently bill federal health care programs and commit medical identity theft.
Examples of some of these scams include:
- Scammers are using social media to perpetrate COVID-19-related scams. In one major scheme, fraudsters hack social media accounts and send direct messages to beneficiaries while posing as a friend or government employee. The impersonator claims the person is eligible for government grants (citing various reasons like COVID-19, disability, etc.) and urges them to call a phone number to collect the funds. Upon calling, the beneficiary is asked to pay a “processing fee” (using bank account information, gift cards, bitcoin) to receive the grant money. In return, targets of this scam never receive any money, but often large sums of their money are stolen from them. These alleged grants are entirely illegitimate.
- Fraudsters are also continuing to offer COVID-19 tests to Medicare beneficiaries in exchange for personal details, including Medicare information. However, the services are unapproved and illegitimate.
- In another fraud scheme, some medical labs are targeting retirement communities claiming to offer COVID-19 tests, but they are actually drawing blood and billing federal health care programs for medically unnecessary services.
- Also, fraudsters are offering people a $200 Medicare prescription card when no such cards currently exist.
Peter Khaim, 40, and Arkadiy Khaimov, 37, both of Forest Hills, New York, each were charged with one count of conspiracy to commit health care fraud and wire fraud, and one count of conspiracy to commit money laundering. Khaim was separately charged with two counts of concealment money laundering and one count of aggravated identity theft. Khaimov was separately charged with two counts of concealment money laundering.
“These defendants allegedly lined their own pockets by exploiting Medicare flexibilities that were designed to ensure that patients obtained access to needed medications during the COVID-19 crisis,” said Acting Assistant Attorney General Brian C. Rabbitt of the Justice Department’s Criminal Division. “Together with our law enforcement partners, the Criminal Division is working to aggressively identify, investigate, and prosecute scammers who seek to take advantage of the COVID-19 crisis to defraud our public health care programs.”
“As alleged in the indictment, the defendants manipulated information in over a dozen pharmacies to defraud the Medicare program, including by taking advantage of systems that were intended to assist patients during the COVID-19 pandemic, and then went to great lengths to hide their ill-gotten gains through a network of sham companies,” said Acting U.S. Attorney Set D. DuCharme of the Eastern District of New York. “This office and our law enforcement partners are committed to holding accountable those who seek to enrich themselves at the expense of vital taxpayer-funded health care programs upon which so many rely.”
“We allege Mr. Khaim and Khaimov used the COVID-19 pandemic as cover to exploit changes in the Medicare system,” said Acting Director in Charge William F. Sweeney Jr of the FBI’s New York Field Office. “The changes to this program, funded by taxpayers, were put in place to help fellow citizens obtain needed medications during the pandemic, not line the pockets of fraudsters. Those who attempt to illegally profit from our public funded healthcare programs should remember taxpayers also fund courts and jails, and behavior like the type announced today will be met with swift action from the FBI and our law enforcement partners. If you are aware of frauds like the one announced today, please contact us at 1-800-CALL-FBI.”
“Fraudsters who target the Federal health care system attempt to undermine the integrity of programs that serve millions of individuals. When they leverage a public health emergency to perpetrate schemes, their wanton disregard for the programs and beneficiaries is glaringly clear,” said Special Agent in Charge Scott J. Lampert of the U.S. Department of Health and Human Services Office of Inspector General (HHS-OIG). “We are responding aggressively with our law enforcement partners to pursue bad actors and to warn the public about these ongoing scams.”
“The defendants allegedly carried out a $30 million health care fraud and money laundering scheme, siphoning funds meant for patients during the COVID-19 pandemic,” said Special Agent in Charge Jonathan D. Larsen of IRS-Criminal Investigation (IRS-CI). “While Americans across the country are in dire need of medical and financial assistance, the defendants allegedly used the stolen proceeds to purchase real estate and luxury items. IRS-CI and our law enforcement partners will continue to work tirelessly to expose COVID-19 schemes and bring those responsible to justice.”
“This indictment describes allegations of crimes that are especially egregious and caused significant harm to the programs designed to protect the most medically vulnerable, jeopardizing the health of our Medicare system and then using our nation’s financial system to launder proceeds of the fraud,” said Special Agent in Charge Patricia Tarasca of the Federal Deposit Insurance Corporation, Office of Inspector General (FDIC-OIG). “We appreciate the cooperation of our fellow law enforcement partners as we work to identify and investigate fraud of this type.”
According to the indictment, the defendants used COVID-19 emergency override billing codes in order to submit fraudulent claims to Medicare, for which they were allegedly paid over $30 million for expensive cancer medication Targretin Gel 1% that, in fact, never was purchased by the pharmacies, prescribed by physicians, or dispensed to patients, often during periods when pharmacies were non-operational, and using doctors’ names on prescriptions without their permission.
The indictment alleges that the defendants acquired control over dozens of New York pharmacies by paying others to pose as the owners of the pharmacies and hiring pharmacists to pretend to be supervising pharmacists at the pharmacies, for the purpose of obtaining pharmacy licenses and insurance plan credentialing. As the effects of the COVID-19 pandemic began to be felt in the United States, the defendants used the COVID-19 pandemic as an opportunity to capitalize on a national emergency for their own financial gain by using the COVID-19 “emergency override” billing codes to submit fraudulent claims for Targretin Gel 1%, which has an average wholesale price of approximately $34,000 for each 60 gram tube.
The indictment also alleges that, with the proceeds of the fraud, the defendants engaged in a complex money laundering conspiracy where they created sham pharmacy wholesale companies, which they named after pre-existing pharmacy wholesalers, and fabricated invoices to make it appear that funds transferred from the pharmacies to the sham pharmacy wholesale companies were for legitimate pharmaceutical drug purchases.
In the first phase of the money laundering conspiracy, the defendants conspired with an international money launderer who arranged for funds to be wired from the sham pharmacy wholesale companies to companies in China for distribution to individuals in Uzbekistan. In exchange, the defendants received cash provided by members of the Uzbekistani immigrant community to an unlicensed money transfer business for remittance to their relatives in Uzbekistan, minus a commission that was deducted by the money launderer.
In the second phase of the money laundering conspiracy, when the amount of fraudulent proceeds exceeded the amount of cash available in the Uzbekistani immigrant community, the defendants directed the international money launderer to transfer funds back from the sham wholesale companies to the defendants, their relatives, or their designess, in the form of certified cashier’s checks and bags of cash that were dropped at their house in the middle of the night. The defendants used the proceeds of the scheme to purchase real estate and other luxury items.
Protect Yourself
Businesses should protect themselves and warn their employees to guard against these and other scams. Recommended steps include:
- Be vigilant and protect yourself from potential fraud concerning COVID-19 vaccines. You will not be asked for money to enhance your ranking for vaccine eligibility. Government and State officials will not call you to obtain personal information in order to receive the vaccine, and you will not be solicited door to door to receive the vaccine.
- Beneficiaries should be cautious of unsolicited requests for their personal, medical, and financial information. Medicare will not call beneficiaries to offer COVID-19 related products, services, or benefit review.
- Be suspicious of any unexpected calls or visitors offering COVID-19 tests or supplies. If you receive a suspicious call, hang up immediately.
- Do not respond to, or open hyperlinks in, text messages about COVID-19 from unknown individuals.
- Ignore offers or advertisements for COVID-19 testing or treatments on social media sites. If you make an appointment for a COVID-19 test online, make sure the location is an official testing site.
- Do not give your personal or financial information to anyone claiming to offer HHS grants related to COVID-19.
- Be aware of scammers pretending to be COVID-19 contact tracers. Legitimate contact tracers will never ask for your Medicare number, financial information, or attempt to set up a COVID-19 test for you and collect payment information for the test.
Proposed Privacy Rules Grant Health Plans New Flexibility, Add New Obligations
December 21, 2020Health plans, health care providers, health insurers, health care clearinghouses (“Covered Entities”) and their business associates should budget and begin compliance plans, even as they comment on proposed changes to the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule announced by the Department of Health & Human Services Office of Civil Rights (“OCR”) in its December 10, 2020 Notice of Proposed Rulemaking (“Proposed Rule). While the official Federal Register publication date has yet to be announced, OCR already is accepting comments pending the official publication. To assure consideration, comments must be received by OCR no later than 60 days from that official Federal Register publication date.
More than 300 pages in length, the proposed HIPAA Privacy Rule changes include grant new flexibility to health plans and health care providers to share protected health information (“PHI”) for care integration and with family and other caregivers, while also imposing tighter requirements on Covered Entities for providing individuals access to PHI and other individual rights. Through the proposed changes, OCR says it hopes to strengthen individuals’ rights to access their own electronic and other health information; improve information sharing for care coordination and case management for individuals; facilitate greater family and caregiver involvement in the care of individuals experiencing emergencies or health crises; enhance flexibilities for disclosures in the Opioid and COVID-19 public health emergencies or other emergency or threatening circumstances; and reduce administrative burdens on HIPAA covered health care providers and health plans. Highlights of some of the more significant proposed changes that the Proposed Rule will make if adopted as proposed include:
New Flexibility To Share PHI For Care Coordination and Case Management Activities
The Proposed Rule also would make a number of changes that OCR believes will remove the barriers created in the current Privacy Rule to Covered Entities, whether a health care provider or health plan, engaging in individual-level care coordination and case management activities. Some of the key elements of these changes include the following:
- Clarification of Rules For Individual-Level Care Coordination. The Proposed Rule would revise existing rules regarding sharing of information for individual-level care coordination to apply to Covered Entities involved in such coordination activities, whether or not the participating Covered Entity is participating in the actual care or treatment of the individual by:
- Revising the definition of “health care operations” in the current version of the Privacy Rule to clarify that the Privacy Rule allows sharing of PHI for individual-level care coordination among Covered Entities whether or not the participating Covered Entity is one involved in treatment or non-treatment involved Covered Entities such as health plans;
- Revises the current minimum necessary restriction on the disclosure of PHI for purposes of individual-level care coordination to treat all Covered Entities engaging in individual-based care coordination and case management activities the same, regardless of whether performing the activities under the “treatment” or “health care operations” functions as defined by HIPAA. Currently non-treatment involved Covered Entities participating in care coordination and case management can only receive and share the minimum necessary PHI as their lack of involvement in treatment disqualifies them for reliance upon the treatment exception to the Privacy Rule’s general requirement to limit disclosures to the minimum necessary.
- The Proposed Rule also would allow Covered Entities to disclose PHI to community-based organizations, home and community-based services (HCBS) providers, social services agencies, and other similar third parties providing health-related services for individual-level care coordination and case management without obtaining a valid authorization from the individual.
Individual Access Rights Expanded
The Proposed Rule includes a number of changes that if adopted as proposed, will increase significantly the burdens upon Covered Entities of complying with the individual access requirements of the Privacy Rule. Among other things, these include the following:
- Responding To Access Requests. The Proposed Rule calls for:
- Reducing the maximum period that Covered Entities have to respond to requests to “as soon as practicable,” but in no case later than 15 calendar days after receipt of the request” instead of current 30 calendar days;
- Clarifying the current requirement for Covered Entities to provide PHI in the form and format requested by the individual if “readily producible” in that form and format by providing that “readily producible” includes secure, standards-based APIs using applications chosen by the individuals, such as a “personal health application” and protect individual’s rights to take notes, videos, and photographs, or use other personal resources to view or capture PHI in person;
- Requiring Covered Entities to allow individuals access to inspect or obtain copies of their own PHI Free of charge when inspecting in person or accessing PHI on the internet, but continue to permit certain fees for labor, supplies, and postage for certain other means of access in accordance with Privacy Rules parameters. In acquiescence to the District Court’s January, 2020 holding that the prohibition against Covered Entities charging for third party copies in the current regulations exceeded its statutory authority in Ciox Health, LLC v. Azar, however the Proposed Rule would allow Covered Entities to charge limited fees to an individual directing transmission of an electronic copy of PHI to a third party under specified circumstances. The Proposed Rule also would require Covered Entities to provide advance notice of estimated fee schedules on their websites (if they have one) for common types of requests for copies of PHI and, upon request, provide individualized estimates of fees for copies and an itemized list of actual costs for requests for copies.
- Right to Direct Copies to Third Parties. The Proposed Rule will require Covered Entities to transmit electronic PHI in an electronic health record to another Covered Entity as part of the individual’s access right. In addition, also in response to the Coix Health, LLC ruling, the Proposed Rule will limit the current right of an individual to direct a copy of PHI to a third party to an electronic copy and will specify that third party direction request need not be in writing as long as it is “clear, conspicuous, and specific.”
- Verification. The Proposed Rule also would prohibit a Covered Entity from imposing “unreasonable” identity verification measures on an individual, including notarization of requests, requiring the individual to provide proof of identity in person when remove verification would be practicable, or requiring the individual to complete a full HIPAA authorization form for an access request.
Disclosures to Family Members and Other Caretakers in Certain Situations
Continuing a trend that OCR has followed over the past several years in its other guidance, the Proposed Rule also would modify the Privacy Rule under specified conditions to facilitate if not encourage health care providers more broadly to disclose PHI to family members or other caretakers of individuals with substance use disorders (SUD) or serious mental illness (SMI) and in emergency situations with less concern about exposing themselves to liability under HIPAA. The key elements of these changes are accomplished as follows:
- The Proposed Rule would replace the current language that allows Covered Entities to make certain uses and disclosures of PHI based on their “exercise of professional judgment” with language allowing disclosure based on a Covered Entity’s “good faith belief” that the use or disclosure is in the best interests of the individual and add a presumption of good faith by the health care provider for this purpose.
- The Proposed Rule would enable Covered Entities to disclose PHI to avert a threat to the health or safety of a person or the public when a harm is “serious and reasonably foreseeable,” instead of the current stricter requirement that the Covered Entity see a “serious and imminent” threat to health or safety.
Clarification Regarding Disclosures to TRS Providers
The Proposed Rule also would amend the current Privacy Rules to remove telephone relay service providers (“TRS providers”) from the definition of “business associates” and expressly to allow disclosures to TRS communications assistants for persons who are deaf, hard of hearing, deaf-blind, or who have a speech disability.
Required Updates To Notices of Privacy Practices
The Proposed Rule also would change the Privacy Rule Notice of Privacy Practices (“NPP”) requirements in a manner that would require most Covered Entities to update their NPPs and associated privacy policies. In the Proposed Rule, OCR proposes:
- Replacing the requirement that certain Covered Entities that have a direct treatment relationship with an individual obtain, and retain copies of, written acknowledgements from that individual confirming their receipt of the NPP with a right for the individual to discuss the NPP with a designee of the Covered Entity.
- Modification of the required NPP content to include an additional description and instruction as to how individuals can exercise their access rights and a new, more detailed and instructive, required header meeting new specifications about the information the NPP provides to individuals with respect to their rights, how to exercise them, and the availability of the Covered Entity’s designated contact person.
Act Now
HIPAA Covered Entities, business associates and other concerned or impacted persons immediately should begin evaluating the Proposed Rule as soon as possible. As the current comment will end 60 days after the impending publication of the Proposed Rule in the Federal Register, concerned persons desiring a change to any provision of the Proposed Rule should prepare and submit appropriate comments to OCR in a timely fashion within the comment period. In addition, all Covered Entities and their business associates should review the rule in preparation for its provisions taking effect with a particular eye toward understanding the actions necessary to comply with the modified rules and to budget the financial and operational resources likely to be required to accomplish that compliance.
More Information
We hope this update is helpful. For more information about the these or other health or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years legal and operational management work, coaching, public policy and regulatory affairs leadership and advocacy, training and public speaking and publications. As a significant part of her work, Ms. Stamer has worked extensively domestically and internationally on an demand, special project and ongoing basis with health industry, health plan and insurance and other business, government and community organizations and their leaders, spoken and published extensively on HIPAA and other privacy and data security concerns, as well as other health care and health benefits; human resources, employee benefits and other workforce and services; insurance; workers’ compensation and occupational disease; business reengineering, disaster and distress; and many other management concerns.
Board Certified in Labor and Employment Law By the Texas Board of Legal Specialization, Scribe for the ABA JCEB Annual Agency Meeting with OCR, Vice Chair of the ABA International Section Life Sciences Committee, and the ABA RPTE Employee Benefits & Other Compensation Group and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer has extensive experience advising, representing, defending and training health care providers, health plans and insurers, employers, community organizations and others about HIPAA and other privacy concerns and has published and spoken extensively on these concerns.
Her involvement with HIPAA and other privacy and data concerns has taken place as part of her more than 30 years involvement working with public and private health industry, health insurance and other employers and organizations of all sizes, employee benefit plans, insurance and financial services, health industry and a broad range of public and private domestic and international business, community and government organizations and leaders on pandemic and other health and safety, workforce and performance preparedness, risks and change management, disaster preparedness and response and other operational and tactical concerns throughout her adult life. A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally and domestically as an advisor to business, community and government leaders on crisis preparedness and response, privacy and data security, workforce, health care and other policy and enforcement, as well as regularly advises and defends organizations about the design, administration and defense of their organizations workforce, employee benefit and compensation, safety, discipline and other management practices and actions.
Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and shares insights and thought leadership through her extensive publications and public speaking. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- New PBGC Pension Rules Effective 3/5 May Require Action On Retirement Plans
- Revise Health Plan HIPAA Records Access Rules & Procedures To Use Newly Flexibility On Charging, Responding To Third Party PHI Requests
- 2/28 New Comment Deadline For NLRB Proposal To Exclude College Work Study Student Workers From NLRA Coverage
- Don’t Get Stuck Paying Another Employer’s Overtime Or Other Backpay
- 2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
- DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
- OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
- Salary Threshold Increases Require Employer Review Of Salaried Worker FLSA Exemption Qualification
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. ©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.
Kickin’ COVID-19: Reopening Texas Summit October 8 On Facebook Live
October 2, 2020A Virtual Summit For Texas Families & Business, Community and Government Leaders On Safely Keeping Texas Working During COVID-19 And Other Pandemics
Presented Via Facebook Live
October 8, 2020
11:00 a.m. – 1:30 p.m. Central Daylight Time
Supercharge your ability to get back to business safely during the COVID-19 and other pandemic health care emergencies by joining other business, community and government leaders online at the Kickin’ COVID-19: Reopening Texas Summit, a free virtual event scheduled on Thursday October 8, 2020 from 11:00 a.m. to 1:30 p.m. Central Daylight Time on Facebook Live.
Solutions Law Press, Inc. PROJECT COPE: COALITION ON PATIENT EMPOWERMENT is happy to join in presenting the Kickin’ COVID-19: Reopening Texas Summit on October 8, 2020 on Facebook Live from 11:00 a.m.-1:30 p.m. Central Time, a free virtual Summit to discuss and share critical tools, information and perspectives to help American citizens, businesses, schools, health care providers, government organizations and leaders and communities better understand options to safely and responsibly do business and get on with life during the COVID-19 and other pandemic outbreaks.
ABOUT THE SUMMIT
Scheduled to be broadcast live on Facebook Live at from 11:30 a.m. to 1:30 p.m. Central Time, the Summit and its resources are designed to empower and inform individuals and families, businesses, schools, churches and other communities and our government leaders about options to continue safe and responsible reopening of Texas and America.
The Summit provides a uniquely valuable opportunity to hear a panel a leading biomedical expert and a panel of other business, community and government leaders share how the COVID-19 health care emergency is affecting their operations, their experiences and strategies reopening in response to these challenges, and their perceptions about the other tools and actions that their organizations for their operations and Texas to reopen and operate safely during the COVID-19 or other pandemic outbreaks. Participants will:
- Hear leading biomedical expert James Burgess objectively explain the science of COVID-19 and other pandemic risks and their management;
- Hear a panel of key business, community and government leaders discuss how COVID-19 impacts their operations, their response, and their thoughts about what their organizations and Texas need to safely resume operations; and
- View and explore a portable pandemic containment unit and other exhibits demonstrating science based pandemic prevention and management tools promoting safe resumption of operations;
- Join the fireside chat between the panel and live audience of business, community and government leaders discuss practical challenges and opportunities for business, community and government leaders separately or collaboratively can help expedite and support the recovery of their own and other businesses, communities, people and economy from the COVID-19 and future pandemics; and
- Collaborate with other business, government and community leaders on reopening and keeping our businesses, governments, communities and economies open and thriving despite the COVID-19 or another pandemic.
Confirmed panelists include:
Biomedical engineer James Burgess, Chief Executive Officer, American Biomedical Group, Inc.
Susan Fletcher, Collin County Commissioner, Precinct 1; Gubernatorial Appointee TCDRS
George C. Fuller, Owner The Guitar Center and The Sanctuary Music & Events Center; Mayor of McKinney, Texas
Traci Mayer, Executive Director, Hotel Association of North Texas
Pam Minick, Executive Vice President of Marketing, Billy Bob’s Texas
Michael Simmons, CISSP, CISM, CISA, CRISC, Managing Director – Technology, Chief Information Security Officer, Southwest Airlines
Cynthia Marcotte Stamer, Executive Director, Project COPE Coalition; Managing Shareholder, Cynthia Marcotte Stamer, P.C.; Vice Chair, American Bar Association International Section Life Sciences & Health Committee and Tort & Insurance Practice Section Medicine & Law Committee
Sean Terry, Chief Operating Officer, Centurion American Development Group; Mayor, City of Celina, Texas; past president of the North Texas Mayors Association
TOUR PANDEMIC MANAGEMENT RESOURCES IN VIRTUAL EXHIBIT HALL
Along with this valuable opportunity to participate in the Summit, participants also can tour the Summit’s Virtual Event Hall of information and exhibits collected as resources for helping to cope with COVID-19 and prepare for future pandemic threats.
The Summit has been organized through a collaboration of business, community and government leaders, who are volunteering their time and resources to share information and discussions they hope will support the continued responsible and safe reopening and continued resumption of operations and life in Texas and across the Nation despite the continued COVID-19 or other pandemic outbreaks. The Solutions Law Press, Inc. is proud to support this effort as part of its PROJECT COPE: Coalition on Patient Empowerment initiatives.
Join the Summit during the live broadcast or in replay at http://www.pandemicresourcegroup.com/pandemic/reopen-texas-summit!
©2020 Solutions Law Press, Inc. All rights reserved.
Employer Option To Defer Paying Some Employee Payroll Taxes Until 2021
September 3, 2020Employers now have the option temporarily to defer paying the employee portion (but not employer’s portion) of certain payroll taxes due between September 1, 2020 to December 31, 2020 for employees earning less than $4000 on a bi-weekly basis.
U.S. Department of the Treasury Notice 2020-65, Relief with Respect to Employment Tax Deadlines Applicable to Employers Affected by the Ongoing Coronavirus (COVID-19) Disease 2019 Pandemic (the “Notice”) issued on August 28, 2020 implements President Trump’s directive in his August 8, 2020 Memorandum on Deferring Payroll Tax Obligations in Light of the Ongoing COVID-19 Disaster (the “Memorandum”) that the Treasury Department allow the deferral of the employee portion of federal payroll taxes (6.2% for Social Security and 1.45% for Medicare) (“Employee Payroll Taxes”) from September 1, 2020 until December 31, 2020 for workers earning less than $4,000 on a biweekly basis (roughly $104,000 annually).
The Notice implements the Memorandum by confirming that employers may (but are not required to) elect to defer the payment of the Employee Payroll Taxes otherwise due on “applicable wages” until next year, after which payment of the deferred Employee Payroll Taxes will be required in installments between January 1, 2021 and April 30, 2021. The option to defer does not, however, extend to the payment of the employer’s portion of payroll taxes. An employer remains obligated timely to pay its employer payroll taxes whether or not the employer elects to take advantage of the Notice’s option to defer paying its employees’ portion of the taxes until 2021.
Employers contemplating this option must keep in mind that the Notice only delays the deadline for the employer to pay the employee portion of the payroll taxes. Employers deferring payment of Employee Payroll Taxes under the Notice remain obligated to pay these taxes to the federal government by the end of April 2021. Employers also will need to consider what arrangements, if any, the employer will make to collect deferred employee payroll taxes from the employee.
More Information
We hope this update is helpful. For more information about this or other health care, human resources, employee benefits, or other legal, operational or risk management developments and strategies, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. provides a broad range of publications and other information, education and other resources and tools to assist management leaders to manage people, process, risk and operations.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Law and Labor and Employment Law and Health Care; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of human resources, employee benefits, compensation and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Ms. Stamer’s work throughout her 30 plus year career has focused heavily on working with health care and managed care, health and other employee benefit plan, insurance and financial services, construction, manufacturing, staffing and workforce and other public and private organizations and their technology, data, and other service providers and advisors domestically and internationally with legal and operational compliance and risk management, performance and workforce management, regulatory and public policy and other legal and operational concerns. As a part of this work, she has continuously and extensively worked with domestic and international employer and other management, employee benefit and other clients on payroll, income and other related tax, workers classification, wage and hour, compensation, benefits, performance, discipline, change and crisis management, internal and agency investigations and defense and a wide range of other workforce matters.
Author of hundreds of highly regarded books, articles and other publications, Ms. Stamer also is widely recognized for her scholarship, coaching, legislative and regulatory advocacy, leadership and mentorship on wage and hour, worker classification and a diverse range of other labor and employment, employee benefits, health and safety, education, performance management, privacy and data security, leadership and governance, and other management concerns within the American Bar Association (ABA), the International Information Security Association, the Southwest Benefits Association, and a variety of other international, national and local professional, business and civic organizations including highly regarded works on worker reclassification and joint employment liability under the FLSA and other laws published by the Bureau of National Affairs and others. Examples of these involvements include her service as the ABA Intellectual Property Law Section Law Practice Management Committee; the ABA International Section Life Sciences and Health Committee Vice Chair-Policy; a Scribe for the ABA Joint Committee on Employee Benefits (JCEB) Annual OCR Agency Meeting and a former JCEB Council Representative and Marketing Chair; Past Chair of the ABA RPTE Employee Benefits and Other Compensation Group and Vice Chair of its Law Practice Management Committee; Past Chair of the ABA Managed Care & Insurance Interest Group; former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Southwest Benefits Association Board member; past Texas Association of Business State Board Member, BACPAC Committee Meeting, Regional and Dallas Chapter Chair; past Dallas Bar Association Employee Benefits Committee Executive Committee; former SHRM Region IV Chair and National Consultants Forum Board Member; for WEB Network of Benefit Professionals National Board Member and Dallas Chapter Chair; former Dallas World Affairs Council Board Member; founding Board Member, past President and Patient Empowerment and Health Care Heroes founder for the Alliance for Health Care Excellence; former Gulf States TEGE Council Exempt Organizations Coordinator and Board member; past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and involvement in a broad range of other professional and civic organizations. For more information about Ms. Stamer or her health industry and other experience and involvements, see http://www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here.
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The author and Solutions Law Press, Inc. disclaim, and have no responsibility to provide any update or otherwise notify anyone any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
DOL Invests $80.6 million in Apprenticeship Expansion Grants
July 3, 2020The U.S. Department of Labor has announced $80.6 million in apprenticeship expansion grants to 42 states and territories that will help create opportunities in new and traditional fields for more Americans to get the skills they need for family-sustaining jobs. Apprenticeship training can be a valuable opportunity for employers to recruit and retain qualified workers and workers to develop new skills. Get more details here.
For More Information
We hope this update is helpful. For more information about this or other labor and employment developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Law and Labor and Employment Law and Health Care; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of health industry and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Ms. Stamer also is widely recognized for her scholarship, coaching, legislative and regulatory advocacy, leadership and mentorship on wage and hour, worker classification and a diverse range of other labor and employment, employee benefits, health and safety, education, performance management, privacy and data security, leadership and governance, and other management concerns within the American Bar Association (ABA), the International Information Security Association, the Southwest Benefits Association, and a variety of other international, national and local professional, business and civic organizations including highly regarded works on worker reclassification and joint employment liability under the FLSA and other laws published by the Bureau of National Affairs and others. Examples of these involvements include her service as the ABA Intellectual Property Law Section Law Practice Management Committee; the ABA International Section Life Sciences and Health Committee Vice Chair-Policy; a Scribe for the ABA Joint Committee on Employee Benefits (JCEB) Annual OCR Agency Meeting and a former JCEB Council Representative and Marketing Chair; Past Chair of the ABA RPTE Employee Benefits and Other Compensation Group and Vice Chair of its Law Practice Management Committee; Past Chair of the ABA Managed Care & Insurance Interest Group; former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Southwest Benefits Association Board member; past Texas Association of Business State Board Member, BACPAC Committee Meeting, Regional and Dallas Chapter Chair; past Dallas Bar Association Employee Benefits Committee Executive Committee; former SHRM Region IV Chair and National Consultants Forum Board Member; for WEB Network of Benefit Professionals National Board Member and Dallas Chapter Chair; former Dallas World Affairs Council Board Member; founding Board Member, past President and Patient Empowerment and Health Care Heroes founder for the Alliance for Health Care Excellence; former Gulf States TEGE Council Exempt Organizations Coordinator and Board member; past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and involvement in a broad range of other professional and civic organizations. For more information about Ms. Stamer or her health industry and other experience and involvements, see http://www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources.
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The author and Solutions Law Press, Inc. disclaim, and have no responsibility to provide any update or otherwise notify anyone any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
Businesses Should Confirm Using Benefits, Meeting Mandates Of Special COVID-19 Tax Rules
June 26, 2020Earlier this week, the Internal Revenue Service (“IRS”) announced that employee benefit plan participants that already took a required minimum distribution (RMD) in 2020 from certain retirement accounts now has the opportunity through August 31, 2020 to roll those funds back into a retirement account following the Coronavirus Aid, Relief, and Economic Security (CARES) Act RMD waiver for 2020. The announcement of this relief covers one of a long and growing list of special tax and other COVID-19 responsive special rules and requirements that may change requirements, provide special relief or both for businesses and individuals that every business leader and individual should carefully monitor and respond to appropriately.
Retirement Plan Rollover Relief
On July 23, 2020, the IRS announced its extension of the 60-day rollover period for any RMDs already taken this year to August 31, 2020 to give taxpayers time to take advantage of this opportunity in Notice 2020-51 (PDF). The Notice also answers questions regarding the waiver of RMDs for 2020 under the Coronavirus Aid, Relief, and Economic Security Act, known as the CARES Act.
The CARES Act enabled any taxpayer with an RMD due in 2020 from a defined-contribution retirement plan, including a 401(k) or 403(b) plan, or an IRA, to skip those RMDs this year. This includes anyone who turned age 70 1/2 in 2019 and would have had to take the first RMD by April 1, 2020. This waiver does not apply to defined-benefit plans.
In addition to the rollover opportunity, an IRA owner or beneficiary who has already received a distribution from an IRA of an amount that would have been an RMD in 2020 can repay the distribution to the IRA by August 31, 2020. The notice provides that this repayment is not subject to the one rollover per 12-month period limitation and the restriction on rollovers for inherited IRAs.
