March 19, 2019
Employers concerned about minimum wage, overtime and other liability from the Proposed Salary Threshold Rule (“Proposal”) that if adopted will increase the minimum salary for the Fair Labor Standards Act (“FLSA”) “white collar” overtime exemption from $23,660 annually to $35,308 annually. If adopted as proposed, the Proposal overnight will disqualify a million plus currently salaried workers to hourly employees that their employers will be required to pay minimum wage and overtime under the FLSA. Businesses concerned about the Proposal or other burdensome minimum wage or overtime requirements under the FLSA need to tell the Labor Department about these rules burdensome effects on business.
Proposal To Raise Minimum Salary For Overtime Exemption
The Labor Department Proposal if adopted will increase to $679 per week the minimum amount that an employer must pay an employee to treat that employee as exempt from the minimum wage or overtime rules of the FLSA regardless of the role or position of the employee. This means that an additional million plus employees overnight no longer would qualify to be paid as salaried rather than hourly employees. The Proposal
Under currently enforced FLSA rules, employers generally must treat any employee earning less than $455 per week ($23,660 annually) as a non-exempt employee. This generally means that the employer must pay the employee at least minimum wage for regular time and must pay overtime to the worker for any hours worked in excess of 40 hours per week.
The Labor Department set the minimum weekly earnings level of $455 per week in 2004. The Proposal if adopted will increase the minimum required earnings an employee must earn to qualify for exemption from minimum wage and overtime rules more than $124 per week to $679 per week (equivalent to $35,308 per year).
The Department also is asking for public comment on the Proposal’s language for periodic review to update the salary threshold. An update would continue to require notice-and-comment rule making rather than calling for automatic adjustments to the salary threshold for inflation.
Speak Up About Proposal & Other FLSA Burdens On Business
Businesses concerned about Proposal to increase the salary threshold or other burdensome FLSA rules or enforcement policies should seize the opportunity to provide feedback.
To start with, businesses should submit comments about the Proposed Rule electronically at www.regulations.gov as soon as possible before the 60-day comment period runs in mid-May.
Additionally, concerned businesses also should consider participating in events like the Small Business Roundtables that the Small Business Administration (“SBA”) Office of Advocacy plans to host to discuss the Proposal to hear directly from small businesses about the impact of the proposed rule. Currently SBA plans to host three roundtables:
- Thursday April 4, 2019 – 2:00 pm – 4:00 pm (EDT) at the University of South Florida Port Tampa Bay, Building 1101 Channelside Dr., Suite 210, Tampa, FL 33602;
- Thursday April 11, 2019 – 2:00 pm – 4:00 pm (EDT) at the SBA Headquarters, Eisenhower Room B 409 Third Street SW, Washington, DC 20416 (Call-in option available); and
- Tuesday April 30, 2019 – 9:00 am – 11:00 am (CDT) at the Mobile Area Chamber of Commerce 451 Government St., Mobile, Alabama 36602
Interested parties must RSVP to Janis.Reyes@sba.gov to participate. Note that while SBA reports that SBA has invited Labor Department staff, the Labor Department has not confirmed its acceptance of these invitations yet. Also, because comments expressed during these roundtables do not take the place of submitting written comments to the regulatory docket, concerned businesses should also still comment on the Proposal. However adverse feedback from business expressed at this meeting could help to motivate SBA to express opposition or other negative feedback on the Proposal.
Other Defensive Actions To Minimize FLSA Exposures
Whether or not the Proposal takes effect, all U.S. businesses will want to strengthen their existing practices for classifying and compensating workers under existing Federal and state wage and hour laws, tighten contracting and other compliance oversight in relation to outsourced services, weigh options to clean up exposure areas, review insurance coverages and consider other options to minimize their potential liability under applicable wages and hour laws. Conducting this analysis within the scope of attorney-client privilege is important because the analysis and discussions are highly sensitive both as potential evidence for wage and hour and other legal purposes. Consequently, businesses and their leaders generally will want to arrange for this work to be protected to the extent by attorney-client privilege, work product and other evidentiary protections against discovery by Department, employees or others for FLSA or other workforce enforcement actions.
As a part of this process, businesses and their leaders generally should plan to:
- Review subcontractor, temporary, lease employee, independent contractor and other outsourced labor and services relationship for potential risk of worker reclassification and tighten contracting and other procedures;
- Audit the position of each employee currently classified as exempt to assess its continued sustainability and to develop documentation justifying that characterization;
- Audit characterization of workers obtained from staffing, employee leasing, independent contractor and other arrangements and implement contractual and other oversight arrangements to minimize risks that these relationships could create if workers are recharacterized as employed by the employer receiving these services;
- Review the characterization of on-call and other time demands placed on employees to confirm that all compensable time is properly identified, tracked, documented, compensated and reported;
- If the employer hires any individuals under age 18, audit and implement appropriate procedures to ensure its ability to demonstrate compliance with all applicable FLSA child labor rules;
- If the employer is a government contractor or subcontractor or otherwise performs any services on projects funded with federal or state funds, evaluate the applicability and fulfillment of any special wage, fringe benefit, recordkeeping or other government contracting wage and hour requirements;
- If the employer hires foreign agricultural or other workers subject to special conditions and requirements, to review compliance with those special requirements;
- Review and tighten existing practices for tracking compensible hours and paying non-exempt employees for compliance with applicable regulations and to identify opportunities to minimize costs and liabilities arising out of the regulatory mandates;
- If the employer uses leased, temporary, or other outsourced labor, evaluate contractual, process and other options to support the employer’s ability cost effectively to respond to an audit, investigation or enforcement action by the Labor Department or private litigants and if necessary, obtain indemnification or other recovery in the event the employer incurs liability due to the use or practices of the outsourced labor supplier;
- If the audit raises questions about the appropriateness of the classification of an employee as exempt, self-initiation of proper corrective action after consultation with qualified legal counsel;
- Review and document all workers classified as exempt;
- Review of existing documentation and record keeping practices for hourly employees;
- Evaluate potential exposures under other employment, labor, tax or related laws or contracts that might be impacted by the findings or actions taken in response to those findings;
- Explore available options and alternatives for calculating required wage payments to non-exempt employees and assessing and resolving other concerns;
- Identify and calculate other employee benefit, tax or other corrections and associated costs and procedures that may be required as a result of findings or corrective actions resulting from their redress;
- Re-engineer work rules, policies, contracts and practices to minimize costs and liabilities as appropriate in