The notice provides two sample amendments that employers may adopt to give plan participants and beneficiaries whose RMDs are waived a choice as to whether or not to receive the waived RMD.
Other COVID-19 Tax Rules & Relief
The guidance and relief in Notice 2020-51 highlights only one of a long list of special COVID-19 associated tax rules and relief that could apply to a business, its employees or employee benefit plan participants or both including the following:
- IR-2020-127, IRS announces rollover relief for required minimum distributions from retirement accounts that were waived under the CARES Act
- IR-2020-126, IRS extends July 15, other upcoming deadlines for tornado victims in parts of the South; provides other relief
- IR-2020-124, Relief for taxpayers affected by COVID-19 who take distributions or loans from retirement plans
- IR-2020-122, IRS outlines changes to health care spending available under CARES Act
- IR-2020-121, IRS alert: Economic Impact Payments belong to recipient, not nursing homes or care facilities
- IR-2020-120, Treasury, IRS provide tax relief to investors and businesses affected by COVID-19 in new markets tax credit transactions
- IR-2020-119, IRS provides guidance on employer leave-based donation programs that aid victims of the COVID-19 pandemic
- IR-2020-118, IRS reminder: File now, choose direct deposit or schedule tax payments electronically before the July 15 deadline
- IR-2020-117, IRS reminder: Deadline postponed to July 15 for those who pay estimated taxes
- IR-2020-115, IRS warns against COVID-19 fraud; other financial schemes
- IR-2020-114, IRS provides answers about Coronavirus related tax relief for Qualified Opportunity Funds and investors
- IR-2020-111, 159 million Economic Impact Payments processed; Low-income people and others who aren’t required to file tax returns can quickly register for payment with IRS Non-Filers tool
- IR-2020-110, IRS provides relief to retirement plan participants to sign elections remotely
- IR-2020-109, IRS reminder: June 15 tax deadline postponed to July 15 for taxpayers who live and work abroad
- IR-2020-106, Treasury, IRS provide safe harbor for taxpayers that develop renewable energy projects
- IR-2020-105, Economic Impact Payments being sent by prepaid debit cards, arrive in plain envelope; IRS.gov answers frequently asked questions
- IR-2020-101, Treasury, IRS release latest state-by-state Economic Impact Payment figures for May 22, 2020
- IR-2020-99, IRS.gov helps taxpayers get tax information they need; find tools for filing, paying, checking accounts and answering questions
- Treasury News Release: Treasury is Delivering Millions of Economic Impact Payments by Prepaid Debit Card
- IR-2020-97, IRS adds phone operators to answer Economic Impact Payment questions
- IR-2020-96, IRS expands partner materials for Economic Impact Payments; continues sweeping effort to share details in multiple languages
- IR-2020-95, IRS provides tax relief through increased flexibility for taxpayers in section 125 cafeteria plans
- IR-2020-93, Why the Economic Impact Payment amount could be different than anticipated
- IR-2020-92, Act by Wednesday for chance to get quicker Economic Impact Payment; timeline for payments continues to accelerate
- IR-2020-91, Treasury, IRS release latest state-by-state Economic Impact Payment figures
- IR-2020-89, IRS: Three new credits are available to many businesses hit by COVID-19
- IR-2020-87, IRS retools Settlement Days program in response to COVID-19 pandemic; allows unrepresented taxpayers to settle their cases virtually and reach finality
- IR-2020-86, VA, SSI recipients with eligible children need to act by Tuesday, May 5 to quickly add money to their automatic Economic Impact Payment; ‘Plus $500 Push’ continues
- IR-2020-85, Economic Impact Payments continue to be sent, check IRS.gov for answers to common questions
- IR-2020-83, Use IRS Non-Filers: Enter Payment Info Here tool to get Economic Impact Payment; many low-income, homeless qualify
- IR-2020-82, IRS enhances Get My Payment online application to help taxpayers
- IR-2020-81, VA, SSI recipients with eligible children need to act by May 5 to quickly add money to their automatic Economic Impact Payment; ‘Plus $500 Push’ continues
- IR-2020-80, Treasury, IRS deliver 89.5 million Economic Impact Payments in first three weeks, release state-by-state Economic Impact Payment figures (Updated: April 28, 2020)
- IR-2020-77, Treasury, IRS announce cross-border tax guidance related to travel disruptions arising from the COVID-19 emergency
- IR-2020-76, SSA, RRB recipients with eligible children need to act by Wednesday to quickly add money to their automatic Economic Impact Payment; IRS asks for help in the “Plus $500 Push”
- IR-2020-75, Veterans Affairs recipients will receive automatic Economic Impact Payments; Step follows work between Treasury, IRS, VA
- IR-2020-74, IRS: Free File use soars; taxpayers still have time to do their taxes for free
- IR-2020-73, Supplemental Security Income recipients will receive automatic Economic Impact Payments; step follows work between Treasury, IRS, Social Security Administration
- IR-2020-72, Treasury, IRS unveil online application to help with Economic Impact Payments
- IR-2020-71, IRS, Security Summit partners warn tax professionals on scams, urge additional security measures to protect taxpayer data
- IR-2020-70, REMINDER: Schedule and pay federal taxes electronically due by July 15; only a few hours remaining for taxpayers to reschedule payments set for April 15
- IR-2020-69, Treasury, IRS launch new tool to help non-filers register for Economic Impact Payments
- IR-2020-68, IRS urges taxpayers to use electronic options; outlines online assistance
- IR-2020-67, IRS provides guidance under the CARES Act to taxpayers with net operating losses
- IR-2020-66, To help taxpayers, the Department of Treasury and the Internal Revenue Service announced today that Notice 2020-23 extends additional key tax deadlines for individuals and businesses
- IR-2020-65, Follow IRS on social media, sign up for e-news subscriptions for urgent updates on COVID-19, scams and economic impact payment information
- IR-2020-64, IRS issues warning about coronavirus-related scams; watch out for schemes tied to economic impact payments
- Treasury News Release: Social Security recipients will automatically receive Economic Impact Payments
- IR 2020-62, IRS: Employee Retention Credit available for many businesses financially impacted by COVID-19
- IR 2020-61, Economic impact payments: What you need to know
- IR-2020-59, IRS unveils new People First Initiative; COVID-19 effort temporarily adjusts, suspends key compliance program
- IR-2020-58, Tax Day now July 15: Treasury, IRS extend filing deadline and federal tax payments regardless of amount
- IR-2020-57, Treasury, IRS and Labor announce plan to implement coronavirus-related paid leave for workers and tax credits for small and midsize businesses to swiftly recover the cost of providing Coronavirus-related leave
- Treasury News Release: Treasury and IRS issue guidance on deferring tax payments due to COVID-19 outbreak
- IR-2020-54, IRS: High-deductible health plans can cover coronavirus costs
Along with these tax rules, businesses and their employees also may be impacted by a broad range of special federal and state labor and employment and other rules adopted in response to the continuing COVID-19 health care emergency and its fallout. Businesses and their leaders should carefully review and monitor these and other COVID-19 specific rules to ensure that their businesses don’t trigger unanticipated liability by failing to meet critical requirements or to ensure that they take full advantage of all available relief.
More Information
We hope this update is helpful. For more information about the these or other health or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years legal and operational management work, coaching, public policy and regulatory affairs leadership and advocacy, training and public speaking and publications. As a significant part of her work, Ms. Stamer has worked extensively domestically and internationally on an demand, special project and ongoing basis with health industry, health plan and insurance and other businesses of all types, government and community organizations and their leaders, spoken and published extensively on workforce and other services, compensation and benefits, and related tax; insurance; workers’ compensation and occupational disease; business reengineering, disaster and distress; and many other management concerns.
Board Certified in Labor and Employment Law By the Texas Board of Legal Specialization, Scribe for the ABA JCEB Annual Agency Meeting with OCR, Vice Chair of the ABA International Section Life Sciences Committee, and the ABA RPTE Employee Benefits & Other Compensation Group and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer has extensive experience advising, representing, defending and training health care providers, health plans and insurers, employers, community organizations and others about HIPAA and other privacy concerns and has published and spoken extensively on these concerns.
Her involvement with HIPAA and other privacy and data concerns has taken place as part of her more than 30 years involvement working with with public and private health industry, health insurance and other employers and organizations of all sizes, employee benefit plans, insurance and financial services, health industry and a broad range of public and private domestic and international business, community and government organizations and leaders on pandemic and other health and safety, workforce and performance preparedness, risks and change management, disaster preparedness and response and other operational and tactical concerns throughout her adult life. A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally and domestically as an advisor to business, community and government leaders on crisis preparedness and response, privacy and data security, workforce, health care and other policy and enforcement, as well as regularly advises and defends organizations about the design, administration and defense of their organizations workforce, employee benefit and compensation, safety, discipline and other management practices and actions.
Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and shares insights and thought leadership through her extensive publications and public speaking. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- Ezekiel Elliott COVID-19 Diagnosis Disclosure Outrage Highlights Need To Handle COVID-19 & Other Medical Information With Care
- Proposed Regulations Would Treat Direct Primary Care and Health Care Sharing Ministries Membership Dues As Qualifying Medical Expenses For Medical Deduction & HSA Reimbursement Purposes
- Wish Tax Guidance Were Clearer? Tell IRS/Treasury Your Suggested Topics For 2020-2021 Treasury Priority Guidance Plan
- New IRS Increased Health FSA Carryover, Gives COVID Health FSA Election Relief
- IRS Shares Initial CARES Act Plan Loan & Distribution Relief Guidance
- Employer Sponsors & Health Plans Face Rising Risk From Mental Health & Substance Abuse Coverage Violations
- Use Prudent Process To Manage Workforce & Other Business Changes To Help Minimize Business & Management Liabilities & Protect Future Recovery
- Congress Expected To Pass COVID-19 Relief Bill With Paid Leave Mandates & Expanded Unemployment Funding This Week
- New Resources For Businesses, Employers, Schools & Homes To Stay Safe From COVID-19
- Self Insured Plan & Contract Amendments Likely Required To Waive Deductibles, Expand Other Coronavirus Coverage
- Health Plans, Providers & PBM Face Pressure To Prepare For Health Transparency As Trump Transparency Reforms March Foward
- Proposed HHS Rule Making PBM Expenses Part of MLS Administrative Expense, Other Changes To ACA Health Plan Rules Comment Deadline 5 P.M. Today
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- New PBGC Pension Rules Effective 3/5 May Require Action On Retirement Plans
- Revise Health Plan HIPAA Records Access Rules & Procedures To Use Newly Flexibility On Charging, Responding To Third Party PHI Requests
- 2/28 New Comment Deadline For NLRB Proposal To Exclude College Work Study Student Workers From NLRA Coverage
- Don’t Get Stuck Paying Another Employer’s Overtime Or Other Backpay
- 2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
- DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
- OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
- Salary Threshold Increases Require Employer Review Of Salaried Worker FLSA Exemption Qualification
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. ©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.
Ezekiel Elliott COVID-19 Diagnosis Disclosure Outrage Highlights Need To Handle COVID-19 & Other Medical Information With Care
June 16, 2020While most COVID-19 test results won’t draw the widespread coverage and public interest that Elliott’s diagnosis did, businesses generally and health care providers, health plans, health care clearinghouses specifically need to recognize that coverage of the Elliott outrage will heighten awareness and therefore their need to properly handle and protect COVID-19 or other infectious disease and other testing, diagnosis, treatment and other medical and disability information collected or encountered in the course of their operation through the current COVID-19 health care emergency and otherwise in their own organizations.
ADA Responsibilities of Employers In Handling Medical Information
Protecting COVID-19 testing and other medical information isn’t just a concern for covered entities and their business associates, however. Businesses that are not covered entities also generally should use care in their collection, use, protection and disclosure of COVID-19 testing and other medical information to mitigate their potential liability under the disability discrimination requirements of the ADA, the Rehabilitation Act and other laws. For instance, along with prohibiting employers covered by the ADA from discriminating against qualified individuals with disabilities and requiring those employers to provide reasonable accommodations to such employees, the ADA also regulates the ability of covered employers to perform or require medical testing and imposes specific medical confidentiality requirements on all covered employers. See e.g., What You Should Know About COVID-19 and the ADA, the Rehabilitation Act, and Other EEO Laws.
The ADA’s medical confidentiality requirements dictate that covered employers maintain medical information and records about employees and applicants in separate, confidential files. Covered employers are responsible for maintaining the confidentiality of medical information and records and cannot disclose it without authorization from the subject employee except under the specific conditions allowed by the ADA.
EEOC guidance provided in its publication entitled Pandemic Preparedness in the Workplace and the Americans With Disabilities Act as updated as of March 19, 2020 emphasizes that covered employers remain accountable for complying with the requirements of the ADA and Rehabilitation Act during the current COVID-19 health care emergency and other pandemics.
While the EEOC Technical Assistance Questions and Answers in its publication What You Should Know About COVID-19 and the ADA, the Rehabilitation Act, and Other EEO Laws
Technical Assistance Questions and Answers as updated on June 11, 2020 recognizes temperature checks and certain other COVID-19 inquiries to screen for COVID-19 exposure or infection might be permitted under the safety exception to the ADA during the current COVID-19 health care emergency, that and other EEOC guidance makes clear that covered employers remain responsible for ensuring that the ADA medical confidentiality requirements are met with regarding to testing and related medical information. As a result, all ADA-covered employers generally and health care employers specifically are urged to use care both in the administration and collection of information regarding COVID-19 testing and diagnosis, and the protection of the confidentiality of COVID-19 and other medical information and records collected in the course of administering employment, safety, medical leave or other absence or other operations throughout the COVID-19 health care emergency.
Added HIPAA & Texas HIPAA Concerns For Health Plans & Other HIPAA Covered Entities
Assuming that the disclosure of Elliott’s information is traced to a testing provider, laboratory or other health care provider, health plan or insurer, health care clearing house subject to HIPAA (“covered entity”), a service provider acting as a business associate to a covered entity, or a member of their workforce, the unauthorized release of Elliott’s test results, that he underwent the testing, or other medical information, Elliott’s complaint about a possible HIPAA violation could be well-founded as both HIPAA and the somewhat broader provisions of the Texas Medical Privacy Act (“Tex-HIPAA”) (hereafter collectively the “HIPAA Laws”) both generally prohibit unauthorized disclosure of protected medical information such as his COVID-19 test or test results to the media.
The COVID-19 test results and of “individually identifiable personal health information” about Elliott and his encounter created, used, access or disclosed by the testing facility or other health care provider, a health plan, health care clearinghouse (“covered entity”) or a member of its workforce or a subcontractor acting as a business associated qualify as “protected health information subject to HIPAA’s privacy, security, breach and privacy rights protections of HIPAA and Tex-HIPAA.
The HIPAA and Tex-HIPAA prohibition against unauthorized disclosure of protected health information to the media stem from the HIPAA Laws’ broader requirement that covered entities and business associates affirmatively safeguard protected health information against unauthorized use, access or disclosure and sweeping prohibition against their disclosing or allowing the disclosure of protected health information without a HIPAA-compliant authorization except under the narrow and specifically delineated exceptions identified in the rule, none of which appear relevant to the media disclosure objected to by Elliott from the currently available public information.
Both HIPAA Laws expressly prohibit unauthorized disclosure of protected health information by covered entities or their business associates except under the specifically detailed conditions specified in one or more exceptions to this general rule. Assuming all relevant conditions to qualify for the exception are met, HIPAA does allow covered entities and business associates treatment, payment, operations, public health activities or another situation meeting all applicable requirements of an express exception to the HIPAA prohibition against disclosure.
The federal agency primarily responsible for the implementation and enforcement of HIPAA, the Department of Health & Human Services Office of Civil Rights (“OCR”) regulatory guidance and enforcement history clearly communicates OCR’s view that covered entities or business associates violate HIPAA by disclosing protected health information to the media or other third parties without first obtaining a HIPAA-compliant authorization from the subject of the information except under the specific circumstances described in an applicable Privacy Rule exception.
In its May 5, 2020 Guidance on Covered Health Care Providers and Restrictions on Media Access to Protected Health Information about Individuals in Their Facilities (“5/5 Guidance”), for instance, OCR specifically reminded HIPAA covered health care providers that the HIPAA Privacy Rule does not permit them to give media and film crews access to protected health information including access to facilities where patients’ protected health information will be accessible without the patients’ prior authorization. has made clear that testing facilities and other health care providers generally remain accountable for complying with the HIPAA Privacy Rule that prohibits unauthorized use, access or disclosure of test results and other protected health information except as specifically allowed in the applicable HIPAA Law.
The 5/5 Guidance specifically states, “The COVID-19 public health emergency does not alter the HIPAA Privacy Rule’s existing restrictions on disclosures of protected health information (PHI) to the media.’ Additionally, it states confirmed that even during the current COVID-19 public health emergency, covered health care providers remain required to obtain a valid HIPAA authorization from each patient whose PHI will be accessible to the media before the media is given access to that PHI. In this regard, the 5/5 Guidance states, As explained in prior guidance,1 HIPAA does not permit covered health care providers to give the media, including film crews, access to any areas of their facilities where patients’ PHI will be accessible in any form (e.g., written, electronic, oral, or other visual or audio form), without first obtaining a written HIPAA authorization from each patient whose PHI would be accessible to the media. 2 Additionally, covered health care providers may not require a patient to sign a HIPAA authorization as a condition of receiving treatment. The guidance clarifies that masking or obscuring patients’ faces or identifying information before broadcasting a recording of a patient is not sufficient, as a valid HIPAA authorization is still required before giving the media such access. Additionally, the guidance describes reasonable safeguards that should be used to protect the privacy of patients whenever the media is granted access to facilities.
OCR’s positions on disclosures to the media in the 5/5 Guidance reaffirm OCR’s longstanding interpretation and enforcement of HIPAA as prohibiting disclosures of PHI and media access to areas where patients or their protected health information might be visible or accessible is long standing.
In June, 2013, for instance, OCR sent a clear message to covered entities and business associates not to make unconsented disclosures of protected health information to or allow media access to areas where patients or their protected health information could be accessed or observed when it required Shasta Regional Medical Center (SRMC) to pay $275,000 to resolve OCR HIPAA charges stemming from SRMC’s unauthorized disclosure of protected health information to multiple media outlets as part of a public relations effort to mitigate damage from fraud and misconduct allegations made against it by the patient. See HIPAA Sanctions Triggered From Covered Entity Statements To Media, Workforce.
OCR subsequently reinforced its warning to covered entities and business associates about unauthorized disclosures of protected health information in a 2016 Frequently Asked Question (Media FAQ) that discussed covered entities HIPAA responsibilities when dealing with the media. The Media FAQ was issued in conjunction with OCR’s collection of its $2.2 million settlement with New York-Presbyterian Hospital and a series of other settlements totaling $999,000 from three other health care providers accused of violating HIPAA by allowing media personnel into treatment or other areas where patients or patient protected health information was accessible without first obtaining a HIPAA compliant written authorization from each patient or other subject present or whose protected health information otherwise would be accessible to the media. See $999K Price Hospitals Pay To Settle HIPAA Privacy Charges From Allowing ABC To Film Patients Without Authorization.
In the Media FAQ, OCR stated HIPAA required covered entities to obtain prior written authorization before disclosing protected health information to the media or allowing media to film or access exam rooms or other areas where patients or protected health information could be observed or accessed. The Media FAQ also stated that masking or blurring the identity of the patient or their specific information was not an adequate substitute for written authorization and that covered entities also were responsible for ensuring that reasonable safeguards were in place to protect against impermissible disclosures or to limit incidental disclosures of other PHI in areas where media is allowed access where prior authorization has not been obtained. While stressing the importance of compliance with these requirements, however, the Media FAQ clarified that the HIPAA Privacy Rule does not require health care providers to prevent members of the media from entering areas of their facilities that are otherwise generally accessible to the public like public waiting areas or areas where the public enters or exits the facility In addition, the Media FAQ states a health care provider or other Covered Entity also highlighted certain other limited circumstances where HIPAA might allow limited disclosure of protected health information to the media in accordance with specific provisions of the Privacy Rule about an incapacitated patient when in the patient’s best interest; or disclose a patient’s location in the facility and condition in general terms that do not communicate specific medical information about the individual to the media or any other person any person where the individual has not objected to his information being included in the facility directory and the media representative or other person asks for the individual by name.
In the intervening years, OCR periodically has issued additional reminders to covered entities about HIPAA’s general prohibition against unconsented disclosures to the media as well as sanctioned harshly various covered entities for violating these prohibitions. In 2017, OCR required the largest not-for-profit health system in Southeast Texas, Memorial Hermann Health System (MHHS), to pay OCR $2.4 million to settle charges it violated HIPAA by issuing a press release to the media that shared the name and other protected health information about a patient suspected of using a fraudulent insurance card to obtain care at a clinic without the patient’s prior HIPAA-compliant authorization. While OCR concluded a report made MHHS made to law enforcement about the patient was allowable under the Privacy Rule, OCR found MHHS violated the Privacy Rule by issuing the press release disclosing the patient’s name and other PHI without authorization from the patient and also by failing to timely document the sanctioning of its workforce members for impermissibly disclosing the patient’s information. See $2.4M HIPAA Settlement Warns Providers About Media Disclosures Of PHI.
While OCR has announced certain temporary enforcement relief from a narrow set of HIPAA requirements during the COVID-19 health care emergency as applied to certain qualifying testing facilities, telemedicine providers and other specific health care providers engaging in certain types of health care during the COVID-19 health care emergency, OCR consistently has made clear that its COVID-19 HIPAA relief is very limited in scope, applicability and duration and in no way waives the prohibition against unauthorized disclosure to the media or other third parties not generally permitted under HIPAA. See e.g., 5/5 Guidance; OCR Issues Guidance on How Health Care Providers Can Contact Former COVID-19 Patients About Blood and Plasma Donation Opportunities; OCR Announces Notification of Enforcement Discretion for Community-Based Testing Sites During the COVID-19 Nationwide Public Health Emergency; OCR Announces Notification of Enforcement Discretion to Allow Uses and Disclosures of Protected Health Information by Business Associates for Public Health and Health Oversight Activities During The COVID-19 Nationwide Public Health Emergency; OCR Issues Bulletin on Civil Rights Laws and HIPAA Flexibilities That Apply During the COVID-19 Emergency; OCR Issues Guidance to Help Ensure First Responders and Others Receive Protected Health Information about Individuals Exposed to COVID-19; OCR Issues Guidance on Telehealth Remote Communications Following Its Notification of Enforcement Discretion; OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency. To the contrary, OCR’s announcement of the 5/5 guidance quotes OCR Director Roger Severino, as stating “Hospitals and health care providers must get authorization from patients before giving the media access to their medical information; obscuring faces after the fact just doesn’t cut it,” Severino added.
Minimize Exposures By Preventing Unauthorized Media & Other Disclosures
Even without Mr. Elliott’s outrage heightening awareness about HIPAA’s prohibitions against unauthorized disclosures of protected health information to the media, the recent warning about HIPAA’s restrictions on media disclosure and access to protected health information and patient treatment areas in OCR’s 5/5 Guidance alone should serve as a strong incentive for covered entities and business associate promptly to reverify that the adequacy of their current policies, practices and training to prevent inappropriate media disclosures of protected health information and otherwise defend their compliance with OCR’s interpretation of HIPAA’s requirements for dealing with the media. Predictable heightened patient and public awareness and expectations about these and other HIPAA responsibilities fueled by the widespread media coverage of Mr. Elliott’s COVID-19 test results and his outrage about the unauthorized disclosure of his test results makes it more important than ever that health care providers and other covered entities and business associates take steps to prepare to respond to foreseeable complaints and questions by other patients, their families and others.
As part of these efforts, most covered entities and business associates may want to consider, at minimum, reconfirming the adequacy and understanding of their current media and other disclosure policies and practices, as well as sending strategic communications to their business associates and members of their workforce reminding them of the covered entity’s policies regarding media access and disclosures.
As part of these activities, covered entities should consider conducting a well-documented assessment of their current policies, practices and workforce training on disclosure of information to the media and other parties generally, as well as policies on allowing media or other parties to enter, film, photograph or record within their facilities or otherwise disclosing or allowing media access to their facilities. Along with these efforts, most covered entities also may want to consider also reminding workforce members that their patient privacy responsibilities also requires that they not share or discuss patient protected health information, film, photograph, or otherwise record, patients or areas where patients or patient protected health information is or might be present without prior written consent of the patient and the consent of their organization.
Since covered entities and members of their workforce also are likely to be subject to other statutory, ethical, contractual or other privacy or confidentiality requirements beyond those imposed by the HIPAA Laws such as medical confidentiality duties applicable to physicians and other health care providers under medical ethics, professional licensure or other similar rules, contractual responsibilities, as well as common law or statutory privacy, theft of likeness or other statutory or common law tort claims and exposures. Covered entities and business associates generally should consider whether other steps are advisable to manage these exposures along with managing their HIPAA Law compliance.
Given the high incidence of COVID-19 exposure and infection within their workplace, covered entities, business associates and other employers should use care fulfill their HIPAA Law relevant employment law confidentiality responsibilities when dealing with testing or other medical information about employees. In this respect, along with any HIPAA Law obligations that a covered entity or business associate has in handling medical information about a patient who also is an employee or family member of an employee, covered entities also should use care to ensure that medical confidentiality requirements of the Americans With Disabilities Act (“ADA”) and other applicable employment laws are met.
Since this analysis and review in most cases will result in the uncovering or discussion of potentially legally or politically sensitive information, Covered Entities should consider consulting with or engaging experienced legal counsel for assistance in structuring and executing these activities to maximize their ability to claim attorney-client privilege or other evidentiary protections against discovery or disclosure of certain aspects of these activities.
Finally, covered entities should keep in mind that HIPAA and other medical privacy compliance and risk management is an ongoing process requiring constant awareness and diligence. Consequently, covered entities and business associates also should use care both to monitor OCR and other regulatory and enforcement developments as well as exercise ongoing vigilance to monitor and maintain compliance within their organizations.
More Information
We hope this update is helpful. For more information about the these or other health or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years legal and operational management work, coaching, public policy and regulatory affairs leadership and advocacy, training and public speaking and publications. As a significant part of her work, Ms. Stamer has worked extensively domestically and internationally on an demand, special project and ongoing basis with health industry, health plan and insurance and other business, government and community organizations and their leaders, spoken and published extensively on HIPAA and other privacy and data security concerns, as well as other health care and health benefits; human resources, employee benefits and other workforce and services; insurance; workers’ compensation and occupational disease; business reengineering, disaster and distress; and many other management concerns.
Board Certified in Labor and Employment Law By the Texas Board of Legal Specialization, Scribe for the ABA JCEB Annual Agency Meeting with OCR, Vice Chair of the ABA International Section Life Sciences Committee, and the ABA RPTE Employee Benefits & Other Compensation Group and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer has extensive experience advising, representing, defending and training health care providers, health plans and insurers, employers, community organizations and others about HIPAA and other privacy concerns and has published and spoken extensively on these concerns.
Her involvement with HIPAA and other privacy and data concerns has taken place as part of her more than 30 years involvement working with with public and private health industry, health insurance and other employers and organizations of all sizes, employee benefit plans, insurance and financial services, health industry and a broad range of public and private domestic and international business, community and government organizations and leaders on pandemic and other health and safety, workforce and performance preparedness, risks and change management, disaster preparedness and response and other operational and tactical concerns throughout her adult life. A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally and domestically as an advisor to business, community and government leaders on crisis preparedness and response, privacy and data security, workforce, health care and other policy and enforcement, as well as regularly advises and defends organizations about the design, administration and defense of their organizations workforce, employee benefit and compensation, safety, discipline and other management practices and actions.
Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and shares insights and thought leadership through her extensive publications and public speaking. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- Proposed HHS Rule Making PBM Expenses Part of MLS Administrative Expense, Other Changes To ACA Health Plan Rules Comment Deadline 5 P.M. Today
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- New PBGC Pension Rules Effective 3/5 May Require Action On Retirement Plans
- Revise Health Plan HIPAA Records Access Rules & Procedures To Use Newly Flexibility On Charging, Responding To Third Party PHI Requests
- 2/28 New Comment Deadline For NLRB Proposal To Exclude College Work Study Student Workers From NLRA Coverage
- Don’t Get Stuck Paying Another Employer’s Overtime Or Other Backpay
- 2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
- DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
- OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
- Salary Threshold Increases Require Employer Review Of Salaried Worker FLSA Exemption Qualification
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. ©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.
Proposed Regulations Would Treat Direct Primary Care and Health Care Sharing Ministries Membership Dues As Qualifying Medical Expenses For Medical Deduction & HSA Reimbursement Purposes
June 11, 2020August 8, 2020 is the deadline to comment on Internal Revenue Service (“IRS”) proposed regulations that if adopted as proposed will allow membership payments for participation in direct primary care (“DPC”) and health care sharing ministries (“HCSMs”) to qualify as medical expenses eligible for the itemized deduction under Internal Revenue Code (“Code”) Section 213 and for reimbursement by an employer sponsored health reimbursement arrangement (“HRA”).
Section 213 of the Code allows individuals to take an itemized deduction for expenses for medical care, including insurance for medical care, to the extent the expenses exceed 7.5% of adjusted gross income.
In Executive Order 13877, Improving Price and Quality Transparency in American Healthcare to Put Patients First” (84 FR 30849 (June 27, 2019), President Trump directed the Secretary of the Treasury, to the extent consistent with law, to “propose regulations to treat expenses related to certain types of arrangements, potentially including direct primary care arrangements and healthcare sharing ministries, as eligible medical expenses under Section 213(d)” of the Code.
In response to Executive Order 13877, the proposed regulations proposed that:
- Payments for DPC arrangements are expenses for medical care under section 213 of the Code. Because these payments are for medical care, a health reimbursement arrangement (HRA) provided by an employer generally may reimburse an employee for DPC arrangement payments.
- Payments for membership in a HCSM are expenses for medical care under section 213 of the Code. Because these payments are for medical care, an HRA provided by an employer generally may reimburse an employee for HCSM membership payments.
Although DPC and HCSM arrangements have gained increasing popularity as alternatives to traditional health insurance among many taxpayers, current ruling IRS guidance prohibited individual taxpayers from counting DPC or HCSM membership dues as medical expenses for purposes of claiming an itemized medical expense deduction and characterized those amounts as ineligible for nontaxable reimbursement under employer sponsored HRAs. The proposed regulations would reverse these positions to allow those membership dues paid for a DPC or HCSM membership as defined in the proposed regulations to qualify for the itemized medical expense deduction by individual taxpayers and as exempt from wages when reimbursed as a medical expense by an employer sponsored HRA. The proposed regulations specify that the rules proposed would become effective for taxable years ending on or after the date of publication of the Treasury decision adopting these rules as final regulations in the Federal Register. Accordingly, as presently written, amounts paid for DPC or HCSM memberships before the effective date of the final regulations presumably would continue to be treated under existing rules and therefore not be eligible to count as medical expenses for purposes of the itemized medical expense deduction or for reimbursement under a HRA.
The proposed regulations invite comments both on the proposed tax treatment of DPC and HCSM membership dues and the arrangements that the proposed regulations would recognize as qualifying as a DPC or HCSM arrangement for purposes of these rules and address certain other analysis and matters regarding the treatment of membership dues paid to these arrangements.
DPC Definition
Relative to the arrangements that would qualify as a DPC arrangement, the proposed regulations provide that a “direct primary care arrangement” as a contract between an individual and one or more primary care physicians under which the physician or physicians agree to provide medical care (as defined in section 213(d)(1)(A)) for a fixed annual or periodic fee without billing a third party. The proposed regulations define a “primary care physician” as an individual who is a physician (as described in section 1861(r)(1) of the Social Security Act (SSA)) who has a primary specialty designation of family medicine, internal medicine, geriatric medicine, or pediatric medicine. This definition is adopted from paragraph (I) of the definition of “primary care practitioner” in section 1833(x)(2)(A)(i) of the SSA. The Treasury Department and the IRS request comments on the definition of primary care physician and on the definition of direct primary care arrangement. In addition, the proposed regulations also invite comments about whether to expand the definition of a direct primary care arrangement to include a contract between an individual and a nurse practitioner, clinical nurse specialist, or physician assistant (as those terms are defined in section 1861(aa)(5) of the SSA) or other non-physician practitioner who provides primary care services under the contract and on how to define primary care services provided by a non-physician practitioner, including whether the definition of primary care services in section 1833(x)(2)(B) of the SSA is appropriate.
In addition, the Treasury Department and the IRS understand that other types of medical arrangements between health practitioners and individuals exist that do not fall within the definition of direct primary care. For example, an agreement between a dentist and a patient to provide dental care, or an agreement between a physician and a patient to provide specialty care, would not be a direct primary care arrangement but nonetheless may be the provision of medical care under section 213(d). The Treasury Department and the IRS request comments on whether the final regulations should clarify the treatment of other types of arrangements that are similar to direct primary care arrangements but do not meet the definition in the proposed regulations.
HCSM Definition
The proposed regulations draw their definition of a “health care sharing ministry” from section 5000A(d)(2)(B)(ii) of the Code, which provides that the individual shared responsibility payment (which is zero after December 31, 2018) does not apply to an individual who is a member of a health care sharing ministry. as an organization. To meet this HCSM definition, the organization must meet each of the following conditions:
- Described in section 501(c)(3) and is exempt from taxation under section 501(a);
- Members of which share a common set of ethical or religious beliefs and share medical expenses among members in accordance with those beliefs and without regard to the State in which a member resides or is employed;
- Members of which retain membership even after they develop a medical condition;
- Which (or a predecessor of which) has been in existence at all times since December 31, 1999, and medical expenses of its members have been shared continuously and without interruption since at least December 31, 1999; and
- Which conducts an annual audit which is performed by an independent certified public accounting firm in accordance with generally accepted accounting principles and which is made available to the public upon request. The Treasury Department and the IRS request comments on the definition of a health care sharing ministry.
Taxpayers and others dealing with HCSM should take particular note that the proposed regulations and its associated Code definition only address the tax consequences of HCSM and DPC arrangements and not their treatment for any other purpose of law. In this respect, it bears noting that the definition of HCSM in the Code is limited to only those arrangements that meet each of the criteria listed. In recent years, various state health insurance regulators have expressed concern that some arrangements promoted as HCSM do not meet all of the criteria required by the Code to qualify as HCSM, are sold or marketed as providing equivalent protection and coverage to regulated health insurance products and other reservations about the design and compliance of certain of these arrangements. Employers contemplating reimbursing these expenses should carefully evaluate the arrangements both for qualification under the Code and the prudence of any such arrangements. Likewise, individuals contemplating participation also are encouraged to carefully evaluate the arrangements both for their anticipated tax treatment and the reliability of the member’s expectations regarding coverage, eligibility, benefits, implications on eligibility for other insurance coverage, and other relevant concerns.
August 8, 2020 Comment/Request For Public Hearing Deadline
Business or individual taxpayers wishing to express support, opposition or other commentary on the proposed regulation should ensure that their written or electronic comments and requests for a public hearing are submitted in accordance with the procedures set forth in the notice of proposed rulemaking by the August 10, 2020 deadline.
More Information
We hope this update is helpful. For more information about the these or other health or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney recognized for her leading edge work on health benefit and other related employee benefit, insurance and health care concerns and policy matters.
Board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer, Ms. Stamer is widely known for 30+ years legal and operational management work, coaching, public policy and regulatory affairs leadership and advocacy, training and public speaking and publications. As a significant part of her work, Ms. Stamer has worked extensively domestically and internationally on an demand, special project and ongoing basis with business, government and community organizations and their leaders, spoken and published extensively on human resources, health and other employee benefits and other workforce and services, tax, health care and health benefits, insurance, workers’ compensation and occupational disease, business disaster and distress and many other management topics, As a key focus of this work, Ms. Stamer has worked with public and private employers of all sizes, employee benefit plans, insurance and financial services, health industry and a broad range of public and private domestic and international business, community and government organizations and leaders on pandemic and other health and safety, workforce and performance preparedness, risks and change management, disaster preparedness and response and other operational and tactical concerns throughout her adult life including extensive work both on the tax, health care, insurance and other policy and regulation, design, administration, defense and enforcement of DPC, HCSM, association health plan, mandate only, short-term limited benefit health insurance and other innovative health benefit, managed care, insurance and care arrangements. A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally and domestically as an advisor to business, community and government leaders on workforce, health care, insurance, benefits and other reform, as well as regularly advises and defends organizations about the design, administration and defense of their organizations workforce, employee benefit and compensation, safety, discipline and other management practices and actions. She has worked, spoken and published extensively on DPC, HCSM and other regulatory and statutory reforms impacting health benefits and health care including speaking on DPC and HCSM tax and other regulatory and enforcement policies on a program on Benefits for Small Employers presented for the American Bar Association Real Property Trusts and Estates Section on March 14, 2020.
Board Certified in Labor and Employment Law By the Texas Board of Legal Specialization, Scribe for the ABA JCEB Annual Agency Meeting with OCR, Vice Chair of the ABA International Section Life Sciences Committee, and the ABA RPTE Employee Benefits & Other Compensation Group and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and shares insights and thought leadership through her extensive publications and public speaking. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- Wish Tax Guidance Were Clearer? Tell IRS/Treasury Your Suggested Topics For 2020-2021 Treasury Priority Guidance Plan
- New IRS Increased Health FSA Carryover, Gives COVID Health FSA Election Relief
- IRS Shares Initial CARES Act Plan Loan & Distribution Relief Guidance
- Employer Sponsors & Health Plans Face Rising Risk From Mental Health & Substance Abuse Coverage Violations
- Use Prudent Process To Manage Workforce & Other Business Changes To Help Minimize Business & Management Liabilities & Protect Future Recovery
- Congress Expected To Pass COVID-19 Relief Bill With Paid Leave Mandates & Expanded Unemployment Funding This Week
- New Resources For Businesses, Employers, Schools & Homes To Stay Safe From COVID-19
- Self Insured Plan & Contract Amendments Likely Required To Waive Deductibles, Expand Other Coronavirus Coverage
- Health Plans, Providers & PBM Face Pressure To Prepare For Health Transparency As Trump Transparency Reforms March Foward
- Proposed HHS Rule Making PBM Expenses Part of MLS Administrative Expense, Other Changes To ACA Helath Plan Rules Comment Deadline 5 P.M. Today
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- New PBGC Pension Rules Effective 3/5 May Require Action On Retirement Plans
- Revise Health Plan HIPAA Records Access Rules & Procedures To Use Newly Flexibility On Charging, Responding To Third Party PHI Requests
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
- Salary Threshold Increases Require Employer Review Of Salaried Worker FLSA Exemption Qualification
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. ©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc. 
Wish Tax Guidance Were Clearer? Tell IRS/Treasury Your Suggested Topics For 2020-2021 Treasury Priority Guidance Plan
June 11, 2020Lack of clarity in current tax regulations or guidance creating headaches? The Department of the Treasury (“Treasury Department”) and the Internal Revenue Service (“IRS”) are inviting businesses and individuals to submit recommendations about what issues the 2020-2021 Priority Guidance Plan should include. Businesses and individuals with ideas about tax guidance needed to solve vexing issues should consider submitting their proposed guidance to the the Treasury Department and IRS in response to this invitation.
The Treasury Department’s Office of Tax Policy and the Service uses the Priority Guidance Plan each year to identify and prioritize the tax issues that tax regulations, revenue rulings, revenue procedures, notices, and other published administrative guidance should address during the year.
The 2020-2021 Priority Guidance Plan will identify guidance projects that the Treasury Department and the Service intend to actively work on as priorities during the period from July 1, 2020, through June 30, 2021.
In reviewing recommendations and selecting additional projects for inclusion on the 2020-2021 Priority Guidance Plan, the Treasury Department and the Service will consider the following:
- Whether the recommended guidance resolves significant issues relevant to a broad class of taxpayers;
- Whether the recommended guidance reduces controversy and lessens the burden on taxpayers or the Service;
- Whether the recommended guidance relates to recently enacted legislation;
- Whether the recommendation involves existing regulations or other guidance that is outdated, unnecessary, ineffective, insufficient, or unnecessarily burdensome and that should be modified, streamlined, expanded, replaced, or withdrawn;
- Whether the recommended guidance would be in accordance with Executive Order 13771 (82 FR 9339), Executive Order 13777 (82 FR 12285), Executive Order 13789 (82 FR 19317), or other executive orders.
- Whether the recommended guidance promotes sound tax administration;
- Whether the Service can administer the recommended guidance on a uniform basis; and
- Whether the recommended guidance can be drafted in a manner that will enable taxpayers to easily understand and apply the guidance.
While suggestions are submitted throughout the year, Notice 2020-47 encourages individuals or businesses desiring to propose issues or other content to be included in the 2020-2021 Priority Guidance to submit their recommendations for guidance by Wednesday, July 22, 2020, for possible inclusion on the original 2020-2021 Priority Guidance Plan. Taxpayers are not required to submit recommendations for guidance in any particular format. Taxpayers should, however, briefly describe the recommended guidance and explain the need for the guidance. In addition, taxpayers may include an analysis of how the issue should be resolved. For recommendations to modify, streamline, or withdraw existing regulations or other guidance, taxpayers should explain
how the changes would reduce taxpayer cost and/or burden or benefit tax administration.
Notice 20-47 also states that taxpayers suggesting more than one guidance project prioritize the projects by order of importance. If a large number of projects are being suggested, it would be helpful if the projects were grouped by subject matter and then in terms of high, medium, or low priority. Requests for guidance in the form of petitions for rulemaking will be considered with other recommendations for guidance in accordance with the considerations described in Notice 2020-47.
More Information
We hope this update is helpful. For more information about the these or other health or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years legal and operational management work, coaching, public policy and regulatory affairs leadership and advocacy, training and public speaking and publications. As a significant part of her work, Ms. Stamer has worked extensively domestically and internationally on an demand, special project and ongoing basis with business, government and community organizations and their leaders, spoken and published extensively on human resources, employee benefits and other workforce and services, tax, health care and health benefits, insurance, workers’ compensation and occupational disease, business disaster and distress and many other management topics, As a key focus of this work, Ms. Stamer has worked with public and private employers of all sizes, employee benefit plans, insurance and financial services, health industry and a broad range of public and private domestic and international business, community and government organizations and leaders on pandemic and other health and safety, workforce and performance preparedness, risks and change management, disaster preparedness and response and other operational and tactical concerns throughout her adult life. A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally as an advisor to business, community and government leaders on crisis preparedness and response, workforce, health care and other reform, as well as regularly advises and defends organizations about the design, administration and defense of their organizations workforce, employee benefit and compensation, safety, discipline and other management practices and actions.
Board Certified in Labor and Employment Law By the Texas Board of Legal Specialization, Scribe for the ABA JCEB Annual Agency Meeting with OCR, Vice Chair of the ABA International Section Life Sciences Committee, and the ABA RPTE Employee Benefits & Other Compensation Group and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and shares insights and thought leadership through her extensive publications and public speaking. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- New IRS Increased Health FSA Carryover, Gives COVID Health FSA Election Relief
- IRS Shares Initial CARES Act Plan Loan & Distribution Relief Guidance
- Employer Sponsors & Health Plans Face Rising Risk From Mental Health & Substance Abuse Coverage Violations
- Use Prudent Process To Manage Workforce & Other Business Changes To Help Minimize Business & Management Liabilities & Protect Future Recovery
- Congress Expected To Pass COVID-19 Relief Bill With Paid Leave Mandates & Expanded Unemployment Funding This Week
- New Resources For Businesses, Employers, Schools & Homes To Stay Safe From COVID-19
- Self Insured Plan & Contract Amendments Likely Required To Waive Deductibles, Expand Other Coronavirus Coverage
- Health Plans, Providers & PBM Face Pressure To Prepare For Health Transparency As Trump Transparency Reforms March Foward
- Proposed HHS Rule Making PBM Expenses Part of MLS Administrative Expense, Other Changes To ACA Helath Plan Rules Comment Deadline 5 P.M. Today
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- New PBGC Pension Rules Effective 3/5 May Require Action On Retirement Plans
- Revise Health Plan HIPAA Records Access Rules & Procedures To Use Newly Flexibility On Charging, Responding To Third Party PHI Requests
- 2/28 New Comment Deadline For NLRB Proposal To Exclude College Work Study Student Workers From NLRA Coverage
- Don’t Get Stuck Paying Another Employer’s Overtime Or Other Backpay
- 2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
- DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- Business Leaders Serve Jail Time For Employment Tax Crimes
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. ©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc. 
New IRS Increased Health FSA Carryover, Gives COVID Health FSA Election Relief
June 11, 2020IRS Notice 2020-33 released indexing the permissible health FSA carryover. As a consequence, the permissible amount immediately increases from $500 to $550.
IRS Notice 2020-29 released to provide temporary flexibility under cafeteria plans for new or changed health coverage and dependent care and health FSA elections, and extensions in certain circumstances of claims periods before use-or-lose must be applied, in response to the changed circumstances many have experienced with respect to availability of childcare and availability of elective health procedures. And a few other HDHP nuggets in there as well.
More Information
We hope this update is helpful. For more information about the these or other health or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years legal and operational management work, coaching, public policy and regulatory affairs leadership and advocacy, training and public speaking and publications. As a significant part of her work, Ms. Stamer has worked extensively domestically and internationally on an demand, special project and ongoing basis with business, government and community organizations and their leaders, spoken and published extensively on human resources, employee benefits and other workforce and services, tax, health care and health benefits, insurance, workers’ compensation and occupational disease, business disaster and distress and many other management topics, As a key focus of this work, Ms. Stamer has worked with public and private employers of all sizes, employee benefit plans, insurance and financial services, health industry and a broad range of public and private domestic and international business, community and government organizations and leaders on pandemic and other health and safety, workforce and performance preparedness, risks and change management, disaster preparedness and response and other operational and tactical concerns throughout her adult life. A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally as an advisor to business, community and government leaders on crisis preparedness and response, workforce, health care and other reform, as well as regularly advises and defends organizations about the design, administration and defense of their organizations workforce, employee benefit and compensation, safety, discipline and other management practices and actions.
Board Certified in Labor and Employment Law By the Texas Board of Legal Specialization, Scribe for the ABA JCEB Annual Agency Meeting with OCR, Vice Chair of the ABA International Section Life Sciences Committee, and the ABA RPTE Employee Benefits & Other Compensation Group and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and shares insights and thought leadership through her extensive publications and public speaking. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- IRS Shares Initial CARES Act Plan Loan & Distribution Relief Guidance
- Employer Sponsors & Health Plans Face Rising Risk From Mental Health & Substance Abuse Coverage Violations
- Use Prudent Process To Manage Workforce & Other Business Changes To Help Minimize Business & Management Liabilities & Protect Future Recovery
- Congress Expected To Pass COVID-19 Relief Bill With Paid Leave Mandates & Expanded Unemployment Funding This Week
- New Resources For Businesses, Employers, Schools & Homes To Stay Safe From COVID-19
- Self Insured Plan & Contract Amendments Likely Required To Waive Deductibles, Expand Other Coronavirus Coverage
- Health Plans, Providers & PBM Face Pressure To Prepare For Health Transparency As Trump Transparency Reforms March Foward
- Proposed HHS Rule Making PBM Expenses Part of MLS Administrative Expense, Other Changes To ACA Helath Plan Rules Comment Deadline 5 P.M. Today
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- New PBGC Pension Rules Effective 3/5 May Require Action On Retirement Plans
- Revise Health Plan HIPAA Records Access Rules & Procedures To Use Newly Flexibility On Charging, Responding To Third Party PHI Requests
- 2/28 New Comment Deadline For NLRB Proposal To Exclude College Work Study Student Workers From NLRA Coverage
- Don’t Get Stuck Paying Another Employer’s Overtime Or Other Backpay
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. ©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc. 
.
IRS Shares Initial CARES Act Plan Loan & Distribution Relief Guidance
May 5, 2020Section 2202 of the Coronavirus Aid, Relief, and Economic Security Act (CARES Act), enacted on March 27, 2020, provides for special distribution options and rollover rules for retirement plans and IRAs and expands permissible loans from certain retirement plans.
While it anticipates issuing further guidance, the Internal Revenue Service (“IRS”) on May 4 provided preliminary guidance in question and answer format titled Coronavirus-related relief for retirement plans and IRAs questions and answers.
More Information
We hope this update is helpful. For more information about the these or other health or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years legal and operational management work, coaching, public policy and regulatory affairs leadership and advocacy, training and public speaking and publications. As a significant part of her work, Ms. Stamer has worked extensively domestically and internationally on an demand, special project and ongoing basis with business, government and community organizations and their leaders, spoken and published extensively on human resources, employee benefits and other workforce and services, tax, health care and health benefits, insurance, workers’ compensation and occupational disease, business disaster and distress and many other management topics, As a key focus of this work, Ms. Stamer has worked with public and private employers of all sizes, employee benefit plans, insurance and financial services, health industry and a broad range of public and private domestic and international business, community and government organizations and leaders on pandemic and other health and safety, workforce and performance preparedness, risks and change management, disaster preparedness and response and other operational and tactical concerns throughout her adult life. A former lead advisor to the Government of Bolivia on its pension project, Ms. Stamer also has worked internationally as an advisor to business, community and government leaders on crisis preparedness and response, workforce, health care and other reform, as well as regularly advises and defends organizations about the design, administration and defense of their organizations workforce, employee benefit and compensation, safety, discipline and other management practices and actions.
Board Certified in Labor and Employment Law By the Texas Board of Legal Specialization, Scribe for the ABA JCEB Annual Agency Meeting with OCR, Vice Chair of the ABA International Section Life Sciences Committee, and the ABA RPTE Employee Benefits & Other Compensation Group and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also serves in leadership of a broad range of professional and civic organizations and shares insights and thought leadership through her extensive publications and public speaking. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- Proposed HHS Rule Making PBM Expenses Part of MLS Administrative Expense, Other Changes To ACA Health Plan Rules Comment Deadline 5 P.M. Today
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- New PBGC Pension Rules Effective 3/5 May Require Action On Retirement Plans
- Revise Health Plan HIPAA Records Access Rules & Procedures To Use Newly Flexibility On Charging, Responding To Third Party PHI Requests
- 2/28 New Comment Deadline For NLRB Proposal To Exclude College Work Study Student Workers From NLRA Coverage
- Don’t Get Stuck Paying Another Employer’s Overtime Or Other Backpay
- 2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
- DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
- OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
- Salary Threshold Increases Require Employer Review Of Salaried Worker FLSA Exemption Qualification
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here. ©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc. 
Employer Sponsors & Health Plans Face Rising Risk From Mental Health & Substance Abuse Coverage Violations
March 20, 2020Employer and union-sponsored health plans, their sponsors, fiduciaries and administrators should heed the reminder of the importance of ensuring their health plans properly comply in form and operation with the mental health and substance abuse parity mandes of the Mental Health Parity and Addiction Equity Act (MHPAEA) in when the U.S. Department of Labor (“DOL”) Employee Benefit Security Administration (“EBSA”) released its 2020 Report to Congress: Parity Partnerships: Working Together (the”2020 Report”) available for review here.
In addition to exposing the health plan administrators and othr fiduciaries to potential claims denial or fiduciary responsibility claims brought by participants or beneficiaries, the Department of Labor or both, administrative penalties by the EBSA, or both, the MHPAEA mental health and substance abuse parity rules are among 40 federal mandates that when violated can rigger the automatic $100 per violation per day employer excise tax penalty under Internal Revenue Code Section 6039D. As a consequence, violations of the MHPAEA are particularly risky and potentially expensive for private employers, their health plans and the plan administrators and fiduciaries that administer it.
To avoid violation of the MHPAEA, covered health plans generally must cover mental health and substance abuse care and treatment on the same terms in form and in operation as other similar benefits, as well as comply with special notice and claims administration requirements. Comparability of mental health and substance abuse coverage is determined in accordance with complicated federal regulations, Meeting these requirements in operations is often tricky, particularly when health plans attempt to apply tools to manage hospitalization or other treatments. For additional information about MHPAEA, C. Stamer, What Should I Know About the MHPAEA and 21st Century Cures Act (2018).
Along with the 2020 Report, Along with releasing the report, EBSA also is continuing its efforts to educate plan sponsors, fiduciaries, administrators about the importance of compliance with the federally imposed group health plan mental health and substance abuse coverage mandates of the Mental Health Parity and Addiction Equity Act (“MHPAEA”). Consequently, along with its release of the 2020 Report, EBSA reminded plans, employers and other interested parties of the following previously published EBSA guidance about the MHPAEA mandates:
- FY 2019 Mental Health Parity and Addiction Equity Act (MHPAEA) Enforcement Fact Sheet, available at https://www.dol.gov/sites/dolgov/files/EBSA/laws-and-regulations/laws/mental-health-parity/mhpaea-enforcement-2019.pdf
- Appendix to FY 2019 MHPAEA Enforcement Fact Sheet, available at https://www.dol.gov/sites/dolgov/files/EBSA/laws-and-regulations/laws/mental-health-parity/mhpaea-enforcement-2019-fact-sheet-appendix.pdf
MHPAEA Enforcement Authority
MHPAEA enforcement is split between the EBSA and the Department of Health & Human Services Centers for Medicare & Medicaid Services (“CMS”) depending on the nature and sponsorship of the health program.
Pursuant to its enforcement authority under Title I of the Employee Retirement Income Security Act of 1974 (ERISA), EBSA is responsible for enforcement of the MHPAEA with respect to approximately 2.4 million private employment-based group health plans. In contrast, CMSenforces MHPAEA and other applicable provisions of Title XXVII of the Public Health Service Act (PHS Act) with respect to non-federal governmental group health plans, such as plans for employees of state and local governments. Sponsors of self-funded, nonfederal governmental plans may elect to exempt those plans from (opt out of) certain requirements of Title XXVII of the PHS Act, including MHPAEA. In addition, CMS enforces MHPAEA with respect to health insurance issuers selling products in the individual and fully insured group markets in states that elect not to enforce or fail to substantially enforce MHPAEA. Currently, CMS is responsible for enforcement of MHPAEA with regard to issuers in four states: Missouri, Oklahoma, Texas and Wyoming. In these states, CMS reviews health insurance policy forms of issuers in the individual and group markets for compliance with MHPAEA prior to the products being offered for sale. In addition, CMS has collaborative enforcement agreements with five states: Alabama, Florida, Louisiana, Montana, and Wisconsin. These states perform state regulatory and oversight functions with respect to the federal requirements, including MHPAEA. However, if the state finds a potential violation and is unable to obtain compliance by an issuer, the state will refer the matter to CMS for possible enforcement action. CMS also performs market conduct examinations, where issuers are audited for compliance with applicable federal requirements, including MHPAEA, in states where CMS is responsible for enforcement and in states with a collaborative enforcement agreement when the state requests assistance.
EBSA FY 2019 Enforcement Against Private Employment Based Health Plans
The Fiscal Year (“FY”) 2019 Fact Sheet reports that in FY 2019, EBSA investigated and closed 186 health plan investigations in FY 2019 (and 3,758 health plan investigations since FY 2011). Of these:
- 71 investigations involved fully-insured plans, 91 investigations involved self-insured plans, and
- 24 investigations involved plans of both types (the plan or service provider offered both fully-insured and self-insured options).
- 183 of these closed investigations involved plans subject to MHPAEA, which were reviewed for MHPAEA compliance. Of these, 68 investigations involved fully-insured plans, 91 investigations involved self-insured plans, and 24 investigations involved plans of both types (the plan or service provider offered both fully-insured and self-insured options).
- EBSA cited 12 MHPAEA violations in 9 of these investigations.
- Of these 9 investigations, 1 investigation involved a fully-insured group health plan, 3 investigations involved self-funded group health plans, 2 investigations involved partially self-funded group health plans and 3 were service provider investigations.
- EBSA benefits advisors answered 90 public inquiries, including 62 complaints, in FY 2019 related to MHPAEA (and answered 1,445 inquiries related to MHPAEA since FY 2011)
Concerning the focus of the EBSA investigated MHPAEA violations, EBSA reports the investigations focused on the following categories:
- Annual dollar limits: dollar limitations on the total amount of specified benefits that may be paid in a 12-month period under a group health plan or health insurance coverage for any coverage unit (such as self-only or family coverage).
- Aggregate lifetime dollar limits: dollar limitations on the total amount of specified benefits that may be paid under a group health plan or health insurance coverage for any coverage unit.
- Benefits in all classifications: requirement that if a plan or issuer provides mental health or substance use disorder benefits in any classification described in the MHPAEA final regulation, mental health or substance use disorder benefits must be provided in every classification in which medical/surgical benefits are provided.
- Financial requirements: deductibles, copayments, coinsurance, or out-of-pocket maximums.
- Treatment limitations: includes limits on benefits based on the frequency of treatment, number of visits, days of coverage, days in a waiting period, or other similar limits on the scope or duration of treatment. Treatment limitations include both quantitative treatment limitations (QTLs), which are expressed numerically (such as 50 outpatient visits per year), and nonquantitative treatment limitations (NQTLs), which otherwise limit the scope or duration of benefits for treatment under a plan or coverage.
- Cumulative financial requirements and QTLs: financial requirements and treatment limitations that determine whether or to what extent benefits are provided based on certain accumulated amounts including deductibles, out-of-pocket maximums and annual or lifetime day or visit limits.
- Other ERISA violations (such as claims processing and disclosure violations) affecting mental health and substance use disorder benefits.
Along with the EBSA enforcement, private participants and beneficiaries of private employer sponsored health plans also can bring lawsuits to recover benefits and other relief for violatons of MHPAEA. Along with the actual damages, attorneys’ fees and other costs of enforcement, a successful MHPAEA enforcement also typically will reveal the sponsoring employer or union’s failure to make the required self-disclosure and excise tax payments mandated for violations under Internal Revenue Code Section 6039D, triggering added penalties beyond the initial penalties triggered by the uncorrected violation. Furthermore, delayed discovery of these violations also makes correction particularly costly for self-insured plans and their sponsors as deadlines for submitting expenses to qualify for stop loss reimbursement often will have passed by the time the liability comes to light. Accordingly, employer and other health plan sponsors, their fiduciaries and adminstrators generally will want to audit and monitor their health plan’s compliance with the MHPAEA throught the calendar year and as plan year or stop loss filing deadlines approach to mitigate these exposures.
More Information
We hope this update is helpful. For more information about the these or other health or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of health industry and other management work, public policy leadership and advocacy, coaching, teachings, and publications. As a significant part of her work, Ms. Stamer has worked extensively domestically and internationally with business, government and community leaders to prepare for and deal with pandemic and other health and safety, financial, workforce and other organizational crisis, change and workforce, employee benefit, health care and other operations planning, preparedness and response for more than 30 years. As a part of this work, she regularly advises businesses and government leaders on an an demand and ongoing basis about preparation of workforce, health care and other business and government policies and practices to deal with management in a wide range of contexts ranging from day to day operations, through times of change and in response to operational, health care, natural disaster, economic and other crisis and change.
Author of “Privacy and the Pandemic Workshop” for the Association of State and Territorial Health Plans, “How to Conduct A Reduction In Force,” and a multitude of other highly regarded publications and presentations on workforce, compliance, health care and health benefits, pandemic and other health crisis, workers’ compensation and occupational disease, business disaster and distress and many other topics, Ms. Stamer has worked with employers, insurers, health industry organizations and providers and domestic and international community and government leaders on pandemic and other health and safety, workforce and performance preparedness, risks and change management, disaster preparedness and response and other operational and tactical concerns throughout her adult life. A former lead advisor to the Government of Bolivia on its pension privaitization project, Ms. Stamer also has worked internationally as an advisor to business, community and government leaders on crisis preparedness and response, workforce, health care and other reform, as well as regularly advises and defends organizations about the design, administration and defense of their organizations workforce, employee benefit and compensation, safety, discipline and other management practices and actions.
Board Certified in Labor and Employment Law By the Texas Board of Legal Specialization, Scribe for the ABA JCEB Annual Agency Meeting with OCR, Vice Chair of the ABA International Section Life Sciences Committee, and the ABA RPTE Employee Benefits & Other Compensation Group and and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her extensive publications and thought leadership as well as leadership involvement in a broad range of other professional and civic organizations. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- Proposed HHS Rule Making PBM Expenses Part of MLS Administrative Expense, Other Changes To ACA Helath Plan Rules Comment Deadline 5 P.M. Today
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- New PBGC Pension Rules Effective 3/5 May Require Action On Retirement Plans
- Revise Health Plan HIPAA Records Access Rules & Procedures To Use Newly Flexibility On Charging, Responding To Third Party PHI Requests
- 2/28 New Comment Deadline For NLRB Proposal To Exclude College Work Study Student Workers From NLRA Coverage
- Don’t Get Stuck Paying Another Employer’s Overtime Or Other Backpay
- 2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
- DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
- OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
- Salary Threshold Increases Require Employer Review Of Salaried Worker FLSA Exemption Qualification
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
Use Prudent Process To Manage Workforce & Other Business Changes To Help Minimize Business & Management Liabilities & Protect Future Recovery
March 16, 2020The financial effects of the COVID-19 pandemic and containment efforts has many businesses flailing to reconfigure their staffing and other business models even as Congress is preparing to impose paid COVID related leave mandate on employers with less than 500 employees. With the sharp falloff in business threatening their current liquidity and operations, many business leaders understandably feel pressure to substantially reduce their workforces or make other radical changes in business operations to stem their business’ resulting COVID-19 created financial crisis. When choosing and implementing their options, however, business leaders should carefully weigh all of their options and use care when designing and implementing their workforce and other business adjustments strategically to best position their businesses to survive the current crisis without triggering unanticipated employment, employee benefit, compensation or other liabilities as well as to best position their organizations and its leaders to retain the trust and respect their business will need to regain the customer, vendor, workforce and other business respect and loyalty their business will need to recover once the crisis has past.
Many business owners and leaders understandably feel the COVID-driven economic downturn forces them to act quickly to implement workforce reductions, close plants, or shut down all or portions of their business operations. Where a distressed business contemplates a plant closing, mass layoff or other substantial change, however, the business and its leaders need to fully understand the various financial and legal effects and costs of the proposed workforce and other business changes and act strategically to manage their resulting obligations and obligations. Businesses owners and leaders dealing with these issues are invited to check out the COVID-19 Workforce Change Planning & Implementation Process Flow tool and other resources available here.
While financial and other business exigencies unquestionably makes speedy action critical for many businesses, owners and management need to recognize that poorly chosen or improperly implemented strategies or actions raises significant risks that unanticipated costs and liabilities will undermine or wipe out anticipated benefits of the contemplated actions, undermine, the business future recovery opportunities, expose the business, its ownership and management to substantial liability and other risks.
While the current economic freefall may tempt many business leaders to see shutting down their operations or other mass layoffs as the best option for protecting their businesses, it is important to keep in mind that layoffs and other employment terminations as well as early terminations of other services contracts typically trigger legal and finanncial exposures. Businesses leaders need to recognize and account for these obligations and their financial and operational costs when weighing their options and plan to manage the obligations and costs and other liabilities when implementing the strategy chosen by their business. This can be particularly important where a realistic likelihood exists that the business may file for bankrutpcy protection and/or fail to meet certain of these obligations as some obligations may create personal liability for business owners or leaders if not fulfilled by the company.
When anticipating or executing potential employment terminations, businesses and their leaders should recognize and address properly the employment, unemployment, employee benefit, compensation and other responsibilities attendant to any employment termination. Whether planning to furlow workers for a short period or planning a longer term layoff or shutdown, businesses leaders must fully understand their probable fixed obligations including any accellerated or added liabilities and costs likely to be triggered by the workforce action. Accordingly businesses should prepare to handle the fallout from COVID-19 impacts to their workforce and other business operations by on their existing or contemplated voluntarily imposed and legally mandated employment, compensation, benefit, safety, contractual and other related obligations obligations.
While planning for workforce or other actions, businesses and leaders also should are urged to confirm the availability of their cash flow to meet current requirements to timely fund payroll and associated taxes, health, disability and defined benefit pension, and other costs where nonpayment or untimely payment carries substantial entity and/or personal exposure to penalties or other liabilities likely to survive bankruptcy or other restructuring. In the case of health and pension benefit liabilities, for instance, nonpayment of premiums and other required funding could carry fiduciary liability for business owners, board members and other management with responsibility or discretion over these programs and their funding. Accordingly, if a business anticipates any risk of inability to fund already accrued or impending funding obligations, management should contact experienced legal counsel for immediate assistance with addressing these potential risks.
Additionally, businesses and their leaders contemplating offering special leave to workers absent or furloughed during leave need to take into account and handle properly both applicable federal, state and local mandated benefits and other rights, the legal requirements for adopting and implementing paid or other voluntarily provided leave, the benefit benefit, recall and other rights of workers terminated, furloughed or absent due COVID-related illness or other events.
COVID-19 Related Since Leave Or Other Absences From Ongoing Workforce
Regardless of whether a business plans additional workforce changes, all businesses need to be prepared to deal with absences resulting from contractions or exposures of COVID-19 by employees or their families or other COVID-19 associated absences.
Employees taking voluntary or involuntary leave likely already are entitled to certain paid or unpaid leave and associated benefit, reinstatement and other rights under a hodgepodge of voluntarily established company policies and other federal, state and even local regulations. Beyond any existing accrued rights to paid or unpaid leave due an employee under voluntary company policies and/or federal, state or local mandates, businesses need to understand and be prepared to meet their obligations to provide continued health benefit coverage and reinstatement to benefits as mandated by the Family & Medical Leave Act (“FMLA”) for FMLA covered workers, health plan continuation coverage rights for employees experiencing reductions in hours triggering losses of health plan eligibility as required by the Consolidated Omnibusiness Budget Reconciliation Act (“COBRA”). These obligations are expected to be expanded later this week if the “Families First Coronavirus Response Act,” (H.R. 6201) passed by the House of Representatives last week passes the Senate and is signed into law by President Trump as expeted later this week as part of efforts to mitigate impacts of disruptions of the COVID-19 containment disruptions. While H.R. 6201 is expected to include tax credits for employers to help mitigate the financial effects of its paid leave mandates for covered employers, employers will want to understand and take into account these requirements and the potential tax credits when deciding what leave to offer beyond the mandated paid leave and properly plan for, anticipate costs of and integrate those obligations with their other leave obligations.
Aside from the likely increase in the frequency of the occurence of these usual employment absence, termination, unemployment, compensation, and benefit liabilities and costs, businesses planning or contemplating some or all of their employees will termiinate employment due to long-term illnesses, employer layoffs or other COVID-related events need to anticipate and prepare to deal with other likely additional consequences. For instance:
- Illness and other absences generally trigger added potential exposure for discrimination, retaliation, privacy and other employment claims and risks if not properly recognized and managed;
- The selection and implementation of workers to be affected by furloughs, layoffs and other workforce actions should be conducted carefully to manage potential Relatively small declines in the size of a business’ workforce can trigger pricing changes or even termination rights for vendors providing coverage or services for group health or other insurance, stop-loss insurance coverage on self-insured health plans or other human resources, payroll, benefits or other related services or coverage;
- Changes in workforce size and compensation can affect whether an employer sponsored health, 401(k) or other savings or retirement plan or other benefit program fulfills applicable coverage, participation and nondiscrimination requirements resulting in tax consequences for the employer and in some instances, key or highly compensated employees, obigations for the business to make additional funding contributions, in the case of employers with health plans covered by Internal Revenue Code Section 4980H, mandatory contributions for health insurance exchange coverage for uncovered employees or other consequences.
- Reductions in hours or terminations of employment that reduce participation in 401(k) and other savings or retirement programs by 20 percent or more generally trigger obligations to fully vest and for retirement plans, accellerate funding of benefts of terminating workers under the “partial termination” rules applicable to those programs.
- Severance, paid or unpaid leave, and other arrangements voluntarily adopted in response to the COVID-19 disruptions or covered by other voluntarily adopted programs or practices need to be appropriately documented and administered in accordance with the Employee Retirement Income Security Act (“ERISA”) or other applicable federal law as well as properly integrated with other federal, state, and local leave or other mandates to manage unanticipated costs and avoid unanticipated fiduciary and financial liability for the business, its management or both.
- Financial disruptions that prevent a business from timely making required contributions to fund defined benefit or other pension plans insured by the Pension Benefit Guarantee Corporation can trigger funding notice, excise tax penalty and other obligations for the employer and its fiduciaries.
- For certain employers, reductiions of all or a significant portion of a workforce companywide or at certain locations by a distressed or other business usually triggers a host of special obligations and attendant costs for businesses. Businesses anticipating these changes need to take into account the financial costs and legal obligations and expossures of proposed workforce or other actions and where applicable, make appropriate arrangements to comply or implement their workforce and other business restructurings to restructuring to minimize and meet these obligations.
Of course, For instance, layoffs and other reductions in force or closings by businesses often trigger a host of legal and financial obligations. at certain businesses or business locations often trigger obligations to provide advance notifications under the Worker Adjustment and Retraining Notification Act (WARN) or other statutes or contracts. Where these obligations are triggered, the business not only will need to arrange to provide required notitications but also needs to take into account their business’ likely financial exposure for payment of pay in lieu of notice or other costs and liability arising from the employment. WARN, business contemplating or implementing a plan closing, mass layoff or other reductions in force also should evaluate and make appropriate arrangements to address potential obligations under state plant closing laws, the ARRA Stimulus Bill Extension Rules amended and extended earlier this month and other requirements of COBRA, voluntary or contractually obligated termination pay or other severance obligations, employee benefit, unemployment, and other laws.
The COVID-19 Workforce Change Planning & Implementation Process Flow tool provides an overview of the type of process flow tthat business owners and leaders dealing with these issues may find useful to help guide their process for planning their business’ workforce management response to the unexpected business exigencies created by the ongoing COVID-19 outbreak.
For More Information
We hope this update is helpful. For more information about this or other labor and employment developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Law and Labor and Employment Law and Health Care; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of health industry and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Ms. Stamer’s work throughout her 30 plus year career has focused heavily on working with health care and managed care, health and other employee benefit plan, insurance and financial services, construction, manufacturing, staffing and workforce and other public and private organizations and their technology, data, and other service providers and advisors domestically and internationally with legal and operational compliance and risk management, performance and workforce management, regulatory and public policy and other legal and operational concerns. As a part of this work, she has continuously and extensively worked with domestic and international employer and other management, employee benefit and other clients to assess, manage and defend joint employer and other worker classifications and practices under the FLSA and other federal and state laws including both advising and and assisting employers to minimize joint employer and other FLSA liability and defending a multitude of employers against joint employer and other FLSA and other worker classification liability. She also has been heavily involved in advocating for the Trump Administration’s restoration of more historical principles for determining and enforcing joint employer liability over the past several years.
Author of hundreds of highly regarded books, articles and other publications, Ms. Stamer also is widely recognized for her scholarship, coaching, legislative and regulatory advocacy, leadership and mentorship on wage and hour, worker classification and a diverse range of other labor and employment, employee benefits, health and safety, education, performance management, privacy and data security, leadership and governance, and other management concerns within the American Bar Association (ABA), the International Information Security Association, the Southwest Benefits Association, and a variety of other international, national and local professional, business and civic organizations including highly regarded works on worker reclassification and joint employment liability under the FLSA and other laws published by the Bureau of National Affairs and others. Examples of these involvements include her service as the ABA Intellectual Property Law Section Law Practice Management Committee; the ABA International Section Life Sciences and Health Committee Vice Chair-Policy; a Scribe for the ABA Joint Committee on Employee Benefits (JCEB) Annual OCR Agency Meeting and a former JCEB Council Representative and Marketing Chair; Past Chair of the ABA RPTE Employee Benefits and Other Compensation Group and Vice Chair of its Law Practice Management Committee; Past Chair of the ABA Managed Care & Insurance Interest Group; former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Southwest Benefits Association Board member; past Texas Association of Business State Board Member, BACPAC Committee Meeting, Regional and Dallas Chapter Chair; past Dallas Bar Association Employee Benefits Committee Executive Committee; former SHRM Region IV Chair and National Consultants Forum Board Member; for WEB Network of Benefit Professionals National Board Member and Dallas Chapter Chair; former Dallas World Affairs Council Board Member; founding Board Member, past President and Patient Empowerment and Health Care Heroes founder for the Alliance for Health Care Excellence; former Gulf States TEGE Council Exempt Organizations Coordinator and Board member; past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and involvement in a broad range of other professional and civic organizations. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- 2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
- DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
- OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- Comment on Interim Domestic Hemp Production Rules By 12/30n. L ok
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
- Salary Threshold Increases Require Employer Review Of Salaried Worker FLSA Exemption Qualification
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The author and Solutions Law Press, Inc. disclaim, and have no responsibility to provide any update or otherwise notify anyone any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
Congress Expected To Pass COVID-19 Relief Bill With Paid Leave Mandates & Expanded Unemployment Funding This Week
March 15, 2020U.S. employers need to prepare for their likely need to deal with paid family medical leave, paid sick leave, unemployment insurance and other employer impacting provisions of the “Families First Coronavirus Response Act,” (H.R. 6201) passed by the House of Representatives last week and expected to pass the Senate in some form this week as part of Congressional efforts to mitigate impacts of disruptions of the COVID-19 containment disruptions. Since the paid leave mandates would take effect 15 days from enactment, employers will want to prepare to comply and take into account the likely mandates when planning and communicating with workers and dealing with other financial and operational disruptions from the crisis.Solutions Law Press, INC. is planning to host a briefing for employers on the requirements after passed by Congress. For an invitation, register at http://www.solutiinslawpress.com or email here.
Paid Family Medical Leave
As passed by the House, the paid leave requirements currently only apply to employers with fewer than 500 employees and are accompanied by tax credit provisions intended to help covered businesses pay the cost of compliance. The bill’s paid leave requirements add special job-protected paid leave to the Family and Medical Leave Act (FMLA) for employees who have been working for at least 30 calendar days. In particular, covered employees would be entitled to 12 weeks of paid family leave, of which the first 14 days may be unpaid, to respond to quarantine requirements or recommendations, to care for family members who are responding to quarantine requirements or recommendations, and to care for a child whose school has been closed as a result of the COVID-19 pandemic (“COVID Leave”). The bill also provides employees may. but employers can’t require employees to use accrued personal or sick leave during the first 14 days. After the initial 14 days, covered employers must compensate employees in an amount that is not less than two-thirds of the employee’s regular rate of pay. Because the leave is FMLA covered, employers should expect to be required to continue health coverage during the leave at usual employee contribution rates and to reinstate the employee to their position with all benefits and employment rights and seniority upon timely return. The provisions will take effect 15 days after the date of enactment and expire on December 31, 2020.
Paid Sick Leave
Employers with fewer than 500 employees will be required to provide full-time employees 2 weeks (80 hours) of paid sick leave for COVID-19 specific circumstances related to COVID-19 such as self-isolating, doctors’ visits or the like. Part-time employees would be entitled to the number of hours of paid sick time equal to the average number of hours worked over a 2-week period.
Employers must pay employees for any paid sick time taken at their regular rates of pay and will be required to post a notice informing employees of their rights to leave.
Since the bill expressly does not, as currently drafted, the bill expressly provides that it does not preempt existing state or local paid sick leave entitlements, employers also could face additional requirements under state or local law.
Like the COVID leave, these provisions also will go into effect 15 days after the date of enactment and expire on December 31, 2020.
Unemployment Insurance
The bill also includes $1 billion in emergency unemployment insurance (UI) relief to the states: $500 million for costs associated with increased administration of each state’s unemployment insurance (“UI”) program and places $500 million in reserve to help states with a 10 percent increase in unemployment. To receive a portion of this grant money, states mustveclerience the required increase in unemployment and temporarily ease certain UI eligibility requirements, such as waiting periods and work search requirements.
Prospects For Enactment
Although some Senators raised questions about certain provisions of the bill, it is expected to pass in some form this week as Congress and the Administration rush to provide relief for workers and business impacted by the economic effects of the COVID-18 pandemic containment efforts. Accordingly, covered employers should expect Congress to pass and President Trump to sign the bill this week. Meanwhile all employers also should brace for added legislation and regulation as well as continued operational and financial disruption as the COVID-19 virus impacts continue to roll out across the U.S. and around the World.
More Information
We hope this update is helpful. For more information about the these or other health or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of health industry and other management work, public policy leadership and advocacy, coaching, teachings, and publications. As a significant part of her work, Ms. Stamer has worked extensively domestically and internationally with business, government and community leaders to prepare for and deal with pandemic and other health and safety, financial, workforce and other organizational crisis, change and workforce, employee benefit, health care and other operations planning, preparedness and response for more than 30 years. As a part of this work, she regularly advises businesses and government leaders on an an demand and ongoing basis about preparation of workforce, health care and other business and government policies and practices to deal with management in a wide range of contexts ranging from day to day operations, through times of change and in response to operational, health care, natural disaster, economic and other crisis and change.
Author of “Privacy and the Pandemic Workshop” for the Association of State and Territorial Health Plans, “How to Conduct A Reduction In Force,” and a multitude of other highly regarded publications and presentations on workforce, compliance, health care and health benefits, pandemic and other health crisis, workers’ compensation and occupational disease, business disaster and distress and many other topics, Ms. Stamer has worked with employers, insurers, health industry organizations and providers and domestic and international community and government leaders on pandemic and other health and safety, workforce and performance preparedness, risks and change management, disaster preparedness and response and other operational and tactical concerns throughout her adult life. A former lead advisor to the Government of Bolivia on its pension privaitization project, Ms. Stamer also has worked internationally as an advisor to business, community and government leaders on crisis preparedness and response, workforce, health care and other reform, as well as regularly advises and defends organizations about the design, administration and defense of their organizations workforce, employee benefit and compensation, safety, discipline and other management practices and actions.
Board Certified in Labor and Employment Law By the Texas Board of Legal Specialization, Scribe for the ABA JCEB Annual Agency Meeting with OCR, Vice Chair of the ABA International Section Life Sciences Committee, and the ABA RPTE Employee Benefits & Other Compensation Group and and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her extensive publications and thought leadership as well as leadership involvement in a broad range of other professional and civic organizations. For more information about Ms. Stamer or her health industry and other experience and involvements, see http://www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation considering the specific facts and circumstances presented in their unique circumstance at the particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law constantly and often rapidly evolves, subsequent developments that could impact the currency and completeness of this discussion are likely. The author and Solutions Law Press, Inc. disclaim, and have no responsibility to provide any update or otherwise notify anyone of any fact or law specific nuance, change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
New Resources For Businesses, Employers, Schools & Homes To Stay Safe From COVID-19
March 11, 2020The Centers for Disease Control is sharing the following recommendations to help Americans stay safe during the current pandemic outbreak:
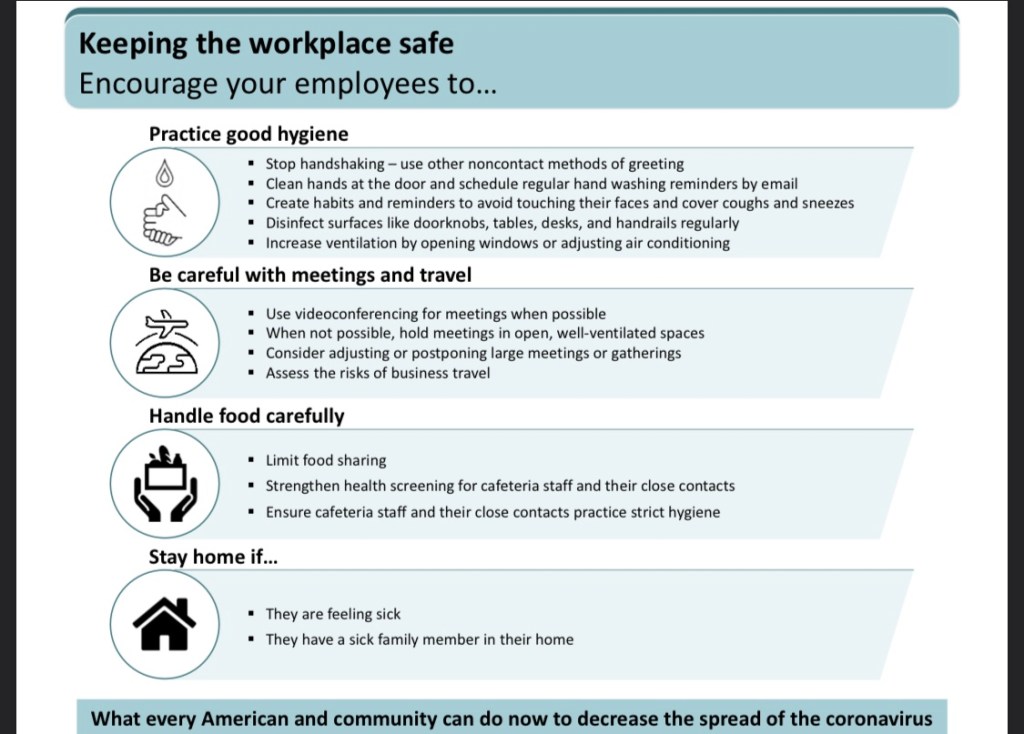



More Information
We hope this update is helpful. For more information about the these or other health or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- Proposed HHS Rule Making PBM Expenses Part of MLS Administrative Expense, Other Changes To ACA Helath Plan Rules Comment Deadline 5 P.M. Today
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- New PBGC Pension Rules Effective 3/5 May Require Action On Retirement Plans
- Revise Health Plan HIPAA Records Access Rules & Procedures To Use Newly Flexibility On Charging, Responding To Third Party PHI Requests
- 2/28 New Comment Deadline For NLRB Proposal To Exclude College Work Study Student Workers From NLRA Coverage
- Don’t Get Stuck Paying Another Employer’s Overtime Or Other Backpay
- 2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
- DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
- OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
- Salary Threshold Increases Require Employer Review Of Salaried Worker FLSA Exemption Qualification
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
Self Insured Plan & Contract Amendments Likely Required To Waive Deductibles, Expand Other Coronavirus Coverage
March 11, 2020Following up on the White House’s announcement yesterday that by major health insurers, Medicare and Medicaid to cover medically necessary testing and expand coverage for treatment of 2019 Novel Coronavirus (“coronavirus), without applying deductibles or coinsurance and offer expanded telemedicine and other coverage for coronavirus care, the Internal Revenue Service (“IRS”) today issued guidance giving health plans confirming health plans waiving deductibles won’t violate the Internal Revenue Code health savings account high deductible health plan rules. However many employer or other sponsors of self-insured health plans may need to amend their health plans and take other steps if they want their health plans to provide similar coverage. Meanwhile the Centers for Disease Control (“CDC”) released updated guidance to help businesses, schools, and other organizations to operate safely during the current outbreak.
Coronavirus Testing & Other Health Coverage
Major health insurers agreed in a Whitehouse Coronavirus Taskforce meeting yesterday to cover medically necessary testing and extend coverage to medically necessary treatment. The agreement only technically binds Medicare, Medicaid and other government programs and private insurers participating in the meeting. It does not automatically extend coverage or waive deductibles for self-insured employer or union sponsored health plans which provide coverage for an estimated 61 percent of covered U.S. worker and their families. Self-insured plan sponsors wishing to provide similar coverage and waive deductibles generally will need to take specific action to amend their plans and related contractracts and communications.
Vice President Pence announced the agreement with insurers yesterday saying among other things:
I’m pleased to report, as you requested, Mr. President, that all the insurance companies here — either today or before today — have agreed to waive all copays on coronavirus testing and extend coverage for coronavirus treatment in all of their benefit plans.
And, at your direction, Medicare and Medicaid, last week, already made it clear to Medicare and Medicaid beneficiaries that coronavirus testing and treatment would be covered. These private insurance carriers have extended that as well.
They’ve also agreed to cover telemedicine so that anyone, particularly among the vulnerable senior population, would not feel it necessary to go to a hospital or go to their doctor. They’ll know that telemedicine is covered.
While the announcement indicates that insurers involved in the meeting plan to expand coverage and waive deductibles, self-insured employer and union sponsored plans aren’t technically covered by the agreement. While many employers sponsoring self-insured health plans will want their health plan to provide similar coverage as part of their risk management response to the coronavirus outbreak. Self-insured plan sponsors and fiduciaries should confirm appropriate plan language is adopted and that their stop loss insurance carriers are on board or other arrangements are made to plan for and cover costs, and that other plan vendors are on board to handle responsibilities. This is particularly critical as failing to make the necessary amendments could result in an absence of stoploss insurance to cover additional cost. And relatively small workforce is with few people seeking the care, this might not make a material difference in plan costs. If several workers seek treatment, however, the absence of stoploss insurance coverage for the claims could both impact coverage for those particular items if the deductible under the policy has been met as well as could affect whether those claims count overall aggregate coverage losses. The bottom line is, make sure that your documentation matches your Promise or your extension of coverage will likely be truly 100% self insured. Likewise employers and other plan sponsors in the plan administrators of these plans are reminded that the law generally requires that they provide written notice of the changes to plan members in a timely fashion. Having plan administration services and other vendors on board also is important to ensure that the claims are appropriately and timely processed to avoid violation of plan terms and other rules.
In the meantime, the widespread lack of understanding among plan members about the distinction between insured and self-insured plans coupled with the breadth of the unqualified announcement by the White House is likely to fuel confusion by covered individuals and their providers. Not only will covered persons and providers need to know whether the program is insured or self-insured, they also will need to confirm how each of these programs implements the expanded coverage.
IRS Guidance Clears Way For High Deductible Health Plans To Raise Deductibles
Employers and health plans wishing to waive deductibles for coronavirus testing will not have to worry that waiving the deductible will violate IRS high deductible health plan (“HDHP”) rules, however. Earlier today, the IRS provided relief allowing high deductible health plans to pay these expenses without disqualifying their programs for high deductible health plan treatment under the Code in Notice 2020-15. The Notice provides that, until further guidance is issued, a health plan that otherwise satisfies the requirements to be a HDHP under Code section 223(c)(2)(A) will not fail to be an HDHP under section 223(c)(2)(A) merely because the health plan provides health benefits associated with testing for and treatment of COVID-19 without a deductible, or with a deductible below the minimum deductible (self only or family) for an HDHP. Also due to this guidance, an individual covered by the HDHP will not be disqualified from being an eligible individual under section 223(c)(1) who may make tax-favored contributions to a health savings account (HSA).
Business & Other Disruptions Response
Government, healthcare and other leaders are urging businesses and individuals to limit contact and care to guard against the virus because of its strength and ability to spread quickly. The U.S.’s top infectious-disease specialist told lawmakers the pathogen “is 10 times more deadly than the seasonal flu.”
Accordingly, health and government officials are urging all segments of society to take precautions. CDC, for instance has published the resources to help businesses, schools and others keep their people and locations safe here.
Unfortunately the strategy for ending the pandemic brings its own draconian side effects. Along with dealing with the threat of the disease itself, the efforts to manage the disease outbreak, many businesses also are forced to deal with demand losses, supply and business interruptions, staffing shortages, unanticipated expenses and a wide range of other operational and financial disruptions that are side effects of the outbreak and its management.
The outbreak has and continues to prompt the cancellation of a plethora of business, trade, government, school, and sports and entertainment events. Notable for its involvement in heath care and related insurance matters, the National Association of Insurance Commissioners (“NAIC”) is one of a growing number of event sponsors that are allowing workers to work from home, are cancelling or banning participation in live meetings and other events and/or are converting from live to virtual formats in response to the outbreak. Trade and business associations, entertainment and sports and otehr venures also are impacted. For instance, the NAIC announced its decision to move its meetings to a purely virtual format today. According to the announcement, the National Spring Meeting that had been scheduled to take place in Phoenix next week is cancelled. Instead, the NAIC announced the following tentative schedule:
- The public portion of the NAIC’s special session on state responses to COVID-19 will be held on March 20, 2020, starting at 11 AM ET via virtual meeting.
- Working groups, subgroups and other meetings will be held via conference calls March 16-31, 2020.
- Task force meetings will be held via conference calls April 1-10, 2020.
- Executive Committee and letter committees will be held via conference calls the week of April 13, 2020.
- EX/Plenary will meet via public conference call on April 20, 2020.
A revised schedule with dates, times and call-in numbers will be available on Naic.org next week.
Concerning the reasons for its decision, the NAIC explained:
Recently, the number of confirmed cases of COVID-19 has exceeded 100,000 worldwide, including over 1000 confirmed U.S. cases in 36 jurisdictions. Given rapidly changing information and out of an abundance of caution for the safety of our members, guests and staff, the NAIC officers, in consultation with NAIC members, have decided to hold the Spring National Meeting in a virtual-only format.
The NAIC is only one of a multitude of events cancelled or converted to a virtual format in the wake of fears of the coronavirus outbreak as US officials try to stem the spread of the virus. See e.g., Coronavirus updates in Texas: Community spread, school cancellations and more; Colleges and Universities Cancel Classes and Move Online Amid Coronavirus Fears; Coronavirus and sports: Seattle Mariners will move their home games, Golden State Warriors will play without fans and CBI is canceled.
Along with limiting contact, for instance, many businesses and organizations are “deep cleaning” their facilities to address potential virus contamination. Some biological experts point out however that this deep cleaning involves substantial expenditures which do little to guard against new exposures brought by others coming into a business, school or other workplace. Some biological contamination experts suggest that organizations should consider investing in resources specified ultraviolet lights or other tools that could help control exposures on a longer-term and more recurrent basis. Experts emphasize that remediation and prevention efforts need to recognize that exposures are likely to occur recurrently over a period of time across the life of this and future virus outbreaks.
The financial consequences of staffing or supply shortages, declines in product or services demands, event cancellations, cleaning and other costs and a host of other side effects present such a widespread risk to many businesses that many are facing layoffs or even bankruptcy or other restrucuring. While President Trump and other federal and state leaders are promising employment tax holidays and other relief to try to mitigate some of these financial effects, businesses impacted by these disruptions should begin assessing and planning to execute options to mitigate losses and manage these risks as soon as possible to maximize their potential ability to take advantage of options to restructure debt or contractual obligations, adjust workforce staffing, and make other adjustments successfully to weather the pandemic storm and fallout. When considering these options, businesses will want to understand the relative complete costs of reductions in hours, furloughs, contractual adjustments and other options to make and execute their choices as well as possible.
More Information
We hope this update is helpful. For more information about the these or other health or other legal, management or public policy developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of health industry and other management work, public policy leadership and advocacy, coaching, teachings, and publications. As a significant part of her work, Ms. Stamer has worked extensively domestically and internationally with business, government and community leaders to prepare for and deal with pandemic and other health and safety, financial, workforce and other organizational crisis, change and workforce, employee benefit, health care and other operations planning, preparedness and response for more than 30 years. As a part of this work, she regularly advises businesses and government leaders on an an demand and ongoing basis about preparation of workforce, health care and other business and government policies and practices to deal with management in a wide range of contexts ranging from day to day operations, through times of change and in response to operational, health care, natural disaster, economic and other crisis and change.
Author of “Privacy and the Pandemic Workshop” for the Association of State and Territorial Health Plans, “How to Conduct A Reduction In Force,” and a multitude of other highly regarded publications and presentations on workforce, compliance, health care and health benefits, pandemic and other health crisis, workers’ compensation and occupational disease, business disaster and distress and many other topics, Ms. Stamer has worked with employers, insurers, health industry organizations and providers and domestic and international community and government leaders on pandemic and other health and safety, workforce and performance preparedness, risks and change management, disaster preparedness and response and other operational and tactical concerns throughout her adult life. A former lead advisor to the Government of Bolivia on its pension privaitization project, Ms. Stamer also has worked internationally as an advisor to business, community and government leaders on crisis preparedness and response, workforce, health care and other reform, as well as regularly advises and defends organizations about the design, administration and defense of their organizations workforce, employee benefit and compensation, safety, discipline and other management practices and actions.
Board Certified in Labor and Employment Law By the Texas Board of Legal Specialization, Scribe for the ABA JCEB Annual Agency Meeting with OCR, Vice Chair of the ABA International Section Life Sciences Committee, and the ABA RPTE Employee Benefits & Other Compensation Group and and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her extensive publications and thought leadership as well as leadership involvement in a broad range of other professional and civic organizations. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- Proposed HHS Rule Making PBM Expenses Part of MLS Administrative Expense, Other Changes To ACA Helath Plan Rules Comment Deadline 5 P.M. Today
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
- New PBGC Pension Rules Effective 3/5 May Require Action On Retirement Plans
- Revise Health Plan HIPAA Records Access Rules & Procedures To Use Newly Flexibility On Charging, Responding To Third Party PHI Requests
- 2/28 New Comment Deadline For NLRB Proposal To Exclude College Work Study Student Workers From NLRA Coverage
- Don’t Get Stuck Paying Another Employer’s Overtime Or Other Backpay
- 2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
- DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
- OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
- Salary Threshold Increases Require Employer Review Of Salaried Worker FLSA Exemption Qualification
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
Health Plans, Providers & PBM Face Pressure To Prepare For Health Transparency As Trump Transparency Reforms March Foward
March 2, 2020Today (March 2, 2020) is the deadline for employers and other health benefit program sponsors, insurers, plan administrators and fiduciaries, health care providers, PBMs and other interested persons to comment on proposed federal rule change that would require insured health plans to count drug rebates and price concessions retained by pharmacy benefit managers (PBMs) as administrative expenses for purposes of determining if the issuing insurer is required to rebate premiums under the medical loss ratio (MLR) rules of the Patient Protection & Affordable Care Act (“ACA”). With the comment period on the package of health care transparency regulations published by the Trump Administration to implement the transparency reform it hopes will fuel better quality and cost effectiveness in the U.S. health care system, health plan sponsors, fiduciaries, administrators, insurers, heath care providers, PBMs, and other participants in the system need to start preparing to deal with their own responsibilities under the new rules, and to help plan members, patients and their caregivers, and other consumers to understand and use the new information the rules will make available.
2/06/20 Proposed Rule Pressures Insurers To Require PBMs To Disclose & Pass Through Manufacturer Rebates
Issued as part of the proposed “Patient Protection and Affordable Care Act; HHS Notice of Benefit and Payment Parameters for 2021; Notice Requirement for Non-Federal Governmental Plans Proposed Rule” (“2/6/20 Proposed Rule”) published by the Department of Health & Human Services (“HHS”) on February 6. 2020, the as part of a series of Trump Administration health care reform initiatives seeking to use competition and transparency to improve health care quality, choice and affordability, in furtherance of the Trump Administration “health plan transparency” initiative HHS predicts this change included in the could generate $18.2 million more per year in the MLR rebate payments to consumers covered under insure health plans subject to the MLR and other insurance market reform provisions of the ACA. See also Remarks by President Trump on Honesty and Transparency in Healthcare Prices (November 15, 2019). For a more detailed summary of the 2/06/20 Proposed Rule, see here.Most health plans contract with PBMs to decide the prescription drug formularies, copays, and other coverage design for their health plans, to administer their pharmacy benefits and to negotiate discounts and rebates from drug manufacturers in exchange for placing their drugs on a health plan’s formulary. PBMs are supposed to work on behalf of health plans to secure drug rebates, refunds, discounts, coupons, and direct or indirect remuneration, among other discounts. Health plans compensate PBMs in a variety of ways, including:
- Paying administrative fees;
- Allowing a PBM to retain the difference between the amount a PBM charges the health plan for a drug and the amount a PBM pays the pharmacy (called “spread pricing”); or
- Allowing a PBM to retain all or a portion of any negotiated discounts from manufacturers, including rebates.
Currently, insured plans covered by the MLR rule as well as the PBM arrangements of many self-insured, employer or union sponsored health plans, do not require PBMs to disclose, account for, or pass through to the health plan they are engaged by the prescription drug rebates and certain other amounts that PBMs receive and retain from prescription drug manufacturers that the PBM selects for inclusion on the health plan formulary.
The current federal ACA MLR rule requires insured health plans subject to the MLR rule to deduct from their prescription drug claims both rebates they receive from manufacturers and any payments the PBM retains from the spread, but does not address situations in which the PBM retains rebates or other price concessions negotiated on behalf of the plans. Consequently, the MLR reporting or calculation of insurers typically does not reflect any rebates PBMs retain that are not passed through to the insurer even though the PBM is supposed to be working on behalf of the health plan.
In recent years, these arrangements have come under widespread criticism as creating conflicts of interests that compromise the loyalty of the PBM to act in the best interest of its health plan clients and their plan members because when PBMs don’t report and pass through all pricing concessions negotiated by PBMs, health plans and health plan members don’t receive the benefit of those price discounts and the decisions that the PBM makes in choosing the highest quality and most cost effective medications for the formulary may lead the PBM to choose and price drugs on the plan formulary to maximize the PBM’s profits rather than the best interests of the plan and its members.
The 2/06/20 Proposed Rule would classify the portion of premium revenue that an insured health plan subject to the MLR rule expends on pharmacy costs as the actual reimbursement to pharmacies – minus any rebates or price concessions from manufacturers – no matter if the plan or its contracted PBM receives the price concession. Requiring health insurers covered by the MLR rule to include rebates retained by their PBMs an administrative expense would make it difficult for most health insurers to keep all administrative expenses within 15 or 20 percent the MLR rules. Since health insurers whose administrative expenses exceed the MLS ratio must rebate premiums under the ACA, HHS anticipates that finalizing the 2/06/20 Proposed Rule as proposed would prompt insured health plans covered by the MLR rule that use PBMs to administer pharmacy benefits to change the compensation provisions of their PBM contracts to eliminate or restructure those payments.
Since self-insured health plans generally are not subject to the ACA MLR rule, however, those plans generally need to pursue contracting or other strategies to address this concern. Increasingly, many self-insured health plan sponsors, fiduciaries and administrators already are changing their PBM contracting and selection strategies to require disclosure and pass through of rebate and other compensation received by PBMs from manufacturers such as including administrative-fee-only compensation and a guarantee of 100 percent pass-through of rebates and manufacturer-derived revenue from the PBM to the health plan in their PBM contracts.
With the official comment deadline set to expire on March 2, 2020, employer and other insured and self-insured health plan sponsors of health plans using PBMs, fiduciaries and advisors should turn their attention to evaluating the likely implications of the 02/06/20 Proposed Rule on their health plan arrangements as well as more generally evaluating their pharmacy benefit designs, PBM contracts and compensation arrangements, and associated arrangements and practices for potential conflicts of interest, hidden cost savings and other opportunities for improvement. As part of this efforts, employer sponsors, plan fiduciaries, administrators, and vendors of self-insured plans should keep in mind that the fiduciary responsibility rules of the Employee Retirement Income Security Act generally require plan fiduciaries to prudently evaluate compensation and other arrangements with plan vendors as well as to take action to identify and protect the plan against breaches of loyalty by plan vendors or fiduciaries from conflicts of interests or prohibited transactions. Plan administrators also should conduct due diligence to confirm that PBM and other vendors properly including all compensation for purposes of Form 5500 and other reporting. Along with assisting their health plan clients with these activities, brokers, consultants, TPAs, and other plan vendors also should evaluate the potential implications of the reforms in the 02/06/20 Proposed Rule as well as any relevant state law reforms on the advice and services they provide to their clients, as well as their potential responsibilities and exposures in light of the evolving state health and PBM transparency rules.
Other Health Plan Transparency Reforms
The 2/06/20 Proposed Rule is one in a series of federal health rule changes the Trump Administration is pursuing as part of its initiative seeking to use health care transparency to improve the price, quality and choice in the U.S. health care system. In addition to the changes proposed in the 2/06/20 Proposed Rule, in response to President Trump’s July 24, 2020 Executive Order on Improving Price and Quality Transparency in American Healthcare to Put Patients First, HHS on November 14, 2019 also undertook two other regulatory actions intended to increase price transparency to empower patients and increase competition among all hospitals, group health plans and health insurance issuers in the individual and group markets:
- Issued a proposed Transparency in Coverage Proposed Rule (the “Proposed Coverage Transparency Rule”); and
- The Calendar Year (CY) 2020 Outpatient Prospective Payment System (OPPS) & Ambulatory Surgical Center (ASC) Price Transparency Requirements for Hospitals to Make Standard Charges Public Final Rule (“Hospital Transparency Rule”).
Both the final and proposed rules require that pricing information be made publicly available.
- Proposed Coverage Transparency Rule
The Proposed Coverage Transparency Rule would require most employer-based group health plans and health insurance issuers offering group and individual coverage to disclose price and cost-sharing information to participants, beneficiaries, and enrollees up front. With this information, patients will have accurate estimates of any out-of-pocket costs they must pay to meet their plan’s deductible, co-pay, or co-insurance requirements. This will make previously unavailable price information accessible to patients and other stakeholders in a standardized way, allowing for easy comparisons.
If finalized, the Proposed Transparency in Coverage Rule will require non-grandfathered health plans and health insurance issuers to make certain health care price information more accessible to consumers and other stakeholders by requiring each non-grandfathered group health plan[2] or health insurance issuer offering non-grandfathered health insurance coverage in the individual and group markets to make available:
- To participants, beneficiaries and enrollees (or their authorized representative) personalized out-of-pocket cost information for all covered health care items and services through an internet-based self-service tool and in paper form upon request. For the first time, most consumers would be able to get estimates of their cost-sharing liability for health care for different providers, allowing them to both understand how costs for covered health care items and services are determined by their plan, and shop and compare costs for health care before receiving care; and
- To the public, including stakeholders such as consumers, researchers, employers, and third-party developers the in-network negotiated rates with their network providers and historical payments of allowed amounts to out-of-network providers through standardized, regularly updated machine-readable files.
The Trump Administration believes these changes will provide opportunities for innovation to drive price comparison and consumerism in the health care market. In addition, the Transparency In Coverage Rule also proposes to allow issuers that empower and incentivize consumers through the introduction of plans that include provisions that encourage consumers to shop for services from lower-cost, higher-value providers, and that share the resulting savings with consumers, to take credit for such “shared savings” payments in their medical loss ratio (MLR) calculations. HHS says it made this proposal to ensure, should the proposal be finalized as proposed, that issuers would not be required to pay MLR rebates based on a plan design that would provide a benefit to consumers that is not currently captured in any existing MLR revenue or expense category. HHS believes this proposal would preserve the statutorily-required value that consumers receive for coverage under the MLR program, while encouraging issuers to offer new or different value-based plan designs that support competition and consumer engagement in health care. See also Transparency in Coverage Proposed Rule (CMS-9915-P) Fact Sheet. The official comment period on the Proposed Transparency in Coverage Rule has not expired. In January, HHS extended the comment period on the Transparency in Coverage Rule from January 14, 2020 to January 29, 2020.
- Final Hospital Transparency Rule
Concurrent with its release of the Proposed Coverage Transparency Rule, HHS also finalized the Hospital Transparency Rule that will require hospitals to provide patients with clear, accessible information about their “standard charges” for the items and services they provide in two ways beginning in 2021:
- Comprehensive Machine-Readable File: Hospitals will be required to make public all hospital standard charges (including the gross charges, payer-specific negotiated charges, the amount the hospital is willing to accept in cash from a patient, and the minimum and maximum negotiated charges) for all items and services on the Internet in a single data file that can be read by other computer systems. The file must include additional information such as common billing or accounting codes used by the hospital (such as Healthcare Common Procedure Coding System (HCPCS) codes) and a description of the item or service to provide common elements for consumers to compare standard charges from hospital to hospital.
- Display of Shoppable Services in a Consumer-Friendly Manner: Hospitals will be required to make public payer-specific negotiated charges, the amount the hospital is willing to accept in cash from a patient for an item or service, and the minimum and maximum negotiated charges for 300 common shoppable services in a manner that is consumer-friendly and update the information at least annually.
- Shoppable services are services that can be scheduled by a healthcare consumer in advance such as x-rays, outpatient visits, imaging and laboratory tests or bundled services like a cesarean delivery, including pre- and post-delivery care.
- The requirements for the consumer-friendly file are that the information must be made public in a prominent location online that is easily accessible, without barriers, and it must also be searchable. Item and service descriptions must be in ‘plain language’ and the shoppable service charges must be displayed and grouped with charges for any ancillary services the hospital customarily provides with the primary shoppable service.
In order to ensure that hospitals comply with the requirements, the Hospital Transparency Rule also provides CMS with new enforcement tools including monitoring, auditing, corrective action plans, and the ability to impose civil monetary penalties of $300 per day. In response to public comments, CMS is finalizing that the effective date of the final rule will be January 1, 2021 to ensure that hospitals have the time to be compliant with these policies. See also
Start Preparing For New Transparency Requirements, Effects & Opportunities
With the comment periods on the Proposed Transparency in Coverage Rule already past and the deadline for comment on the 2/6/20 Proposed Rule set to expire today, employer and other health benefit plan sponsors, insurers, fiduciaries, administrators, heath care providers, insurers, plan members and other stakeholders should turn their attention to evaluating the potential opportunities, burdens, and impacts of these transparency reforms.
More Information
We hope this update is helpful. For more information about the or other health or other employee benefits, human resources, or health care developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
The author of this update, Cynthia Marcotte Stamer, will speak about these and other health care cost and transparency reforms as a panelist on the program on Impact of Governmental Policy on Pricing and Access to Prescription Medical Products in the US and International Marketplace scheduled to take place at the American Bar Association International Section Annual Meeting in New York City on April 23, 2020.
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of health industry and other management work, public policy leadership and advocacy, coaching, teachings, and publications including more than 30 years’ leading edge work on PBM and other insured and self-insured contracting and related matters. .
Author of numerous highly regarded works on PBM and other health plan contracting and design, Vice Chair of the ABA International Section Life Sciences Committee, past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group and the ABA RPTE Employee Benefits & Other Compensation Group, Ms. Stamer’s work throughout her 30 plus year career has focused heavily on working with health care and managed care, health and other employee benefit plan, insurance and financial services and other public and private organizations and their technology, data, and other service providers and advisors domestically and internationally with legal and operational compliance and risk management, performance and workforce management, regulatory and public policy and other legal and operational concerns. As a part of this work, she has continuously and extensively worked with domestic and international health plans, their sponsors, fiduciaries, administrators, and insurers; managed care and insurance organizations; hospitals, health care systems and other health care providers, accreditation, peer review and quality committees and organizations; billing, utilization management, management services organizations, group purchasing organizations; pharmaceutical, pharmacy, and prescription benefit management and organizations; consultants; investors; EMR, claims, payroll and other technology, billing and reimbursement and other services and product vendors; products and solutions consultants and developers; investors; managed care organizations, self-insured health and other employee benefit plans, their sponsors, fiduciaries, administrators and service providers, insurers and other payers, health industry advocacy and other service providers and groups and other health and managed care industry clients as well as federal and state legislative, regulatory, investigatory and enforcement bodies and agencies.
Ms. Stamer is most widely recognized for her decades of pragmatic, leading edge work, scholarship and thought leadership on health and other privacy and data security and other health industry legal, public policy and operational concerns. This involvement encompasses helping health care systems and organizations, group and individual health care providers, health plans and insurers, health IT, life sciences and other health industry clients prevent, investigate, manage and resolve sexual assault, abuse, harassment and other organizational, provider and employee misconduct and other performance and behavior; manage Section 1557, Civil Rights Act and other discrimination and accommodation, and other regulatory, contractual and other compliance; vendors and suppliers; contracting and other terms of participation, medical billing, reimbursement, claims administration and coordination, Medicare, Medicaid, CHIP, Medicare/Medicaid Advantage, ERISA and other payers and other provider-payer relations, contracting, compliance and enforcement; Form 990 and other nonprofit and tax-exemption; fundraising, investors, joint venture, and other business partners; quality and other performance measurement, management, discipline and reporting; physician and other workforce recruiting, performance management, peer review and other investigations and discipline, wage and hour, payroll, gain-sharing and other pay-for performance and other compensation, training, outsourcing and other human resources and workforce matters; board, medical staff and other governance; strategic planning, process and quality improvement; meaningful use, EMR, HIPAA and other technology, data security and breach and other health IT and data; STARK, ant kickback, insurance, and other fraud prevention, investigation, defense and enforcement; audits, investigations, and enforcement actions; trade secrets and other intellectual property; crisis preparedness and response; internal, government and third-party licensure, credentialing, accreditation, HCQIA and other peer review and quality reporting, audits, investigations, enforcement and defense; patient relations and care; internal controls and regulatory compliance; payer-provider, provider-provider, vendor, patient, governmental and community relations; facilities, practice, products and other sales, mergers, acquisitions and other business and commercial transactions; government procurement and contracting; grants; tax-exemption and not-for-profit; privacy and data security; training; risk and change management; regulatory affairs and public policy; process, product and service improvement, development and innovation, and other legal and operational compliance and risk management, government and regulatory affairs and operations concerns. to establish, administer and defend workforce and staffing, quality, and other compliance, risk management and operational practices, policies and actions; comply with requirements; investigate and respond to Board of Medicine, Health, Nursing, Pharmacy, Chiropractic, and other licensing agencies, Department of Aging & Disability, FDA, Drug Enforcement Agency, OCR Privacy and Civil Rights, Department of Labor, IRS, HHS, DOD, FTC, SEC, CDC and other public health, Department of Justice and state attorneys’ general and other federal and state agencies; JCHO and other accreditation and quality organizations; private litigation and other federal and state health care industry actions: regulatory and public policy advocacy; training and discipline; enforcement; and other strategic and operational concerns.
Author of publications on “Transparent PBM Contracting,” “ACOs, Direct Contracting: Legal & Practical Challenges For Employers, Providers & TPAs,” “The Medicare Advantage Contracting Manual,” “Third Party Administrator (TPA) Contracting Principles and Strategies and a multitude of other highly regarded publications and presentations, Stamer is widely recognized for her thought leadership on PBM and other managed care and health plan contracting and design, and a multitude of other health care, health plan and other health industry matters. In addition, Ms. Stamer contributes her time and leadership to numerous policy, professional, civil and other organizations including service as the, the American Bar Association (ABA) International Section Life Sciences Committee Vice Chair, a Scribe for the ABA Joint Committee on Employee Benefits (JCEB) Annual OCR Agency Meeting and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her extensive publications and thought leadership as well as leadership involvement in a broad range of other professional and civic organizations. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- 2/28 New Comment Deadline For NLRB Proposal To Exclude College Work Study Student Workers From NLRA Coverage
- Don’t Get Stuck Paying Another Employer’s Overtime Or Other Backpay
- 2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
- DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
- OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation considering the specific facts and circumstances presented in their unique circumstance at the particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law constantly and often rapidly evolves, subsequent developments that could impact the currency and completeness of this discussion are likely. The author and Solutions Law Press, Inc. disclaim, and have no responsibility to provide any update or otherwise notify anyone of any fact or law specific nuance, change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
Proposed HHS Rule Making PBM Expenses Part of MLS Administrative Expense, Other Changes To ACA Helath Plan Rules Comment Deadline 5 P.M. Today
March 2, 2020Today (March 2, 2020) is the last day to submit comments on Department of Health and Human Services (“HHS”) “Patient Protection and Affordable Care Act; HHS Notice of Benefit and Payment Parameters for 2021; Notice Requirement for Non-Federal Governmental Plans Proposed Rule” (“Proposed Rule”) published by HHS on February 6. 2020.
Among other things, the Proposed Rule, if adopted as proposed, would:
- Repeal regulations relating to the Early Retiree Reinsurance Program;
- Require health plans in state insurance markets to count drug rebates and price concessions retained by pharmacy benefit managers (PBMs) as administrative expenses. HHS predicts this change could generate $18.2 million more per year in medical loss ratio (MLR) rebate payments to consumers;.
- Establish payment parameters and provisions related to the risk adjustment and risk adjustment data validation programs; cost-sharing parameters and cost-sharing reductions; and user fees for federally-facilitated Exchanges and State-based Exchanges on the Federal platform;
- Modify requirements for “essential health benefits” to allow states greater flexibility and add an annual state reporting of state-required benefits that are in addition to essential health benefits (EHB) for which states are required to defray the costs;
- Amend rules to give states with additional flexibility in the operation and establishment of Exchanges concerning cost-sharing for prescription drugs; excepted benefit health reimbursement arrangements offered by non-Federal governmental plan sponsors; the medical loss ratio program; Exchange eligibility and enrollment; exemptions from the requirement to maintain coverage; quality rating information display standards for Exchanges; and other related topics.
For a more detailed summary of the Proposed Rule, see here.
Employer and other health benefit plan sponsors, insurers, fiduciaries, administrators, heath care providers and other stakeholders desiring to comment on the Proposed Rule must submit their comments electronically no later than 5 p.m. Eastern today (March 2, 2020) by following the submit comments instructions here.
More Information
We hope this update is helpful. For more information about the this or other health or other employee benefits, human resources, or health care developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of health industry and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Scribe for the ABA JCEB Annual Agency Meeting with OCR, Vice Chair of the ABA International Section Life Sciences Committee, past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group and the ABA RPTE Employee Benefits & Other Compensation Group, Ms. Stamer’s work throughout her 30 plus year career has focused heavily on working with health care and managed care, health and other employee benefit plan, insurance and financial services and other public and private organizations and their technology, data, and other service providers and advisors domestically and internationally with legal and operational compliance and risk management, performance and workforce management, regulatory and public policy and other legal and operational concerns. As a part of this work, she has continuously and extensively worked with domestic and international health plans, their sponsors, fiduciaries, administrators, and insurers; managed care and insurance organizations; hospitals, health care systems, clinics, skilled nursing, long term care, rehabilitation and other health care providers and facilities; medical staff, accreditation, peer review and quality committees and organizations; billing, utilization management, management services organizations, group purchasing organizations; pharmaceutical, pharmacy, and prescription benefit management and organizations; consultants; investors; EMR, claims, payroll and other technology, billing and reimbursement and other services and product vendors; products and solutions consultants and developers; investors; managed care organizations, self-insured health and other employee benefit plans, their sponsors, fiduciaries, administrators and service providers, insurers and other payers, health industry advocacy and other service providers and groups and other health and managed care industry clients as well as federal and state legislative, regulatory, investigatory and enforcement bodies and agencies.
Ms. Stamer is most widely recognized for her decades of pragmatic, leading edge work, scholarship and thought leadership on health and other privacy and data security and other health industry legal, public policy and operational concerns. This involvement encompasses helping health care systems and organizations, group and individual health care providers, health plans and insurers, health IT, life sciences and other health industry clients prevent, investigate, manage and resolve sexual assault, abuse, harassment and other organizational, provider and employee misconduct and other performance and behavior; manage Section 1557, Civil Rights Act and other discrimination and accommodation, and other regulatory, contractual and other compliance; vendors and suppliers; contracting and other terms of participation, medical billing, reimbursement, claims administration and coordination, Medicare, Medicaid, CHIP, Medicare/Medicaid Advantage, ERISA and other payers and other provider-payer relations, contracting, compliance and enforcement; Form 990 and other nonprofit and tax-exemption; fundraising, investors, joint venture, and other business partners; quality and other performance measurement, management, discipline and reporting; physician and other workforce recruiting, performance management, peer review and other investigations and discipline, wage and hour, payroll, gain-sharing and other pay-for performance and other compensation, training, outsourcing and other human resources and workforce matters; board, medical staff and other governance; strategic planning, process and quality improvement; meaningful use, EMR, HIPAA and other technology, data security and breach and other health IT and data; STARK, ant kickback, insurance, and other fraud prevention, investigation, defense and enforcement; audits, investigations, and enforcement actions; trade secrets and other intellectual property; crisis preparedness and response; internal, government and third-party licensure, credentialing, accreditation, HCQIA and other peer review and quality reporting, audits, investigations, enforcement and defense; patient relations and care; internal controls and regulatory compliance; payer-provider, provider-provider, vendor, patient, governmental and community relations; facilities, practice, products and other sales, mergers, acquisitions and other business and commercial transactions; government procurement and contracting; grants; tax-exemption and not-for-profit; privacy and data security; training; risk and change management; regulatory affairs and public policy; process, product and service improvement, development and innovation, and other legal and operational compliance and risk management, government and regulatory affairs and operations concerns. to establish, administer and defend workforce and staffing, quality, and other compliance, risk management and operational practices, policies and actions; comply with requirements; investigate and respond to Board of Medicine, Health, Nursing, Pharmacy, Chiropractic, and other licensing agencies, Department of Aging & Disability, FDA, Drug Enforcement Agency, OCR Privacy and Civil Rights, Department of Labor, IRS, HHS, DOD, FTC, SEC, CDC and other public health, Department of Justice and state attorneys’ general and other federal and state agencies; JCHO and other accreditation and quality organizations; private litigation and other federal and state health care industry actions: regulatory and public policy advocacy; training and discipline; enforcement; and other strategic and operational concerns.
Author of leading works on HIPAA and a multitude of other health care, health plan and other health industry matters, the American Bar Association (ABA) International Section Life Sciences Committee Vice Chair, a Scribe for the ABA Joint Committee on Employee Benefits (JCEB) Annual OCR Agency Meeting and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her extensive publications and thought leadership as well as leadership involvement in a broad range of other professional and civic organizations. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- 2/28 New Comment Deadline For NLRB Proposal To Exclude College Work Study Student Workers From NLRA Coverage
- Don’t Get Stuck Paying Another Employer’s Overtime Or Other Backpay
- 2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
- DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
- OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation considering the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law constantly and often rapidly evolves, subsequent developments that could impact the currency and completeness of this discussion are likely. The author and Solutions Law Press, Inc. disclaim, and have no responsibility to provide any update or otherwise notify anyone of any fact or law specific nuance, change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
February 25, 2020Employers and their payroll service provider should prepare for income and employment tax withholding changes expected when the Department of Treasury and Internal Revenue Service (IRS) finalize recently proposed rules on Income Tax Withholding From Wages intended to update the federal income tax withholding rules to reflect changes made by the Tax Cuts and Jobs Act (TCJA) and other legislation.
Staying on top of employment tax compliance is important because business owners and operators and the business’ tax, accounting and other service providers increasingly risk criminal prosecution as well as stiff civil tax penalties upon their businesses for failing properly to report wages and withhold and pay federal income tax and employees’ share of social security and Medicare taxes (collectively known as “FICA taxes”). Learn more here.
The proposed rules officially published in the Federal Register on February 13, 2020 available here follow up the agencies’ previous release of the resigned 2020 W-4, Employee’s Withholding Certificate by providing guidance to employers about the amount of federal income tax to withhold from employee’s wages following the TCJA.
The proposed regulations address numerous income tax withholding and reporting changes made by TCJA to sections 3401 and 3402, but do not address withholding withholding on pensions, annuities, and certain other deferred income under section 3405(a) as the agencies separately addrress those rules in Notice 2020-3.
The agencies describe the proposed rules as providing “flexible and administrable rules for income tax withholding from wages intended to work with both the 2020 Form W-4 and its related tables and computational procedures described in Publication 15-T, and Forms W-4 and related tables and computational procedures provided in 2019 and earlier years.
As the proposed regulations are expected to impact the wage based tax information collection, withholding and reporting practices of most employers, every business paying wages subject to withholding will want to act quickly to review the proposed regulations to identify and begin preparations to implement the necessary changes in their systems and practices to comply with the proposed rules when finalized. Small or other employers or other stakeholders that wish to provide feedback on the proposed rules also will want to submit any comments before the comment period closes on April 13, 2020.
More Information
We hope this update is helpful. For more information about the Coix Order or other health or other employee benefits, human resources, or health care developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation; Former Chair of the RPTE Employee Benefits and Compensation Committee, the current Co-Chair of its Welfare Benefit Committee and former Chair of its Welfare Benefit, Plan Terminations, Fiduciary Responsibility and Defined Compensation Plan Committees; former RPTE Joint Committee on Employee Benefits Council (JCEB) Representative, Cynthia Marcotte Stamer is a Martindale-Hubble “AV-Preeminent” practicing attorney and management consultant, author, public policy advocate, author and lecturer repeatedly recognized for her 30 plus years’ of work and pragmatic thought leadership, publications and training on health, pension and other employee benefit, insurance, labor and employment, and health care fiduciary responsibility, payment, investment, contracting and other design, administration and compliance concerns as among the “Top Rated Labor & Employment Lawyers in Texas,” a “Legal Leader,” a “Top Woman Lawyer” and with other awards by LexisNexis® Martindale-Hubbell®; as among the “Best Lawyers In Dallas” for her work in the field of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, in International Who’s Who of Professionals and with numerous other awards and distinctions.
Highly valued for combining extensive legal and industry knowledge and experience with pragmatic creativity to help clients find and implement workable client-centric solutions, Ms. Stamer advises, represents and defends employers and other management clients and organizations; employer, union, multi-employer, association and other employee benefit plan plans, their sponsors, insurers and fiduciaries, plan administrators, administrative services, technology and other service providers, foreign and domestic governments, and others about employment and other services; health and welfare, pension, profit sharing other employee benefit and insurance program and policy management, administration, design and innovation, compliance, funding, documentation, communication, data security and use, contracting, plan, public and regulatory reforms and enforcement, and other risk management, compliance and operations matters. Her experience encompasses leading and supporting the development and defense of innovative new policies, programs, practices and solutions; advising and representing clients on routine plan establishment, plan documentation and contract drafting and review, administration, change and other compliance and operations; crisis prevention and response, compliance and risk management audits and investigations, enforcement actions and other dealings with the US Congress, Departments of Labor, Treasury, Health & Human Services, Federal Trade Commission, Justice, Securities and Exchange Commission, Education and other federal agencies, state legislatures, attorneys general, insurance, labor, worker’s compensation, and other agencies and regulators, and various other foreign and domestic governmental bodies and agencies. She also provides strategic and other supports clients in defending litigation as lead strategy counsel, special counsel and as an expert witness.
Alongside her extensive legal and operational experience, Ms. Stamer also is recognized for her work as a public and regulatory policy advocate and community leader with a gift for finding pragmatic solutions and helping to forge the common ground necessary to build consensus. Best known for her domestic public policy and community leadership on health care and insurance reform, Ms. Stamer’s lifelong public policy and community service involvement includes service as a lead consultant to the Government of Bolivia on its pension privatization project, as well as extensive legislative and regulatory reform, advocacy and input workforce, worker classification, employee benefit, public health and healthcare, social security and other disability and aging in place, education, migration reforms domestically and internationally throughout her adult life. In addition to her public and regulatory policy involvement, Ms. Stamer also contributes her service and leadership to a professional and civic organizations and efforts. Beyond her RPTE leadership involvements, these include her involvement as the Founder and Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE; Coalition on Patient Empowerment, a founding Board Member and past President of the Alliance for Healthcare Excellence; former Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; Vice Chair, Policy for the Life Sciences Committee of the ABA International Section, Chair of the ABA Intellectual Property Section Law Practice Management Committee, Past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group; former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, former Board Member, Continuing Education Chair and Treasurer of the Southwest Benefits Association; Vice President and Executive Director of the North Texas Healthcare Compliance Professionals Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; past Dallas World Affairs Council Board Member, and leadership of many other professional, civic and community organizations. Ms. Stamer also is a highly popular lecturer, symposia chair and author, who publishes and speaks extensively on health and managed care industry, human resources, employment and other privacy, data security and other technology, regulatory and operational risk management for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, the Society of Professional Benefits Administrators, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients, serves on the faculty and planning committee of many workshops, seminars, and symposia, and on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Beyond these involvements, Ms. Stamer also is active in the leadership of a broad range of other public policy advocacy and other professional and civic organizations and involvements. Through these and other involvements, she helps develop and build solutions, build consensus, garner funding and other resources, manage compliance and other operations, and take other actions to identify promote tangible improvements in health care and other policy and operational areas.
Before founding her current law firm, Cynthia Marcotte Stamer, P.C., Ms. Stamer practiced law as a partner with several prominent national and international law firms for more than 10 years before founding Cynthia Marcotte Stamer, P.C. to practice her unique brand of “Solutions law™” and to devote more time to the pragmatic policy and system reform, community education and innovation, and other health system improvement efforts of her PROJECT COPE: the Coalition on Patient Empowerment initiative.
Scribe for the ABA JCEB Annual Agency Meeting with OCR, Vice Chair of the ABA International Section Life Sciences Committee, past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group and the ABA RPTE Employee Benefits & Other Compensation Group, Ms. Stamer is most widely recognized for her decades of pragmatic, leading edge work, scholarship and thought leadership on health and other privacy and data security and other health industry legal, public policy and operational concerns. Ms. Stamer’s work throughout her 30 plus year career has focused heavily on working with health care and managed care, health and other employee benefit plan, insurance and financial services and other public and private organizations and their technology, data, and other service providers and advisors domestically and internationally with legal and operational compliance and risk management, performance and workforce management, regulatory and public policy and other legal and operational concerns. As a part of this work, she has continuously and extensively worked with domestic and international health plans, their sponsors, fiduciaries, administrators, and insurers; managed care and insurance organizations; hospitals, health care systems, clinics, skilled nursing, long term care, rehabilitation and other health care providers and facilities; medical staff, accreditation, peer review and quality committees and organizations; billing, utilization management, management services organizations, group purchasing organizations; pharmaceutical, pharmacy, and prescription benefit management and organizations; consultants; investors; EMR, claims, payroll and other technology, billing and reimbursement and other services and product vendors; products and solutions consultants and developers; investors; managed care organizations, self-insured health and other employee benefit plans, their sponsors, fiduciaries, administrators and service providers, insurers and other payers, health industry advocacy and other service providers and groups and other health and managed care industry clients as well as federal and state legislative, regulatory, investigatory and enforcement bodies and agencies.
This involvement encompasses helping health care systems and organizations, group and individual health care providers, health plans and insurers, health IT, life sciences and other health industry clients prevent, investigate, manage and resolve sexual assault, abuse, harassment and other organizational, provider and employee misconduct and other performance and behavior; manage Section 1557, Civil Rights Act and other discrimination and accommodation, and other regulatory, contractual and other compliance; vendors and suppliers; contracting and other terms of participation, medical billing, reimbursement, claims administration and coordination, Medicare, Medicaid, CHIP, Medicare/Medicaid Advantage, ERISA and other payers and other provider-payer relations, contracting, compliance and enforcement; Form 990 and other nonprofit and tax-exemption; fundraising, investors, joint venture, and other business partners; quality and other performance measurement, management, discipline and reporting; physician and other workforce recruiting, performance management, peer review and other investigations and discipline, wage and hour, payroll, gain-sharing and other pay-for performance and other compensation, training, outsourcing and other human resources and workforce matters; board, medical staff and other governance; strategic planning, process and quality improvement; meaningful use, EMR, HIPAA and other technology, data security and breach and other health IT and data; STARK, ant kickback, insurance, and other fraud prevention, investigation, defense and enforcement; audits, investigations, and enforcement actions; trade secrets and other intellectual property; crisis preparedness and response; internal, government and third-party licensure, credentialing, accreditation, HCQIA and other peer review and quality reporting, audits, investigations, enforcement and defense; patient relations and care; internal controls and regulatory compliance; payer-provider, provider-provider, vendor, patient, governmental and community relations; facilities, practice, products and other sales, mergers, acquisitions and other business and commercial transactions; government procurement and contracting; grants; tax-exemption and not-for-profit; privacy and data security; training; risk and change management; regulatory affairs and public policy; process, product and service improvement, development and innovation, and other legal and operational compliance and risk management, government and regulatory affairs and operations concerns. to establish, administer and defend workforce and staffing, quality, and other compliance, risk management and operational practices, policies and actions; comply with requirements; investigate and respond to Board of Medicine, Health, Nursing, Pharmacy, Chiropractic, and other licensing agencies, Department of Aging & Disability, FDA, Drug Enforcement Agency, OCR Privacy and Civil Rights, Department of Labor, IRS, HHS, DOD, FTC, SEC, CDC and other public health, Department of Justice and state attorneys’ general and other federal and state agencies; JCHO and other accreditation and quality organizations; private litigation and other federal and state health care industry actions: regulatory and public policy advocacy; training and discipline; enforcement; and other strategic and operational concerns.
Author of leading works on HIPAA and a multitude of other health care, health plan and other health industry matters, the American Bar Association (ABA) International Section Life Sciences Committee Vice Chair, a Scribe for the ABA Joint Committee on Employee Benefits (JCEB) Annual OCR Agency Meeting and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her extensive publications and thought leadership as well as leadership involvement in a broad range of other professional and civic organizations. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- New PBGC Pension Rules Effective 3/5 May Require Action On Retirement Plans
- Revise Health Plan HIPAA Records Access Rules & Procedures To Use Newly Flexibility On Charging, Responding To Third Party PHI Requests
- 2/28 New Comment Deadline For NLRB Proposal To Exclude College Work Study Student Workers From NLRA Coverage
- Don’t Get Stuck Paying Another Employer’s Overtime Or Other Backpay
- 2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
- DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
- OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
- Salary Threshold Increases Require Employer Review Of Salaried Worker FLSA Exemption Qualification
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation considering the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law constantly and often rapidly evolves, subsequent developments that could impact the currency and completeness of this discussion are likely. The author and Solutions Law Press, Inc. disclaim, and have no responsibility to provide any update or otherwise notify anyone of any fact or law specific nuance, change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
Employers Prepare For Employment Tax Withholding Changes; Review & Comment On Proposed Rule Changes
February 25, 2020Employers and their payroll service provider should prepare for income and employment tax withholding changes expected when the Department of Treasury and Internal Revenue Service (IRS) finalize recently proposed rules on Income Tax Withholding From Wages intended to update the federal income tax withholding rules to reflect changes made by the Tax Cuts and Jobs Act (TCJA) and other legislation.
The proposed rules officially published in the Federal Register on February 13, 2020 available here follow up the agencies’ previous release of the resigned 2020 W-4, Employee’s Withholding Certificate by providing guidance to employers about the amount of federal income tax to withhold from employee’s wages following the TCJA.
The proposed regulations address numesrous income tax withholding and reporting changes made by TCJA to sections 3401 and 3402, but do not address withholding withholding on pensions, annuities, and certain other deferred income under section 3405(a) as the agencies separately addrress those rules in Notice 2020-3.
The agencies describe the proposed rules as providing “flexible and administrable rules for income tax withholding from wages intended to work with both the 2020 Form W-4 and its related tables and computational procedures described in Publication 15-T, and Forms W-4 and related tables and computational procedures provided in 2019 and earlier years.
As the proposed regulations are expected to impact the wage based tax information collection, withholding and reporting practices of most employers, every business paying wages subject to withholding will want to act quickly to review the proposed regulations to identify and begin preparations to implement the necessary changes in their systems and practices to comply with the proposed rules when finalized. Small or other employers or other stakeholders that wish to provide feedback on the proposed rules also will want to submit any comments before the comment period closes on April 13, 2020.
More Information
We hope this update is helpful. For more information about the Coix Order or other health or other employee benefits, human resources, or health care developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation; Former Chair of the RPTE Employee Benefits and Compensation Committee, the current Co-Chair of its Welfare Benefit Committee and former Chair of its Welfare Benefit, Plan Terminations, Fiduciary Responsibility and Defined Compensation Plan Committees; former RPTE Joint Committee on Employee Benefits Council (JCEB) Representative, Cynthia Marcotte Stamer is a Martindale-Hubble “AV-Preeminent” practicing attorney and management consultant, author, public policy advocate, author and lecturer repeatedly recognized for her 30 plus years’ of work and pragmatic thought leadership, publications and training on health, pension and other employee benefit, insurance, labor and employment, and health care fiduciary responsibility, payment, investment, contracting and other design, administration and compliance concerns as among the “Top Rated Labor & Employment Lawyers in Texas,” a “Legal Leader,” a “Top Woman Lawyer” and with other awards by LexisNexis® Martindale-Hubbell®; as among the “Best Lawyers In Dallas” for her work in the field of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, in International Who’s Who of Professionals and with numerous other awards and distinctions.
Highly valued for combining extensive legal and industry knowledge and experience with pragmatic creativity to help clients find and implement workable client-centric solutions, Ms. Stamer advises, represents and defends employers and other management clients and organizations; employer, union, multi-employer, association and other employee benefit plan plans, their sponsors, insurers and fiduciaries, plan administrators, administrative services, technology and other service providers, foreign and domestic governments, and others about employment and other services; health and welfare, pension, profit sharing other employee benefit and insurance program and policy management, administration, design and innovation, compliance, funding, documentation, communication, data security and use, contracting, plan, public and regulatory reforms and enforcement, and other risk management, compliance and operations matters. Her experience encompasses leading and supporting the development and defense of innovative new policies, programs, practices and solutions; advising and representing clients on routine plan establishment, plan documentation and contract drafting and review, administration, change and other compliance and operations; crisis prevention and response, compliance and risk management audits and investigations, enforcement actions and other dealings with the US Congress, Departments of Labor, Treasury, Health & Human Services, Federal Trade Commission, Justice, Securities and Exchange Commission, Education and other federal agencies, state legislatures, attorneys general, insurance, labor, worker’s compensation, and other agencies and regulators, and various other foreign and domestic governmental bodies and agencies. She also provides strategic and other supports clients in defending litigation as lead strategy counsel, special counsel and as an expert witness.
Alongside her extensive legal and operational experience, Ms. Stamer also is recognized for her work as a public and regulatory policy advocate and community leader with a gift for finding pragmatic solutions and helping to forge the common ground necessary to build consensus. Best known for her domestic public policy and community leadership on health care and insurance reform, Ms. Stamer’s lifelong public policy and community service involvement includes service as a lead consultant to the Government of Bolivia on its pension privatization project, as well as extensive legislative and regulatory reform, advocacy and input workforce, worker classification, employee benefit, public health and healthcare, social security and other disability and aging in place, education, migration reforms domestically and internationally throughout her adult life. In addition to her public and regulatory policy involvement, Ms. Stamer also contributes her service and leadership to a professional and civic organizations and efforts. Beyond her RPTE leadership involvements, these include her involvement as the Founder and Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE; Coalition on Patient Empowerment, a founding Board Member and past President of the Alliance for Healthcare Excellence; former Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; Vice Chair, Policy for the Life Sciences Committee of the ABA International Section, Chair of the ABA Intellectual Property Section Law Practice Management Committee, Past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group; former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, former Board Member, Continuing Education Chair and Treasurer of the Southwest Benefits Association; Vice President and Executive Director of the North Texas Healthcare Compliance Professionals Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; past Dallas World Affairs Council Board Member, and leadership of many other professional, civic and community organizations. Ms. Stamer also is a highly popular lecturer, symposia chair and author, who publishes and speaks extensively on health and managed care industry, human resources, employment and other privacy, data security and other technology, regulatory and operational risk management for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, the Society of Professional Benefits Administrators, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients, serves on the faculty and planning committee of many workshops, seminars, and symposia, and on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Beyond these involvements, Ms. Stamer also is active in the leadership of a broad range of other public policy advocacy and other professional and civic organizations and involvements. Through these and other involvements, she helps develop and build solutions, build consensus, garner funding and other resources, manage compliance and other operations, and take other actions to identify promote tangible improvements in health care and other policy and operational areas.
Before founding her current law firm, Cynthia Marcotte Stamer, P.C., Ms. Stamer practiced law as a partner with several prominent national and international law firms for more than 10 years before founding Cynthia Marcotte Stamer, P.C. to practice her unique brand of “Solutions law™” and to devote more time to the pragmatic policy and system reform, community education and innovation, and other health system improvement efforts of her PROJECT COPE: the Coalition on Patient Empowerment initiative.
Scribe for the ABA JCEB Annual Agency Meeting with OCR, Vice Chair of the ABA International Section Life Sciences Committee, past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group and the ABA RPTE Employee Benefits & Other Compensation Group, Ms. Stamer is most widely recognized for her decades of pragmatic, leading edge work, scholarship and thought leadership on health and other privacy and data security and other health industry legal, public policy and operational concerns. Ms. Stamer’s work throughout her 30 plus year career has focused heavily on working with health care and managed care, health and other employee benefit plan, insurance and financial services and other public and private organizations and their technology, data, and other service providers and advisors domestically and internationally with legal and operational compliance and risk management, performance and workforce management, regulatory and public policy and other legal and operational concerns. As a part of this work, she has continuously and extensively worked with domestic and international health plans, their sponsors, fiduciaries, administrators, and insurers; managed care and insurance organizations; hospitals, health care systems, clinics, skilled nursing, long term care, rehabilitation and other health care providers and facilities; medical staff, accreditation, peer review and quality committees and organizations; billing, utilization management, management services organizations, group purchasing organizations; pharmaceutical, pharmacy, and prescription benefit management and organizations; consultants; investors; EMR, claims, payroll and other technology, billing and reimbursement and other services and product vendors; products and solutions consultants and developers; investors; managed care organizations, self-insured health and other employee benefit plans, their sponsors, fiduciaries, administrators and service providers, insurers and other payers, health industry advocacy and other service providers and groups and other health and managed care industry clients as well as federal and state legislative, regulatory, investigatory and enforcement bodies and agencies.
This involvement encompasses helping health care systems and organizations, group and individual health care providers, health plans and insurers, health IT, life sciences and other health industry clients prevent, investigate, manage and resolve sexual assault, abuse, harassment and other organizational, provider and employee misconduct and other performance and behavior; manage Section 1557, Civil Rights Act and other discrimination and accommodation, and other regulatory, contractual and other compliance; vendors and suppliers; contracting and other terms of participation, medical billing, reimbursement, claims administration and coordination, Medicare, Medicaid, CHIP, Medicare/Medicaid Advantage, ERISA and other payers and other provider-payer relations, contracting, compliance and enforcement; Form 990 and other nonprofit and tax-exemption; fundraising, investors, joint venture, and other business partners; quality and other performance measurement, management, discipline and reporting; physician and other workforce recruiting, performance management, peer review and other investigations and discipline, wage and hour, payroll, gain-sharing and other pay-for performance and other compensation, training, outsourcing and other human resources and workforce matters; board, medical staff and other governance; strategic planning, process and quality improvement; meaningful use, EMR, HIPAA and other technology, data security and breach and other health IT and data; STARK, ant kickback, insurance, and other fraud prevention, investigation, defense and enforcement; audits, investigations, and enforcement actions; trade secrets and other intellectual property; crisis preparedness and response; internal, government and third-party licensure, credentialing, accreditation, HCQIA and other peer review and quality reporting, audits, investigations, enforcement and defense; patient relations and care; internal controls and regulatory compliance; payer-provider, provider-provider, vendor, patient, governmental and community relations; facilities, practice, products and other sales, mergers, acquisitions and other business and commercial transactions; government procurement and contracting; grants; tax-exemption and not-for-profit; privacy and data security; training; risk and change management; regulatory affairs and public policy; process, product and service improvement, development and innovation, and other legal and operational compliance and risk management, government and regulatory affairs and operations concerns. to establish, administer and defend workforce and staffing, quality, and other compliance, risk management and operational practices, policies and actions; comply with requirements; investigate and respond to Board of Medicine, Health, Nursing, Pharmacy, Chiropractic, and other licensing agencies, Department of Aging & Disability, FDA, Drug Enforcement Agency, OCR Privacy and Civil Rights, Department of Labor, IRS, HHS, DOD, FTC, SEC, CDC and other public health, Department of Justice and state attorneys’ general and other federal and state agencies; JCHO and other accreditation and quality organizations; private litigation and other federal and state health care industry actions: regulatory and public policy advocacy; training and discipline; enforcement; and other strategic and operational concerns.
Author of leading works on HIPAA and a multitude of other health care, health plan and other health industry matters, the American Bar Association (ABA) International Section Life Sciences Committee Vice Chair, a Scribe for the ABA Joint Committee on Employee Benefits (JCEB) Annual OCR Agency Meeting and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her extensive publications and thought leadership as well as leadership involvement in a broad range of other professional and civic organizations. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- New PBGC Pension Rules Effective 3/5 May Require Action On Retirement Plans
- Revise Health Plan HIPAA Records Access Rules & Procedures To Use Newly Flexibility On Charging, Responding To Third Party PHI Requests
- 2/28 New Comment Deadline For NLRB Proposal To Exclude College Work Study Student Workers From NLRA Coverage
- Don’t Get Stuck Paying Another Employer’s Overtime Or Other Backpay
- 2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
- DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
- OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
- Salary Threshold Increases Require Employer Review Of Salaried Worker FLSA Exemption Qualification
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation considering the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law constantly and often rapidly evolves, subsequent developments that could impact the currency and completeness of this discussion are likely. The author and Solutions Law Press, Inc. disclaim, and have no responsibility to provide any update or otherwise notify anyone of any fact or law specific nuance, change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
New PBGC Pension Rules Effective 3/5 May Require Action On Retirement Plans
February 3, 2020Defined benefit and other plan sponsors, fiduciaries, administrators, and their legal counsel and other service providers should review a new Pension Benefit Guarantee Final Regulation on Miscellaneous Corrections, Clarifications, and Improvements scheduled for publication tomorrow (February 4, 2020) that will make various key changes to the PBGC’s current regulations on n Reportable Events and Certain Other Notification Requirements, Annual Financial and Actuarial Information Reporting, Termination of Single-Employer Plans, and Premium Rates.
Generally scheduled to take effect March 5, 2020, the key changes implemented by the Final Regulations will include:
- Reportable Events – eliminating possible duplicative reporting of active participant reductions, clarifying when a liquidation occurs, and providing additional examples for certain events;
- Financial and Actuarial Information Reporting (“4010 filings”) – eliminating a requirement to submit individual financial information for each controlled group member;
- Standard Terminations – providing more time to file a post-distribution certification; and
- Premium Rates – clarifying the date on which participants are counted for premium calculations and emphasizing that a plan doesn’t qualify for the variable rate premium exemption for the year in which it completes a standard termination if it engages in a non-de minimis spinoff in the same year.
Highlights of Regulatory Changes
The rule changes generally take effect on March 5, 2020 (i.e., 30 days after publication, but certain provisions have different applicability dates (e.g., the changes first impact 4010 filings due on or after April 15, 2020). However, some requirements have later effective dates. For instance:
- The changes in 29 CFR 4006.5(f)(3), which deal with premium proration for short plan years where the plan’s assets are distributed in a termination, are applicable to plan years beginning in or after 2020;
- The changes in 29 CFR 4010.7(a)(2), § 4010.9(b)(2), and § 4010.11(a)(1)(i), which deal with identifying legal relationships of controlled group members, consolidated financial statements, and calculating the funding target for purposes of the 4010 funding shortfall waiver, respectively) are applicable to 4010 filings due or amended on or after April 15, 2020;
- The changes in § 4010.8(d)(2) for valuing benefit liabilities in cash balance plan account conversions are applicable to plan years beginning on or after January 1, 2020;
- The changes in 29 CFR 4041.29 are applicable to plan terminations for which, as March 5, 2020, the statutory deadline for certifying that plan assets have been distributed as required, has not passed; and
- The changes in 29 CFR 4043.23, § 4043.27(d)(3), § 4043.29, § 4043.30, 4043.31(c)(6), § 4043.32(c)(4), and § 4043.35(b)(3) (which deal with active participant reductions, changes in contributing sponsor or controlled group, liquidation, insolvency or similar settlement, and the public company waiver) are applicable to post-event reports for those reportable events occurring on or after March 5, 2020.
The PBGC says revised forms, instructions, and e-filing portal (reflecting the changes) are under review by OMB, which PBGC expects to be available for use by the effective date. (02/03/2020)
Required Action
With many of the changes in the Final Regulation slated to take effect on March 5, 2020, employer and other sponsors of defined benefit and other pension plans covered by the PBGC’s rules and their fiduciaries, plan administrators, actuaries and other service providers will want to evaluate the potential implication of the regulatory changes on their programs, its documentation, design, administration, reporting and other requirements and make any adjustments in a timely fashion. Employer and other plan sponsors, fiduciaries, administrators, advisors and service providers also will want to consider the advisability of modifying budget estimates, data collection and recordkeeping practices or other related activities and plans to account for the modified rules and responsibilities.
More Information
We hope this update is helpful. For more information about the Coix Order or other health or other employee benefits, human resources, or health care developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation; Former Chair of the RPTE Employee Benefits and Compensation Committee, the current Co-Chair of its Welfare Benefit Committee and former Chair of its Welfare Benefit, Plan Terminations, Fiduciary Responsibility and Defined Compensation Plan Committees; former RPTE Joint Committee on Employee Benefits Council (JCEB) Representative, Cynthia Marcotte Stamer is a Martindale-Hubble “AV-Preeminent” practicing attorney and management consultant, author, public policy advocate, author and lecturer repeatedly recognized for her 30 plus years’ of work and pragmatic thought leadership, publications and training on health, pension and other employee benefit, insurance, labor and employment, and health care fiduciary responsibility, payment, investment, contracting and other design, administration and compliance concerns as among the “Top Rated Labor & Employment Lawyers in Texas,” a “Legal Leader,” a “Top Woman Lawyer” and with other awards by LexisNexis® Martindale-Hubbell®; as among the “Best Lawyers In Dallas” for her work in the field of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, in International Who’s Who of Professionals and with numerous other awards and distinctions.
Highly valued for combining extensive legal and industry knowledge and experience with pragmatic creativity to help clients find and implement workable client-centric solutions, Ms. Stamer advises, represents and defends employers and other management clients and organizations; employer, union, multi-employer, association and other employee benefit plan plans, their sponsors, insurers and fiduciaries, plan administrators, administrative services, technology and other service providers, foreign and domestic governments, and others about employment and other services; health and welfare, pension, profit sharing other employee benefit and insurance program and policy management, administration, design and innovation, compliance, funding, documentation, communication, data security and use, contracting, plan, public and regulatory reforms and enforcement, and other risk management, compliance and operations matters. Her experience encompasses leading and supporting the development and defense of innovative new policies, programs, practices and solutions; advising and representing clients on routine plan establishment, plan documentation and contract drafting and review, administration, change and other compliance and operations; crisis prevention and response, compliance and risk management audits and investigations, enforcement actions and other dealings with the US Congress, Departments of Labor, Treasury, Health & Human Services, Federal Trade Commission, Justice, Securities and Exchange Commission, Education and other federal agencies, state legislatures, attorneys general, insurance, labor, worker’s compensation, and other agencies and regulators, and various other foreign and domestic governmental bodies and agencies. She also provides strategic and other supports clients in defending litigation as lead strategy counsel, special counsel and as an expert witness.
Alongside her extensive legal and operational experience, Ms. Stamer also is recognized for her work as a public and regulatory policy advocate and community leader with a gift for finding pragmatic solutions and helping to forge the common ground necessary to build consensus. Best known for her domestic public policy and community leadership on health care and insurance reform, Ms. Stamer’s lifelong public policy and community service involvement includes service as a lead consultant to the Government of Bolivia on its pension privatization project, as well as extensive legislative and regulatory reform, advocacy and input workforce, worker classification, employee benefit, public health and healthcare, social security and other disability and aging in place, education, migration reforms domestically and internationally throughout her adult life. In addition to her public and regulatory policy involvement, Ms. Stamer also contributes her service and leadership to a professional and civic organizations and efforts. Beyond her RPTE leadership involvements, these include her involvement as the Founder and Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE; Coalition on Patient Empowerment, a founding Board Member and past President of the Alliance for Healthcare Excellence; former Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; Vice Chair, Policy for the Life Sciences Committee of the ABA International Section, Chair of the ABA Intellectual Property Section Law Practice Management Committee, Past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group; former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, former Board Member, Continuing Education Chair and Treasurer of the Southwest Benefits Association; Vice President and Executive Director of the North Texas Healthcare Compliance Professionals Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; past Dallas World Affairs Council Board Member, and leadership of many other professional, civic and community organizations. Ms. Stamer also is a highly popular lecturer, symposia chair and author, who publishes and speaks extensively on health and managed care industry, human resources, employment and other privacy, data security and other technology, regulatory and operational risk management for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, the Society of Professional Benefits Administrators, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients, serves on the faculty and planning committee of many workshops, seminars, and symposia, and on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Beyond these involvements, Ms. Stamer also is active in the leadership of a broad range of other public policy advocacy and other professional and civic organizations and involvements. Through these and other involvements, she helps develop and build solutions, build consensus, garner funding and other resources, manage compliance and other operations, and take other actions to identify promote tangible improvements in health care and other policy and operational areas.
Before founding her current law firm, Cynthia Marcotte Stamer, P.C., Ms. Stamer practiced law as a partner with several prominent national and international law firms for more than 10 years before founding Cynthia Marcotte Stamer, P.C. to practice her unique brand of “Solutions law™” and to devote more time to the pragmatic policy and system reform, community education and innovation, and other health system improvement efforts of her PROJECT COPE: the Coalition on Patient Empowerment initiative.
Scribe for the ABA JCEB Annual Agency Meeting with OCR, Vice Chair of the ABA International Section Life Sciences Committee, past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group and the ABA RPTE Employee Benefits & Other Compensation Group, Ms. Stamer is most widely recognized for her decades of pragmatic, leading edge work, scholarship and thought leadership on health and other privacy and data security and other health industry legal, public policy and operational concerns. Ms. Stamer’s work throughout her 30 plus year career has focused heavily on working with health care and managed care, health and other employee benefit plan, insurance and financial services and other public and private organizations and their technology, data, and other service providers and advisors domestically and internationally with legal and operational compliance and risk management, performance and workforce management, regulatory and public policy and other legal and operational concerns. As a part of this work, she has continuously and extensively worked with domestic and international health plans, their sponsors, fiduciaries, administrators, and insurers; managed care and insurance organizations; hospitals, health care systems, clinics, skilled nursing, long term care, rehabilitation and other health care providers and facilities; medical staff, accreditation, peer review and quality committees and organizations; billing, utilization management, management services organizations, group purchasing organizations; pharmaceutical, pharmacy, and prescription benefit management and organizations; consultants; investors; EMR, claims, payroll and other technology, billing and reimbursement and other services and product vendors; products and solutions consultants and developers; investors; managed care organizations, self-insured health and other employee benefit plans, their sponsors, fiduciaries, administrators and service providers, insurers and other payers, health industry advocacy and other service providers and groups and other health and managed care industry clients as well as federal and state legislative, regulatory, investigatory and enforcement bodies and agencies.
This involvement encompasses helping health care systems and organizations, group and individual health care providers, health plans and insurers, health IT, life sciences and other health industry clients prevent, investigate, manage and resolve sexual assault, abuse, harassment and other organizational, provider and employee misconduct and other performance and behavior; manage Section 1557, Civil Rights Act and other discrimination and accommodation, and other regulatory, contractual and other compliance; vendors and suppliers; contracting and other terms of participation, medical billing, reimbursement, claims administration and coordination, Medicare, Medicaid, CHIP, Medicare/Medicaid Advantage, ERISA and other payers and other provider-payer relations, contracting, compliance and enforcement; Form 990 and other nonprofit and tax-exemption; fundraising, investors, joint venture, and other business partners; quality and other performance measurement, management, discipline and reporting; physician and other workforce recruiting, performance management, peer review and other investigations and discipline, wage and hour, payroll, gain-sharing and other pay-for performance and other compensation, training, outsourcing and other human resources and workforce matters; board, medical staff and other governance; strategic planning, process and quality improvement; meaningful use, EMR, HIPAA and other technology, data security and breach and other health IT and data; STARK, ant kickback, insurance, and other fraud prevention, investigation, defense and enforcement; audits, investigations, and enforcement actions; trade secrets and other intellectual property; crisis preparedness and response; internal, government and third-party licensure, credentialing, accreditation, HCQIA and other peer review and quality reporting, audits, investigations, enforcement and defense; patient relations and care; internal controls and regulatory compliance; payer-provider, provider-provider, vendor, patient, governmental and community relations; facilities, practice, products and other sales, mergers, acquisitions and other business and commercial transactions; government procurement and contracting; grants; tax-exemption and not-for-profit; privacy and data security; training; risk and change management; regulatory affairs and public policy; process, product and service improvement, development and innovation, and other legal and operational compliance and risk management, government and regulatory affairs and operations concerns. to establish, administer and defend workforce and staffing, quality, and other compliance, risk management and operational practices, policies and actions; comply with requirements; investigate and respond to Board of Medicine, Health, Nursing, Pharmacy, Chiropractic, and other licensing agencies, Department of Aging & Disability, FDA, Drug Enforcement Agency, OCR Privacy and Civil Rights, Department of Labor, IRS, HHS, DOD, FTC, SEC, CDC and other public health, Department of Justice and state attorneys’ general and other federal and state agencies; JCHO and other accreditation and quality organizations; private litigation and other federal and state health care industry actions: regulatory and public policy advocacy; training and discipline; enforcement; and other strategic and operational concerns.
Author of leading works on HIPAA and a multitude of other health care, health plan and other health industry matters, the American Bar Association (ABA) International Section Life Sciences Committee Vice Chair, a Scribe for the ABA Joint Committee on Employee Benefits (JCEB) Annual OCR Agency Meeting and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her extensive publications and thought leadership as well as leadership involvement in a broad range of other professional and civic organizations. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- 2/28 New Comment Deadline For NLRB Proposal To Exclude College Work Study Student Workers From NLRA Coverage
- Don’t Get Stuck Paying Another Employer’s Overtime Or Other Backpay
- 2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
- DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
- OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
- Salary Threshold Increases Require Employer Review Of Salaried Worker FLSA Exemption Qualification
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation considering the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law constantly and often rapidly evolves, subsequent developments that could impact the currency and completeness of this discussion are likely. The author and Solutions Law Press, Inc. disclaim, and have no responsibility to provide any update or otherwise notify anyone of any fact or law specific nuance, change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
Revise Health Plan HIPAA Records Access Rules & Procedures To Use Newly Flexibility On Charging, Responding To Third Party PHI Requests
January 28, 2020Health plans and their health plan records providers and other business associates should review and update their existing policies and practices concerning providing and charging individuals for access to protected health information in response to modifications in the Department of Health & Human Service (“HHS”) Office of Civil Rights (“OCR”) rules implementing the Health Insurance Portability & Accountability Act (“HIPAA”) requirements regarding patient’s rights to access their protected health information (“PHI”) from health plans, health care providers, health care clearinghouses (“”Covered Entities”) and their business associates (“HIPAA entities”) to comply with a January 23, 2020 court order (the “Coix Order”) in Coix Health, LLC v. Azar, et al, No 18 –CV-0040 (D>D.C. January 23, 2020). Utilizing the flexibility resulting from the Coix Order could help reduce health plan costs of compliance with the HIPAA right of access rule by allowing the health plan and its records providers more freedom to determine the charges and format for delivering PHI in response to records requests received from other insurers, lawyers and other third parties.
Coix Order Invalidates Pieces of OCR HIPAA Rules On PHI Record Rules
The new flexibility is the result of the Coix Order entered by a Federal District Court in response to a lawsuit brought by Coix Health, LLC (“”Coix”). Coix brought the lawsuit challenging the “Patient Rate” restrictions on the amounts that HIPAA entities can charge for providing records containing PHI the “third party directive” requirements in the rules implementing HIPAA’s right of access requirements under 45 C.F.R. §164.524 as adopted by OCR as part of its final rule entitled “Modifications to the HIPAA Privacy, Security, and Enforcement Rules Under the Health Information Technology for Economic and Clinical Health Act, and the Genetic Information Nondiscrimination Act; Other Modifications to the HIPAA Rules.” (The “2013 Omnibus Rule”) on January 25, 2013. In particular, the 2013 Omnibus Rule includes a “Patient Rate” rule that limits the charges that Covered Entities can make for delivering PHI requested by patients and third parties to prevent patient access to PHI from being thwarted by excessive fees. As part of the Patient Rate rule, OCR restricted what Covered Entities and their records providers can charge to provide copies of protected health information. The Patient Rate rule restricts charges that can be imposed to provide protected health information, restricts the methods for calculating these charges and limits the type and amount of labor costs that can be included when calculating the Patient Rate. The Patient Rate rule in the 201 Omnibus Rule also requires that Covered Entities and their records companies provide the requested PHI directly to the patient or to a third party designed by the patient and in the format requested by the patient regardless of the format in which the Covered Entity or its medical provider maintains the PHI within its record.
When originally implemented, the medical records industry generally understood that the Patient Rate limitations applied only to requests for PHI made by the patient for use by the patient. Before 2016, however, Covered Entities and their medical records providers generally understood that this Patient Rate rule did not apply to or limit fees that Covered Entities or their medical records providers could charge commercial entities or other third parties like insurance companies and law firms to fill requests for PHI. That understanding changed, in 2016, however, when HHS issued guidance that stated that the Patient Rate applies even to requests to deliver PHI to third parties.
A specialized medical-records provider that contracts with healthcare suppliers nationwide to maintain, retrieve, and produce individuals’ PHI, Cox handles tens of millions of requests for records containing PHI annually including demands by healthcare providers for treatment purposes, patients asking for their own PHI, and third parties, such as life insurance companies and law firms, seeking a patient’s PHI for commercial or legal reasons. According to Cox, OCR’s interpretation of the Patient Rate rule as applicable to third party requests as well as direct patient requests cost it and other medical records companies millions of dollars in revenue. Accordingly, Coix filed the Coix Health, LLC v. Azar, et al lawsuit challenging OCR’s 2016 application of the Patient Rate to third party requests as violating the procedural and substantive protections of the Administrative Procedure Act (“APA”). In addition to this challenge to the scope of the Patient Rate, Coix also contested OCR pronouncements in the 2016 guidance document on (1) the types of labor costs that are recoverable under the Patient Rate; and (2) the three alternative methods identified for calculating the Patient Rate as violating the APA’s procedural and substantive provisions. Finally, Coix also challenged the requirement in the Patient Rate rule that records companies to send PHI to third parties regardless of the format in which the PHI is contained and in the format specified by the patient. According to Coix, Congress required only that certain types of electronic health records be delivered to third parties, not all records regardless of their format, as HHS’s regulations now command.
In its January 23, 2020 ruling on HHS’s motion to dismiss and the parties’ cross-motions for summary judgment, the D.C. District Court agreed with OCR that OCR’s rule requiring the use of one of three methods for calculating the Patient Rate was unreviewable as a final agency action and dismissed Coix’ challenge to that requirement. Concerning Coax’s other challenges, the Court sided with Coix. It ruled that:
- OCR’s 2013 rule compelling delivery of PHI to third parties regardless of the records’ format is arbitrary and capricious insofar as it goes beyond the statutory requirements set by Congress;
- OCR’s broadening of the Patient 3 Rate in 2016 is a legislative rule that the agency failed to subject to notice and comment in violation of the APA; and
- OCR’s 2016 explanation concerning what labor costs can be recovered under the Patient Rate is an interpretative rule that OCR was not required to subject to notice and comment.
Accordingly, District Court in the Coix Order declares unlawful and vacates (1) the 2016 Patient Rate expansion and (2) the 2013 mandate broadening PHI delivery to third parties regardless of format within the individual right of access” set forth in the provisions of 45 C.F.R. §164.524 of the 2013 Omnibus Rule insofar as it expands the HITECH Act’s third-party directive beyond requests for a copy of an electronic health record with respect to protected health information of an individual in an electronic format.” Additionally, the federal court ordered that the fee limitation set forth at 45 C.F.R. § 164.524(c)(4) only apply to an individual’s request for access to their own records, and does not apply to an individual’s request to transmit records to a third party.
As a result of the Coix Order, Covered Entities and their medical records providers still must calculate the Patient Rate in accordance with one of the three allowed methodologies when providing a patient with records containing PHI in response to a patient request. However, Covered Entities and their medical records provider now may exercise greater flexibility when determining the format and charges when responding to requests from third parties other than the patient for records containing PHI. Before doing so, however, most Covered Entities and business associates will want to update their HIPAA policies and procedures to reflect the new practices consistent with the new HIPAA and other relevant requirements. Updating the policies first is important because the 2013 Omnibus Rule states Covered Entities violate HIPAA by failing to follow their own HIPAA privacy and security policies when those practices are more restrictive than those mandated by OCR’s 2013 Omnibus Rule. Consequently however, Covered Entities and their medical records companies desiring to exercise this newly available flexibility should revise their existing policies and procedures to authorize their exercise of this new flexibility consistent with the Coix Order and associated OCR guidance.
OCR Plans To Comply With Coix Order In Applying Patient Record Rule
In an “Important Notice Regarding Individuals’ Right of Access to Health Records” released January 28, 2020, OCR announced that that it will comply with the Coix Order vacating the “third-party directive” within the individual right of access “insofar as it expands the HITECH Act’s third-party directive beyond requests for a copy of an electronic health record with respect to [protected health information] of an individual . . . in an electronic format.” Additionally, OCR stated that the fee limitation set forth at 45 C.F.R. § 164.524(c)(4) will apply only to an individual’s request for access to their own records, and not apply to an individual’s request to transmit records to a third party. However, OCR also added that the right of individuals to access their own records and the fee limitations that apply when exercising this right are undisturbed and remain in effect. OCR will continue to enforce the right of access provisions in 45 C.F.R. § 164.524 that are not restricted by the court order.
More Information
We hope this update is helpful. For more information about the Coix Order or other health or other employee benefits, human resources, or health care developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of health industry and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Scribe for the ABA JCEB Annual Agency Meeting with OCR, Vice Chair of the ABA International Section Life Sciences Committee, past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group and the ABA RPTE Employee Benefits & Other Compensation Group, Ms. Stamer’s work throughout her 30 plus year career has focused heavily on working with health care and managed care, health and other employee benefit plan, insurance and financial services and other public and private organizations and their technology, data, and other service providers and advisors domestically and internationally with legal and operational compliance and risk management, performance and workforce management, regulatory and public policy and other legal and operational concerns. As a part of this work, she has continuously and extensively worked with domestic and international health plans, their sponsors, fiduciaries, administrators, and insurers; managed care and insurance organizations; hospitals, health care systems, clinics, skilled nursing, long term care, rehabilitation and other health care providers and facilities; medical staff, accreditation, peer review and quality committees and organizations; billing, utilization management, management services organizations, group purchasing organizations; pharmaceutical, pharmacy, and prescription benefit management and organizations; consultants; investors; EMR, claims, payroll and other technology, billing and reimbursement and other services and product vendors; products and solutions consultants and developers; investors; managed care organizations, self-insured health and other employee benefit plans, their sponsors, fiduciaries, administrators and service providers, insurers and other payers, health industry advocacy and other service providers and groups and other health and managed care industry clients as well as federal and state legislative, regulatory, investigatory and enforcement bodies and agencies.
Ms. Stamer is most widely recognized for her decades of pragmatic, leading edge work, scholarship and thought leadership on health and other privacy and data security and other health industry legal, public policy and operational concerns. This involvement encompasses helping health care systems and organizations, group and individual health care providers, health plans and insurers, health IT, life sciences and other health industry clients prevent, investigate, manage and resolve sexual assault, abuse, harassment and other organizational, provider and employee misconduct and other performance and behavior; manage Section 1557, Civil Rights Act and other discrimination and accommodation, and other regulatory, contractual and other compliance; vendors and suppliers; contracting and other terms of participation, medical billing, reimbursement, claims administration and coordination, Medicare, Medicaid, CHIP, Medicare/Medicaid Advantage, ERISA and other payers and other provider-payer relations, contracting, compliance and enforcement; Form 990 and other nonprofit and tax-exemption; fundraising, investors, joint venture, and other business partners; quality and other performance measurement, management, discipline and reporting; physician and other workforce recruiting, performance management, peer review and other investigations and discipline, wage and hour, payroll, gain-sharing and other pay-for performance and other compensation, training, outsourcing and other human resources and workforce matters; board, medical staff and other governance; strategic planning, process and quality improvement; meaningful use, EMR, HIPAA and other technology, data security and breach and other health IT and data; STARK, ant kickback, insurance, and other fraud prevention, investigation, defense and enforcement; audits, investigations, and enforcement actions; trade secrets and other intellectual property; crisis preparedness and response; internal, government and third-party licensure, credentialing, accreditation, HCQIA and other peer review and quality reporting, audits, investigations, enforcement and defense; patient relations and care; internal controls and regulatory compliance; payer-provider, provider-provider, vendor, patient, governmental and community relations; facilities, practice, products and other sales, mergers, acquisitions and other business and commercial transactions; government procurement and contracting; grants; tax-exemption and not-for-profit; privacy and data security; training; risk and change management; regulatory affairs and public policy; process, product and service improvement, development and innovation, and other legal and operational compliance and risk management, government and regulatory affairs and operations concerns. to establish, administer and defend workforce and staffing, quality, and other compliance, risk management and operational practices, policies and actions; comply with requirements; investigate and respond to Board of Medicine, Health, Nursing, Pharmacy, Chiropractic, and other licensing agencies, Department of Aging & Disability, FDA, Drug Enforcement Agency, OCR Privacy and Civil Rights, Department of Labor, IRS, HHS, DOD, FTC, SEC, CDC and other public health, Department of Justice and state attorneys’ general and other federal and state agencies; JCHO and other accreditation and quality organizations; private litigation and other federal and state health care industry actions: regulatory and public policy advocacy; training and discipline; enforcement; and other strategic and operational concerns.
Author of leading works on HIPAA and a multitude of other health care, health plan and other health industry matters, the American Bar Association (ABA) International Section Life Sciences Committee Vice Chair, a Scribe for the ABA Joint Committee on Employee Benefits (JCEB) Annual OCR Agency Meeting and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her extensive publications and thought leadership as well as leadership involvement in a broad range of other professional and civic organizations. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- 2/28 New Comment Deadline For NLRB Proposal To Exclude College Work Study Student Workers From NLRA Coverage
- Don’t Get Stuck Paying Another Employer’s Overtime Or Other Backpay
- 2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
- DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
- OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation considering the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law constantly and often rapidly evolves, subsequent developments that could impact the currency and completeness of this discussion are likely. The author and Solutions Law Press, Inc. disclaim, and have no responsibility to provide any update or otherwise notify anyone of any fact or law specific nuance, change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
Don’t Get Stuck Paying Another Employer’s Overtime Or Other Backpay
January 13, 2020No business wants to get hit with a bill or judgement for unpaid overtime or other wages and penalties under the Fair Labor Standards Act (“FLSA”). It’s even worse when the order to pay is for back pay another business owed but didn’t pay. New FLSA joint employer regulations released today update the rules about when your business could get stuck paying another business’ backpay. That’s why all U.S. employers should re-evaluate their potential minimum wage, overtime, recordkeeping and other Fair Labor Standards Acts (“FLSA”) liability exposure from work performed by workers employed by subcontractors or contractors, staffing, leasing, manpower and workforce and other separate business entities in light of the new Final Rule: Joint Employer Status under the Fair Labor Standards Act (“Final Rule”) on determining joint employer status under the FLSA released by the Department of Labor Wage and Hour Division (“Labor Department”). The Labor Department released a copy of the Final Rule to the public today today (January 13, 2020) in anticipation of its scheduled official publication in the Federal Register on January 16, 2019.
Joint Employer Liability Long Standing FLSA Risk
Many businesses and their management are unaware that if their business meets the definition of a “joint employer” for purposes of the FLSA, their businesses could be required to pay unpaid wages and penalties another business owes for failing to pay minimum wage or overtime or other FLSA violations. even though their business never directly employed those workers. This is because the FLSA also makes business that are “joint employers” as defined for purposes of the FLSA jointly and severally liable with the direct employer for proper payment of wages and other compliance with the FLSA. The FLSA requires covered employers to pay their employees at least the federal minimum wage for every hour worked and overtime for every hour worked over 40 in a workweek. To be liable for paying minimum wage or overtime, an individual or entity must be an “employer,” which the FLSA defines in Section 3(d) to include “any person acting directly or indirectly in the interest of an employer in relation to an employee[.]” Under the FLSA, an employee may have—in addition to his or her employer—one or more joint employers. A joint employer is any additional “person” (i.e., an individual or entity) who is jointly and severally liable with the employer for the employee’s wages under the applicable Labor Department regulations.
While both the Labor Department and private litigants have used the joint employer rules and precedent to nail businesses for other employer’s wage and hour liability frequently for the past sixty plus years, Obama Administration changes in the Labor Department’s interpretation and enforcement of the joint employer rule have significantly broadened the scope of relationships found to constitute joint employment to include a broad range of subcontractor and other business relationships not historically recognized as triggering joint employer liability. Historically, joint employer determinations were reached by applying highly subjective, fact specific analysis heavily reliant upon decades of court decisions which required some evidence that the alleged joint employer possessed or exercised some control over the employees to support the finding of joint employment. Under these historical tests, mere benefit from work performed by individuals employed by another employer did not establish a presumption, much less proof of joint employment.
During the Obama Administration, however, the Department of Labor both stepped up its efforts to identify and enforce these joint employer provisions and concurrently without formally issuing new regulations adopted interpretive and enforcement guidelines for finding joint employer status that that significantly broadened the employment relationships that the Labor Department treated as joint employers in a manner that presumed the existence of a joint employment relationship whenever the alleged joint employer benefitted from the performance of work even when the facts showed little or any evidence that the alleged joint employer possessed or exercised any control over the employee or the details of his work. As a consequences, construction and other businesses uses contractors, health care organizations, and a host of other entities were surprised to be nailed with wage and hour liabilities arising from work performed by subcontractors, contractors, and other businesses including overtime liability attributable to work performed for the benefit of other customers of the employer.
Final Joint Employer Rule Changes Rules Effective March 16, 2020
Prompted by the Trump Administration’s broader effort to roll back these and other Obama Era pro-labor rulemaking and enforcement, the new Final Rule seeks to restore and reaffirm the requirement of evidence of the possession of authority or exercise of some traditional employer control by the alleged joint employer. Scheduled to take effect on March 16, 2020, the new Final Rule will continue to recognize two potential scenarios where an employee may have one or more joint employers based on a highly subjective analysis of the factual realities of an alleged joint employer with another business or businesses under two scenarios:
- The employee has an employer who suffers, permits, or otherwise employs the employee to work, but another individual or entity simultaneously benefits from that work (“Scenario One”); versus
- One employer employs an employee for one set of hours in a workweek, and another employer employs the same employee for a separate set of hours in the same workweek (“Scenario Two”).
The Final Rule modifies and clarifies the Labor Department’s historical joint employer rule as it relates to the determination of joint employment status in Scenario One situations but leaves substantially unchanged its existing rules on joint employer determinations in Scenario Two situations.
Finally, the Final Rule provides several examples of how the Department’s joint employer guidance should be applied in various factual circumstances
Final Rule Modifications To Existing Rules On Joint Employment in Scenario One Situations
Under the Final Rule in a Scenario One situation under which an employee performs work for the employer that simultaneously benefits another individual or entity, the Final Rule adopts a four-factor balancing test to determine whether the potential joint employer is directly or indirectly controlling the employee, assessing whether the potential joint employer:
- hires or fires the employee;
- supervises and controls the employee’s work schedule or conditions of employment to a substantial degree;
- determines the employee’s rate and method of payment; and
- maintains the employee’s employment records.
Businesses should keep in mind that proof of the exercise of exercise direct control over these details of employment of an employee is not required for a finding of joint employment. Indirect exercise of control is sufficient. Examples of indirect exercise of control recognized in the Final Regulations as supporting joint employer liability include control over an employee through mandatory directions to another employer that directly control the employee. However, indirect control does not include the direct employer’s voluntary decision to accommodate the potential joint employer’s request, recommendation, or suggestion. Similarly, acts that incidentally impact the employee do not indicate joint employer status. For example, a restaurant could request lower fees from its cleaning contractor, which, if agreed to, could impact the wages of the cleaning contractor’s employees. However, this request would not constitute an exercise of indirect control over the employee’s rate of payment.
Like under the prior rules and standards, whether a person is a joint employer under the new standards established in the Final Rule will continue to depend upon all the facts in a particular case, and the appropriate weight to give each factor will vary depending on the circumstances. Moreover, all of these factors need not be present for joint employment to exist. However, the Final Rule states the potential joint employer’s maintenance of the employee’s employment records alone will not lead to a finding of joint employer status. For purposes of its provisions, the Final Rule defines the “employment records” referred to in the fourth factor to mean only those records, such as payroll records, that reflect, relate to, or otherwise record information pertaining to the hiring or firing, supervision and control of the work schedules or conditions of employment, or determining the rate and method of payment of the employee.
Additionally, the Final Rule also notes that additional factors may also be relevant in determining whether another person is a joint employer in this situation, but only when they show whether the potential joint employer is exercising significant control over the terms and conditions of the employee’s work.
The Final Rule also identifies factors that are not relevant to the determination of FLSA joint employer status. For example, the Final Rule specifies that whether the employee is economically dependent on the potential joint employer, including factors traditionally used to establish whether a particular worker is a bona fide independent contractor (e.g., the worker’s opportunity for profit or loss, their investment in equipment and materials, etc.), are not relevant to determine joint employer liability. Economic dependence was an evidentiary factor promoted as evidence of joint employment in several Obama Administration era enforcement actions.
The Final Rule also identifies certain other factors that do not make joint employer status more or less likely under the Act which had been relied upon by the Labor Department under the Obama Administration era interpretation of the FLSA, including:
- operating as a franchisor or entering into a brand and supply agreement, or using a similar business model;
- the potential joint employer’s contractual agreements with the employer requiring the employer to comply with its legal obligations or to meet certain standards to protect the health or safety of its employees or the public;
- the potential joint employer’s contractual agreements with the employer requiring quality control standards to ensure the consistent quality of the work product, brand, or business reputation; and
- the potential joint employer’s practice of providing the employer with a sample employee handbook, or other forms, allowing the employer to operate a business on its premises (including “store within a store” arrangements), offering an association health plan or association retirement plan to the employer or participating in such a plan with the employer, jointly participating in an apprenticeship program with the employer, or any other similar business practice.
Additionally, the Final Rule makes clear that a finding of joint employer status in Scenario One situations must be based on an actual exercise of control by the alleged joint employer. In this respect, the Final Rule provides that although an individual or entity’s power, ability, or reserved contractual right to exercise control relating to one or more of the factors may be relevant in determining whether they are an FLSA joint employer, such power, ability, or reserved contractual rights are not in themselves sufficient to establish FLSA joint employer status without some actual exercise of control.
Final Rule Retains Existing Rules On Joint Employment In Scenario Two Situations
The Final Rule did not make any substantive changes to the standard for determining joint employer liability in Scenario Two situations. If the employers are acting independently of each other and are disassociated with respect to the employment of the employee, the Final Rule continues to provide that each employer may disregard all work performed by the employee for the other employer in determining its liability under the FLSA. However, if the factual realities show that the employers are sufficiently associated with respect to the employment of the employee, the Final Rule continues to state that the two businesses are joint employers and must aggregate the hours worked for each for purposes of determining if they are in compliance.
For purposes of the Scenario Two analysis, the Final Rule provides that employers generally will be sufficiently associated if there is an arrangement between them to share the employee’s services, the employer is acting directly or indirectly in the interest of the other employer in relation to the employee, or they share control of the employee, directly or indirectly, by reason of the fact that one employer controls, is controlled by, or is under common control with the other employer. Employers using manpower, staffing, employee leasing or other shared or part time workforces should keep in mind that a finding that their business is a joint employer with the supplier of the workers can result in liability for their business associated both for hours of work performed for the benefit of their business as well as any work the employee worked for another client of the supplier business. As these shared workforces often perform work for several competitors, ironically this often means that a joint employer often ends up payment overtime liability attributable to unpaid overtime or other wages performed for a competitor business or businesses that also are clients of the same partial workforce supplier.
Businesses Should Act To Assess & Mitigate Joint Employer & Other FLSA Liability
The Labor Departments that its adoption of the revisions to the joint employer rule made by the Final Rule will add greater certainty regarding what business practices may result in joint employer status: and promote greater uniformity among court decisions by providing a clearer interpretation of FLSA joint employer status. While the clarifications may help businesses to better predict certain relationships and arrangements that carry a higher risk of joint employer liability exposure, businesses must keep in mind that joint employer determinations under the Final Rule will continue to turn on highly subjective analysis of facts and circumstances that existing precedent suggests often finds the requisite evidence to find a joint employer relationship in many circumstances surprising to many business owners even taking into account the modifications made by the Final Rule, For this reason, virtually all businesses generally will want to critically evaluate their existing and prospective relationships for potential joint employer liability under the FLSA in light of the Final Regulations.
Businesses should look to the guidance in the new Final Rule initially to evaluate whether their existing or prospective relationships meet, or could be restructured to meet all of the requisites to avoid or reduce the risk of findings of joint employer status. When possible, businesses should seek to structure their contractual relationships and business dealings with other businesses to fit as closely as possible with those arrangements that the new Final Regulations identify as not constituting joint employer relationships in form and operation. When engaging in these efforts, businesses need to look beyond their contractual agreements to examine the factual realities of their relationships with other businesses realistically based upon a clear understanding of the historical precedent to avoid mischaracterizing their relationships and their associated risks. For added protection, businesses also should consider seeking contractual representations of compliance, coupled with requirements that other businesses whose employment practices could create joint employment risk provide records and other documentation needed to verify compliance and defend against potential joint employer liability claims.
Concurrently, businesses looking at FLSA joint employer liability risk management also should keep in mind that the new Final Rule only addresses joint employer determinations under the FLSA. This Final Rule does not address “joint employer” status or other characterizations of relationships under other federal employment laws, such as the National Labor Relations Act (NLRA), the Employee Retirement Income Security Act of 1974 (ERISA), the Migrant and Seasonal Agricultural Worker Protection Act, Title VII of the Civil Rights Act, state labor, tax, unemployment, workers’ compensation or other laws, which often apply different standards for finding joint employment or other imputed liability of businesses other than the direct or nominal employer. While different rules apply for those laws, government agencies and private litigants also increasingly successfully assert joint employer or other theories to impute liability to businesses that are not the nominal employer of workers protected by these laws. To effectively plan for a control their broader joint employer risk, most businesses benefit from looking at their exposure holistically taking into account the potential characterization and liabilities under all of these rules concurrently.
Before beginning these assessments, businesses and their leaders are encouraged to engage an attorney experienced in FLSA and other joint employer and other worker classification laws in light of the legally sensitive evidence and discussions inherently involved in this process. Conducting this analysis within the scope of attorney-client privilege helps protector limit the discoverability of sensitive discussions and work product in the event of a Labor Department investigation or litigation.
For More Information
We hope this update is helpful. For more information about this or other labor and employment developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Law and Labor and Employment Law and Health Care; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of health industry and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Ms. Stamer’s work throughout her 30 plus year career has focused heavily on working with health care and managed care, health and other employee benefit plan, insurance and financial services, construction, manufacturing, staffing and workforce and other public and private organizations and their technology, data, and other service providers and advisors domestically and internationally with legal and operational compliance and risk management, performance and workforce management, regulatory and public policy and other legal and operational concerns. As a part of this work, she has continuously and extensively worked with domestic and international employer and other management, employee benefit and other clients to assess, manage and defend joint employer and other worker classifications and practices under the FLSA and other federal and state laws including both advising and and assisting employers to minimize joint employer and other FLSA liability and defending a multitude of employers against joint employer and other FLSA and other worker classification liability. She also has been heavily involved in advocating for the Trump Administration’s restoration of more historical principles for determining and enforcing joint employer liability over the past several years.
Author of hundreds of highly regarded books, articles and other publications, Ms. Stamer also is widely recognized for her scholarship, coaching, legislative and regulatory advocacy, leadership and mentorship on wage and hour, worker classification and a diverse range of other labor and employment, employee benefits, health and safety, education, performance management, privacy and data security, leadership and governance, and other management concerns within the American Bar Association (ABA), the International Information Security Association, the Southwest Benefits Association, and a variety of other international, national and local professional, business and civic organizations including highly regarded works on worker reclassification and joint employment liability under the FLSA and other laws published by the Bureau of National Affairs and others. Examples of these involvements include her service as the ABA Intellectual Property Law Section Law Practice Management Committee; the ABA International Section Life Sciences and Health Committee Vice Chair-Policy; a Scribe for the ABA Joint Committee on Employee Benefits (JCEB) Annual OCR Agency Meeting and a former JCEB Council Representative and Marketing Chair; Past Chair of the ABA RPTE Employee Benefits and Other Compensation Group and Vice Chair of its Law Practice Management Committee; Past Chair of the ABA Managed Care & Insurance Interest Group; former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Southwest Benefits Association Board member; past Texas Association of Business State Board Member, BACPAC Committee Meeting, Regional and Dallas Chapter Chair; past Dallas Bar Association Employee Benefits Committee Executive Committee; former SHRM Region IV Chair and National Consultants Forum Board Member; for WEB Network of Benefit Professionals National Board Member and Dallas Chapter Chair; former Dallas World Affairs Council Board Member; founding Board Member, past President and Patient Empowerment and Health Care Heroes founder for the Alliance for Health Care Excellence; former Gulf States TEGE Council Exempt Organizations Coordinator and Board member; past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and involvement in a broad range of other professional and civic organizations. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- 2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
- DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
- OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- Comment on Interim Domestic Hemp Production Rules By 12/30n. L ok
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
- Salary Threshold Increases Require Employer Review Of Salaried Worker FLSA Exemption Qualification
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The author and Solutions Law Press, Inc. disclaim, and have no responsibility to provide any update or otherwise notify anyone any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2020 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
2019 OCR Enforcement Shows Getting Defensibly HIPAA Compliant Necessary In 2020!
January 1, 2020The $65,000 payment and corrective action plan commitments West Georgia Ambulance, Inc. (“West Georgia”) is making to settle Department of Health & Human Services Office for Civil Rights (“OCR”) charges it recurrently violated the Health Insurance Portability and Accountability Act (“HIPAA”) Security Rule and other 2019 HIPAA enforcement sends a clear warning to other HIPAA-covered health plans, health care providers, health care clearighouses and their business associates (“covered entities”) to maintain and be prepared to defend their own HIPAA compliance.
The Western Georgia Resolution Agreement and Corrective Action Plan (“Resolution Agreement”) OCR announced on December 30, 2019 resolves charges resulting from an OCR investigation initiated in response to a HIPAA breach report the Georgia based ambulance company filed in 2013 in which the company, which provides emergency and non-emergency ambulance services in Carroll County, Georgia, disclosed the loss of an unencrypted laptop containing the protected health information (PHI) of 500 individuals. The breach occurred when an unencrypted laptop fell off the back bumper of an ambulance. The laptop was not recovered. West Georgia reported that exactly 500 individuals were affected by the breach.
In the course of its investigation of the breach report, OCR’s investigation uncovered long-standing noncompliance with the HIPAA Rules, including failures to conduct a risk analysis, provide a security awareness and training program, and implement HIPAA Security Rule policies and procedures. Specifically, the Resolution Agreement states that West Georgia:
- Did not conduct an accurate and thorough risk analysis of the potential risks and vulnerabilities to the confidentiality, integrity, and availability of all of its ePHI. See 45 C.F.R. § 164.308(a)(1)(ii)(A);
- Failed to have a HIPAA security training program, and failed to provide security training to its employees. See 45 C.F.R. § 164.308(a)(5);
- Failed to implement Security Rule policies or procedures. See 45 C.F.R. § 164.316; and
- Despite OCR’s investigation and technical assistance, “did not take meaningful steps to address their systemic failures.”
To resolve its exposure to the substantially higher civil monetary penalties that OCR could impose for violations of this nature, West Georgia agreed to pay a $65,000 resolution payment to OCR and implement and comply with a corrective action plan that in addition to requiring West Georgia to correct the compliance deficiencies, also subjects West Georgia to two years of OCR monitoring and oversight.
The Resolution Agreement and corrective action plan carry a number of important messages for other health care providers and other Covered Entities. First, the OCR enforcement action against West Georgia coming at the end of yet another heavy HIPAA enforcement year by OCR reminds Covered Entities that OCR is serious about HIPAA enforcement on the heels of its 2018 HIPAA record setting collection of $28.7 million in civil monetary penalties and resolution payments including the single largest individual HIPAA settlement in history of $16 million with Anthem, Inc. See OCR Concludes 2018 with All-Time Record Year for HIPAA Enforcement. While not topping this record, OCR during 2019 now has collected civil monetary penalties and resolution payments totaling more than $15 million from HIPAA Covered Entities and their business associates including:
- A $3 Million Resolution Payment from Cottage Health;
- A $3 Million Resolution Payment From A Tennessee Diagnostic Medical Imaging Services Company;
- A $100,000 Resolution Payment From An Indiana Medical Records Service Business Associate;
- A $85,000 Settlement PaymentFrom Bayfront Health St. Petersburg For Failing To Provide PHI Access;
- A $10,000 Settlement Payment From A Dental Practice For Wrongful Social Media Disclosures Of PHI; –
- A $2.15 Million Civil Money Penalty From Jackson Health System for Systemic HIPAA Violations
- A $3 Million Settlement Payment From University of Rochester Medical Center For Failing To Encrypt Laptops
- A $1.6 Million Civil Money Penalty From Texas Health and Human Services Commission For Long-Standing and Wide Reaching HIPAA Noncompliance;
- A $2.175 Settlement Payment From Sentara Hospitals For Violating The Breach Notification Rules; and
- A $85,000 Settlement Payment From Primary Care Provider Korunda Medical, LLC For Not Providing PHI Access
Second, the Resolution Agreement and various other smaller settlements during the year show HIPAA compliance and enforcement is a concern for smaller provideres and other covered entities, not juswt the huge ones. While the $65,000 settlement payment required by the Resolution Agreement is substantially smaller than the amounts of the civil monetary penalties and many of resolution payments OCR collected in its other 2019 enforcement actions, the West Georgia and other 2019 enforcement actions demonstrate the teeth behind the warning in the OCR Press Release announcing the West Georgia Resolution Agreement from OCR Director Roger Severino that“All providers, large and small, need to take their HIPAA obligations seriously.” With OCR promises to keep up its vigorous investigation and enforcement of the HIPAA requirements, every Covered Entity and business associate should take the necessary steps to verify and maintain their HIPAA compliance and to be prepared to defend their compliance under the Privacy, Security, Breach Notification and HIPAA access and other individual rights mandates of HIPAA.
Third, OCR’s statement in the Resolution Agreement about the failure by West Georgia to meaningfully act to correct compliance deficiencies and cooperate in other corrective action during the period following the breach report highlights the importance for covered entities involved in a breach or other dealings with OCR on a potential compliance concern to behave appropriately to express and exhibit the necessary concern OCR expects regarding the compliance issue to position themselves to request and receive the clemency OCR is empowered under HIPAA to extend when deciding the sanctions for any noncompliance.
Of course meeting the requirements of HIPAA is not the only concern that covered entities should consider as they review and tightened their HIPAA and other privacy and data security procedures. Health care providers and other covered entities also should keep in mind their other obligations to protect patient and other confidential information under other federal laws, the requirements of which also are ever-evolving. For instance, on January 1, 2020 Texas providers like other Texas businesses will become subject to a shortened deadline for providing notice of data breaches under a new law enacted by the Texas Legislature in its last session. Arrangements should be designed to fulfill all of these requirements as well as any ethical or contractual.
Covered entities also should keep in mind that violations of HIPAA can have implications well beyond HIPAA.ramifications beyond HIPAA itself. For instance, heath care providers can face disqualification from federal program participation, licensing and ethics discipline and other professional consequences. Health plans and their fiduciaries also may face Department of Labor and other fiduciary claims, while insurers can face licensing and other regulatory consequences. The Labor Department followed up on previous warnings that health plan fiduciaries duties include a fiduciary duty to protect health plan data by adding HIPAA compliance to certain health plan audits. Insurers, third of art administrators and others also can face duties and liabilities under state insurance and data privacy laws from regulator or private litigant actions.
For More Information
We hope this update is helpful. For more information about this or other labor and employment developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of health industry and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Scribe for the ABA JCEB Annual Agency Meeting with the Department of Health & Human Services Office of Civil Rights, Vice Chair of the ABA International Section Life Sciences Committee, past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group and the ABA RPTE Employee Benefits & Other Compensation Group, Ms. Stamer has extensive legal, operational, and public policy experience advising and representing health care, health care and other entities about HIPAA and other privacy, data security, confidentiality and other matters.
Ms. Stamer’s work throughout her 30 plus year career has focused heavily on working with health care and managed care, health and other employee benefit plan, insurance and financial services, public and private primary, secondary, and other educational institutions, and other public and private organizations and their technology, data, and other service providers and advisors domestically and internationally with legal and operational compliance and risk management, performance and workforce management, regulatory and public policy and other legal and operational concerns. As a part of this work, she has recurrently worked extensively with public school districts and public and private primary and secondary schools, colleges and universities, academic medical, and other educational institutions, insured and self-insured health plans; domestic and international hospitals, health care systems, clinics, skilled nursing, long term care, rehabilitation and other health care providers and facilities; medical staff, accreditation, peer review and quality committees and organizations; billing, utilization management, management services organizations, group purchasing organizations; pharmaceutical, pharmacy, and prescription benefit management and organizations; consultants; investors; EMR, claims, payroll and other technology, billing and reimbursement and other services and product vendors; products and solutions consultants and developers; investors; managed care organizations, employers; and federal and state legislative, regulatory, investigatory and enforcement bodies and agencies on health care, education, and other data privacy, security, use, protection and disclosure; disability and other educational rights; workforce, and a host of other risk management and compliance concerns.
Ms. Stamer is most widely recognized for her decades-long leading edge work, scholarship and thought leadership on health and other privacy and data security and other health industry legal, public policy and operational concerns. This involvement encompasses helping health care systems and organizations, group and individual health care providers, health plans and insurers, health IT, life sciences and other health industry clients prevent, investigate, manage and resolve sexual assault, abuse, harassment and other organizational, provider and employee misconduct and other performance and behavior; manage Section 1557, Civil Rights Act and other discrimination and accommodation, and other regulatory, contractual and other compliance; vendors and suppliers; contracting and other terms of participation, medical billing, reimbursement, claims administration and coordination, Medicare, Medicaid, CHIP, Medicare/Medicaid Advantage, ERISA and other payers and other provider-payer relations, contracting, compliance and enforcement; Form 990 and other nonprofit and tax-exemption; fundraising, investors, joint venture, and other business partners; quality and other performance measurement, management, discipline and reporting; physician and other workforce recruiting, performance management, peer review and other investigations and discipline, wage and hour, payroll, gain-sharing and other pay-for performance and other compensation, training, outsourcing and other human resources and workforce matters; board, medical staff and other governance; strategic planning, process and quality improvement; meaningful use, EMR, HIPAA and other technology, data security and breach and other health IT and data; STARK, ant kickback, insurance, and other fraud prevention, investigation, defense and enforcement; audits, investigations, and enforcement actions; trade secrets and other intellectual property; crisis preparedness and response; internal, government and third-party licensure, credentialing, accreditation, HCQIA and other peer review and quality reporting, audits, investigations, enforcement and defense; patient relations and care; internal controls and regulatory compliance; payer-provider, provider-provider, vendor, patient, governmental and community relations; facilities, practice, products and other sales, mergers, acquisitions and other business and commercial transactions; government procurement and contracting; grants; tax-exemption and not-for-profit; privacy and data security; training; risk and change management; regulatory affairs and public policy; process, product and service improvement, development and innovation, and other legal and operational compliance and risk management, government and regulatory affairs and operations concerns. to establish, administer and defend workforce and staffing, quality, and other compliance, risk management and operational practices, policies and actions; comply with requirements; investigate and respond to Board of Medicine, Health, Nursing, Pharmacy, Chiropractic, and other licensing agencies, Department of Aging & Disability, FDA, Drug Enforcement Agency, OCR Privacy and Civil Rights, Department of Labor, IRS, HHS, DOD, FTC, SEC, CDC and other public health, Department of Justice and state attorneys’ general and other federal and state agencies; JCHO and other accreditation and quality organizations; private litigation and other federal and state health care industry actions: regulatory and public policy advocacy; training and discipline; enforcement; and other strategic and operational concerns.
Author of leading works on HIPAA and a multitude of other health care, health plan and other health industry matters, the American Bar Association (ABA) International Section Life Sciences Committee Vice Chair, a Scribe for the ABA Joint Committee on Employee Benefits (JCEB) Annual OCR Agency Meeting and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her extensive publications and thought leadership as well as leadership involvement in a broad range of other professional and civic organizations. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- Omnicare & CVS Accused Of Health Care Fraud In Long Term Care Pharmacies
- $1.6M HIPAA Penalty Mostly Due To Inadequate Security Assessment & Oversight
- Former NFL Players Charged With Health Fraud Not Helped By Providers
- University of Rochester Medical Center Paying $3 Million For Unencrypted Laptop & Flash Drive
- Comment On New Interim Final Hemp Production Regs By 12/30
- Jackson Health System Nailed With $2.15 Million Plus Penalty For Violating HIPAA
- IRS Proposes Easing Disclosure Requirements For Certain Tax-Exempt Entities
- Important Lessons For Health Care Providers From Michigan State Settlement Of OCR Larry Nassar Sexual Abuse Investigation
- Air Ambulance Bills Drawing Congressional “Surprise Billing” Scrutiny
- Two Women Sentenced for Defrauding Federal Health Care Program of $26 Million Plus
- VA App Helps Providers Screen Vets For Environmental Exposures
- Health IT Provider Pays $100K To OCR For Breach After No HIPAA Risk Assessment
- New Pharma Transparency Rules Mean More Work For Providers
- Tips Help Exempt Organizations Avoid Common Form 990 Filing Mistakes
- Providers, Other HIPAA-Covered Entities Must Provide PHI to Patient-Designated Apps; Liable For Security On Covered Entity Supplied Or Sponsored Apps
- Provider Pays $3 Million For Breach With Delayed Investigation & Notice
- VA Offers Free Online Provider Training on Chronic Multisymptom Illness & Other Veteran Care Topics
- CMS Finalizes 2020 Medicare Advantage & Prescription Drug Program Rule Updates & Implements Other Integrity Rule Changes
- Beef Up Patient Education & Management Tools With Diabetes Alert Day Resources
- New GAO Report Likely To Fuel Scrutiny Of Air Ambulance Charges
- Tax Exemption Determination Procedures Changing
- Cognitive Disability Exclusion from Heart Transplant List Placement Prohibited
- FDA Announces Emergency Approval of In Vitro Diagnostic Device Ebola Detection in Congo
- Year-End $3 Million HIPAA Settlement Pushes 2018 OCR HIPAA Recoveries Over $28 Million; Act Promptly To Strengthen Compliance & Share Ideas For Simplification
- ONC Report Signals New Interoperability Demands Coming
- Watch FLSA Compliance When Scheduling or Paying Healthcare Workers Creatively
- Obamacare Future Unclear After Trial Court Holds Unconstitutional
- Allergy Practice $125,000 Settlement Reminds Health Care Providers, Other HIPAA Entities Of Press-Related HIPAA Risk
- DOJ-Atrium Settlement Signals Possible Antitrust Risks From Common Provider Contract Terms
- Record $16M HIPAA Sanction Shows Need For Current Enterprise Risk Assessment; ONC/OCR Share New Tool To Help HIPAA Covered Entities Comply
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The author and Solutions Law Press, Inc. disclaim, and have no responsibility to provide any update or otherwise notify anyone any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2019 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
DOJ Omnicare/CVS Suit Highlights Potential Pharmacy Benefit Claims Abuse Exposure For Health Plans, Member Safety Risk
December 18, 2019A civil health care fraud lawsuit filed by the Department of Justice (“DOJ”) in the U.S. District Court for the Southern District of New York today (December 17, 2019) against the nation’s largest long term care pharmacy provider, Omnicare, and its parent, CVS Healthcare Corporation may signal the advisability for insurers, fiduciaries, administrators and sponsors of insured and self-insured health and other benefit plans providing pharmacy benefits to tighten claims and audit past claims payments for prescription drug claims submitted by Omnicare and other CVS pharmacy providers as well as other pharmacy claims to the pharmacy possessed a valid, current prescription to dispense the drug.
Omnicare Complaint Highlights Potential Prescription Drug Fraud By Billing For Filling Expired Prescriptions
In its U.S. ex rel Bassan complaint in intervention (Omnicare and CVS) complaint DOJ joined by 29 states and the District of Colombia filed suit against Omnicare, and its parent company, CVS Healthcare Corporation for damages and civil penalties under the False Claims Act for fraudulently billing federal healthcare programs for hundreds of thousands of non-controlled prescription drugs that DOJ claims Omnicare illegally dispensed to elderly and disabled individuals in assisted living facilities, group homes, independent living communities, and other non-skilled residential long-term care facilities (“LTC facilities”) without a valid, current prescription.. The States of California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Illinois, Indiana, Iowa, Louisiana, Maryland, Massachusetts, Michigan, Minnesota, Montana, Nevada, New Jersey, New Mexico, New York, North Carolina, Oklahoma, Rhode Island, Tennessee, Texas, Vermont, Virginia, Washington, Wisconsin, and the District Of Columbia are joining the DOJ in the complaint as co-plaintiffs.
Omnicare is the country’s largest provider of pharmacy services to LTC facilities. It currently operates approximately 160 pharmacies in 47 states across the United States, which dispense tens of millions of prescription drugs to LTC facilities that serve elderly and disabled individuals. CVS acquired Omnicare in May 2015, and shortly thereafter assumed an active role in overseeing Omnicare’s operations, including pharmacy dispensing practices and systems.
The DOJ complaint in the Federal District Court in Manhattan, New York charges that Omnicare illegally dispensed and billed the federal government and patients for antipsychotics, anticonvulsants, and antidepressants Omnicare dispensed to elderly and disabled residents in LTC facilities without proper prescriptions. According to the DOJ complaint from 2010 until 2018, Omnicare and CVS allowed Omnicare pharmacies to dispense non-controlled prescription drugs to tens of thousands of elderly and disabled individuals living in LTC facilities based on prescriptions that had expired, were out of refills, or were otherwise invalid. Omnicare repeatedly disregarded prescription refill limitations and expiration dates that required doctor visits to reevaluate whether the drug should be renewed. Instead of requesting new prescriptions when old ones expired, Omnicare allowed prescriptions to “roll over.” At Omnicare, “rolling over” a prescription meant that when a prescription expired, Omnicare’s computer systems would assign the old prescription a new number and the pharmacy would continue to dispense the drug indefinitely without the need for a prescription renewal. Depending on the computer system used, DOJ claims Omnicare also sometimes assigned a fake number of authorized refills to a prescription – usually 99 allowable refills for Medicare patients – to allow for continuous refilling. DOJ claims that Omnicare pharmacies “rolled over” prescriptions for elderly and disabled individuals living in more than 3,000 residential long-term care facilities, including assisted living facilities operated by the largest long-term care providers in the country, such as Brookdale Senior Living, Atria Senior Living, Sunrise Senior Living Services, and Five Star Senior Living. DOJ charges that Omnicare used these practices to refill prescriptions for patients after the required prescription for refill expired for months, and sometimes years, after the prescriptions expired. The complaint alleged that Omnicare internally referred to these renumbered expired prescriptions as “rollover” prescriptions.
Many of the prescription drugs dispensed by Omnicare without valid prescriptions treat serious, chronic conditions, such as dementia, depression, and heart disease. They include antipsychotics, anticonvulsants, cardiovascular medications, anti-depressants, and other drugs that can have dangerous side effects and need to be closely monitored by doctors, particularly when taken in combination with other drugs by elderly patients.
DOJ says these Omnicare practices of illegally dispensing drugs to elderly and disabled individuals living in LTC facilities exposed these vulnerable individuals to a significant risk of harm. In contrast to traditional skilled nursing homes, where residents have access to 24-hour medical care supervised by doctors, assisted living and other non-skilled residential facilities offer more limited medical care, or none at all. In particular, these LTC facilities generally do not have doctors on staff to oversee and monitor residents’ drug therapy. By repeatedly dispensing potent drugs without current and valid prescriptions, Omnicare jeopardized the health and safety of tens of thousands of individuals who continued to take the same drugs for months, and sometimes years, without consulting their doctors to determine whether the medications were still clinically appropriate.
A large percentage of the long-term care residents served by Omnicare are beneficiaries of federal healthcare programs. The complaint charges that along with illegally filling the expired prescriptions, Omnicare knowingly transmitted false information to these federal healthcare programs that made it appear that drug dispensations were supported by current, valid prescriptions from physicians when in fact they were not. By dispensing drugs without valid prescriptions, Omnicare presented, or caused to be presented, hundreds of thousands of false claims to Medicare, Medicaid, and TRICARE that were ineligible for payment in violation of the False Claims Act. In fact, the complaint charges that Omnicare managers exerted pressure on overwhelmed pharmacy staff to fill prescriptions quickly so that Omnicare could submit claims and collect payments on these rollover claims.
Moreover, DOJ says that it possesses evidence that senior management at Omnicare and CVS knew of the practices. The DOJ complaint charges among other things that the Omnicare’s Compliance Department succinctly acknowledged the problem in an internal April 2015 email in which one Regional Compliance Officer stated: “An issue that I am running into more and more in multiple states concerns the ability of our systems to allow prescriptions to continue to roll after a year to a new prescription number without any documentation or pharmacist intervention.” A compliance officer then forwarded the email to the head of Omnicare’s Third Party Audit group, who responded that she had a “potential solution (programmed last year) but no one is rolling it out now.”
In today’s announcement of the lawsuit, Manhattan U.S. Attorney Geoffrey S. Berman said: “As alleged, Omnicare put at risk the health of tens of thousands of elderly and disabled individuals living in assisted living and other residential long-term care facilities by dispensing drugs for months, and sometimes years, without obtaining current, valid prescriptions from doctors. A pharmacy’s fundamental obligation is to ensure that drugs are dispensed only under the supervision of treating doctors who monitor patients’ drug therapies. Omnicare blatantly ignored this obligation in favor of pushing drugs out the door as quickly as possible to make more money. This Office will continue to hold accountable those who put at risk people’s health and safety just to turn a profit.”
Meanwhile, HHS-OIG Special Agent in Charge Scott J. Lampert said: “Failing to consult doctors as to whether prescriptions should be refilled places patients’ health and medical care at serious risk. These automatic rollover refills could have significant consequences for vulnerable people in long term-care facilities. We will continue working with law enforcement partners to protect people depending on these taxpayer-funded government health programs.”
Charges Suggest Potential Advisability For Plan Audit of Prescription Drug Charges To Confirm Supported By Valid Prescription For Dispensed Drugs
The charges made in the complaint filed against Omnicare highlight an area of claims payment eligibility not regularly verified by many pharmacy benefit and other health claims administrators when administering pharmacy benefit claims- the existence of a current valid prescription to support the dispensation of the billed prescription medication. Except for pain management and certain other medications flagged by regulators or benefit systems as subject to heightened abuse risks, many plan administrators regularly take for granted existence of a current, valid script for many common, frequently issued and renewed, low cost prescriptions issued within frequency and other guidelines based upon the assumption that legal and ethical obligations of pharmacists and pharmacies under licensing, Drug Enforcement Agency and other rules generally provides adequate deterrence against abuses like those the DOJ accuses Omnicare of engaging in its complaint. However, growing corporate or other nonprofessional ownership or management of pharmacies and their management coupled with very limited, virtually all complaint driven oversight of federal and state regulatory and ethical agencies is diminishing the frequency and effectiveness of such oversight. As evidenced by the Omnicare complaint, scrupulous pharmacies may leverage opportunities allowed by this limited oversight to dispense and bill for commonly renewed prescription medication without proper orders in a manner that potentially places patients at risk at the expense of plans and their participants, beneficiaries, sponsors and insurers. Plans, insurers, fiduciaries, plan sponsors and administrators concerned about these risks may want to use the Omnicare lawsuit announcement as an opportunity to educate plan members and their caregivers about the importance of monitoring prescriptions, their refills and claims for abuse; audit and encourage plan members and their caregivers of members with claims paid with respect to Omnicare and other pharmacy claims’ and take other steps to assess the adequacy and tighten as appropriate their existing pharmacy benefit review procedures for verification of the existence of a current, valid prescription to mitigate these exposures. These exposures are further heightened by the widespread practice of outsourcing of pharmacy claims to prescription benefit management or other speciality pharmacy claims providers in many health plan designs including vendoirsand service providers owned or managed by parents or related companies of the pharmacy filling and billing for the scripts.
Health plan fiduciaries, administrators and sponsors that discover potential deficiencies in the validity of a prescription or other elements of a received or previously paid prescription benefit or other claim are cautioned to review and follow the applicable ERISA and for insured plans, state insurance, Patient Protection and Affordable Care Act (“ACA”) and contractual claims and appeals timelines and processes. Failure to follow these requirements can undermine the enforceability of plan remedies as well as expose the plan, its insurer or fiduciary to administrative penalties and other liabilities. Additionally, violations of the ACA mandated procedures also in the case of employment based plans also could expose the sponsoring employer or ubnion to liability for self reporting, self-assessment and payment of penalties under Internal Revenue Code Section 6039D. Where relevant regulatory or contractual time periods for denial have already expired either because the claim already was paid or the analysis otherwise was not timely completed in time to meet the deadline, plans may need to rely upon filing health care fraud or other avenues of relief in lieu of attempting to retroactively deny and recoup the questioned amounts in order to avoid violating the ACA and other rules. Plan fiduciaries and administrators also may need to consider the applicability of offering review by an independent medical review organization to fulfill ACA or other similar mandatesfor medical judgement based determinations.
More Information
We hope this update is helpful. For more information about this or other labor and employment developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of health industry and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Scribe for the ABA JCEB Annual Agency Meeting with OCR, Vice Chair of the ABA International Section Life Sciences Committee, past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group and the ABA RPTE Employee Benefits & Other Compensation Group, Ms. Stamer’s work throughout her 30 plus year career has focused heavily on working with health care and managed care, health and other employee benefit plan, insurance and financial services and other public and private organizations and their technology, data, and other service providers and advisors domestically and internationally with legal and operational compliance and risk management, performance and workforce management, regulatory and public policy and other legal and operational concerns. As a part of this work, she has continuously and extensively worked with domestic and international hospitals, health care systems, clinics, skilled nursing, long term care, rehabilitation and other health care providers and facilities; medical staff, accreditation, peer review and quality committees and organizations; billing, utilization management, management services organizations, group purchasing organizations; pharmaceutical, pharmacy, and prescription benefit management and organizations; consultants; investors; EMR, claims, payroll and other technology, billing and reimbursement and other services and product vendors; products and solutions consultants and developers; investors; managed care organizations, self-insured health and other employee benefit plans, their sponsors, fiduciaries, administrators and service providers, insurers and other payers, health industry advocacy and other service providers and groups and other health and managed care industry clients as well as federal and state legislative, regulatory, investigatory and enforcement bodies and agencies.
Ms. Stamer is most widely recognized for her decades-long leading edge work, scholarship and thought leadership on health and other privacy and data security and other health industry legal, public policy and operational concerns. This involvement encompasses helping health care systems and organizations, group and individual health care providers, health plans and insurers, health IT, life sciences and other health industry clients prevent, investigate, manage and resolve sexual assault, abuse, harassment and other organizational, provider and employee misconduct and other performance and behavior; manage Section 1557, Civil Rights Act and other discrimination and accommodation, and other regulatory, contractual and other compliance; vendors and suppliers; contracting and other terms of participation, medical billing, reimbursement, claims administration and coordination, Medicare, Medicaid, CHIP, Medicare/Medicaid Advantage, ERISA and other payers and other provider-payer relations, contracting, compliance and enforcement; Form 990 and other nonprofit and tax-exemption; fundraising, investors, joint venture, and other business partners; quality and other performance measurement, management, discipline and reporting; physician and other workforce recruiting, performance management, peer review and other investigations and discipline, wage and hour, payroll, gain-sharing and other pay-for performance and other compensation, training, outsourcing and other human resources and workforce matters; board, medical staff and other governance; strategic planning, process and quality improvement; meaningful use, EMR, HIPAA and other technology, data security and breach and other health IT and data; STARK, ant kickback, insurance, and other fraud prevention, investigation, defense and enforcement; audits, investigations, and enforcement actions; trade secrets and other intellectual property; crisis preparedness and response; internal, government and third-party licensure, credentialing, accreditation, HCQIA and other peer review and quality reporting, audits, investigations, enforcement and defense; patient relations and care; internal controls and regulatory compliance; payer-provider, provider-provider, vendor, patient, governmental and community relations; facilities, practice, products and other sales, mergers, acquisitions and other business and commercial transactions; government procurement and contracting; grants; tax-exemption and not-for-profit; privacy and data security; training; risk and change management; regulatory affairs and public policy; process, product and service improvement, development and innovation, and other legal and operational compliance and risk management, government and regulatory affairs and operations concerns. to establish, administer and defend workforce and staffing, quality, and other compliance, risk management and operational practices, policies and actions; comply with requirements; investigate and respond to Board of Medicine, Health, Nursing, Pharmacy, Chiropractic, and other licensing agencies, Department of Aging & Disability, FDA, Drug Enforcement Agency, OCR Privacy and Civil Rights, Department of Labor, IRS, HHS, DOD, FTC, SEC, CDC and other public health, Department of Justice and state attorneys’ general and other federal and state agencies; JCHO and other accreditation and quality organizations; private litigation and other federal and state health care industry actions: regulatory and public policy advocacy; training and discipline; enforcement; and other strategic and operational concerns.
Author of leading works on HIPAA and a multitude of other health care, health plan and other health industry matters, the American Bar Association (ABA) International Section Life Sciences Committee Vice Chair, a Scribe for the ABA Joint Committee on Employee Benefits (JCEB) Annual OCR Agency Meeting and a former Council Representative, Past Chair of the ABA Managed Care & Insurance Interest Group, former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her extensive publications and thought leadership as well as leadership involvement in a broad range of other professional and civic organizations. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
- NLRB Restores Pre-Obama Era Union Dues Checkoff Rule
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- Comment on Interim Domestic Hemp Production Rules By 12/30n. L ok
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
- Salary Threshold Increases Require Employer Review Of Salaried Worker FLSA Exemption Qualification
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The author and Solutions Law Press, Inc. disclaim, and have no responsibility to provide any update or otherwise notify anyone any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2019 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
OSHA Seeks Small Business Volunteers For Tree Care Safety Panel
December 17, 2019On December 10, 2019, the Occupational Safety and Health Administration (OSHA) notified the Small Business Administration Office of Advocacy that it plans to convene a small business panel on a possible OSHA Tree Care Operations safety standard in early 2020. OSHA’s potential tree care standard could cover employees who perform tree care operations, such as pruning, maintaining, repairing, or removing trees, as well as establish safe work practices for such operations. Potentially regulated entities would include employers who engage in daily tree care operations, as well as companies, municipalities, and organizations that occasionally perform tree care and removal as part of their primary operations (e.g., residential and commercial construction and remodeling, landscaping, golf course maintenance, power and pipeline clearing, certain agricultural operations, etc.).
The Office of Advocacy is seeking small entity representatives from the potentially regulated sectors to assist the OSHA panel in its review of this possible regulation. Small entity representatives, or SERS, may include small businesses, small non-profits organizations, and small governmental jurisdictions.
Any small business employer who would be affected by this potential regulation, please contact Bruce Lundegren at (202) 205-6144 or Bruce.Lundegren@sba.gov.
For More Information
We hope this update is helpful. For more information about this or other labor and employment developments, please contact the author Cynthia Marcotte Stamer via e-mail or via telephone at (214) 452 -8297.
Solutions Law Press, Inc. invites you receive future updates by registering on our Solutions Law Press, Inc. Website and participating and contributing to the discussions in our Solutions Law Press, Inc. LinkedIn SLP Health Care Risk Management & Operations Group, HR & Benefits Update Compliance Group, and/or Coalition for Responsible Health Care Policy.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Law and Labor and Employment Law and Health Care; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of health industry and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Ms. Stamer’s work throughout her 30 plus year career has focused heavily on working with health care and managed care, health and other employee benefit plan, insurance and financial services and other public and private organizations and their technology, data, and other service providers and advisors domestically and internationally with legal and operational compliance and risk management, performance and workforce management, regulatory and public policy and other legal and operational concerns. As a part of this work, she has continuously and extensively worked with domestic and international employer and other management clients including hospitals, health care systems and other health care organizations, management services organizations, group purchasing organizations; creditors, debtors, bankruptcy trustees and other change organizations; consultants; investors; payroll and other technology and other services and product vendors; products and solutions consultants and developers; self-insured health and other employee benefit plans, their sponsors, fiduciaries, administrators and service providers, insurers and other insurance and risk management clients; as well as federal and state legislative, regulatory, investigatory and enforcement bodies and agencies.
Author of hundreds of highly regarded books, articles and other publications, Ms. Stamer also is widely recognized for her scholarship, coaching, legislative and regulatory advocacy, leadership and mentorship on labor and employment, employee benefits, health and safety, education, performance management, privacy and data security, leadership and governance, and other management concerns within the American Bar Association (ABA), the International Information Security Association, the Southwest Benefits Association, and a variety of other international, national and local professional, business and civic organizations. Examples of these involvements include her service as the ABA Intellectual Property Law Section Law Practice Management Committee; the ABA International Section Life Sciences and Health Committee Vice Chair-Policy; a Scribe for the ABA Joint Committee on Employee Benefits (JCEB) Annual OCR Agency Meeting and a former JCEB Council Representative and Marketing Chair; Past Chair of the ABA RPTE Employee Benefits and Other Compensation Group and Vice Chair of its Law Practice Management Committee; Past Chair of the ABA Managed Care & Insurance Interest Group; former Vice President and Executive Director of the North Texas Health Care Compliance Professionals Association, past Southwest Benefits Association Board member; past Texas Association of Business State Board Member, BACPAC Committee Meeting, Regional and Dallas Chapter Chair; past Dallas Bar Association Employee Benefits Committee Executive Committee; former SHRM Region IV Chair and National Consultants Forum Board Member; for WEB Network of Benefit Professionals National Board Member and Dallas Chapter Chair; former Dallas World Affairs Council Board Member; founding Board Member, past President and Patient Empowerment and Health Care Heroes founder for the Alliance for Health Care Excellence; former Gulf States TEGE Council Exempt Organizations Coordinator and Board member; past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, and involvement in a broad range of other professional and civic organizations. For more information about Ms. Stamer or her health industry and other experience and involvements, see www.cynthiastamer.com or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources available here such as:
- $1.6M HIPAA Penalty Largely Caused By Inadequate Security Assessments & Oversight
- 10 Former NFL Payers Charged With Defrauding NFL Retiree Health Fund
- NLRB Order Directs Settlement Of McDonald’s Unfair Labor Practice Complaints Including Joint Employer Liability Charges Against McDonald’s USA
- 2018 US National Health Expenditures Grew Again
- ONC Patient Matching for Prescription Drug Monitoring Program Slides Available
- SBA Hosts Employee Benefits Roundtable 11/21
- College Pays $54,000 To Settle DOJ ADA Lawsuit For Paramedic Program’s Termination of TA With MS
- Business Leaders Serve Jail Time For Employment Tax Crimes
- Comment on Interim Domestic Hemp Production Rules By 12/30n. L ok
- New $2.15M OCR Penalty Shows Health Plans Risks Of HIPAA Violations
- Proposed NLRB Employee Definition To Exclude College Study Workers
- DOL Proposing To Allow Default Website ERISA Retirement Plan Disclosures
- Salary Threshold Increases Require Employer Review Of Salaried Worker FLSA Exemption Qualification
- Chrisley and Other Criminal Tax Prosecut
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The author and Solutions Law Press, Inc. disclaim, and have no responsibility to provide any update or otherwise notify anyone any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2019 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.



 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer 

You must be logged in to post a comment.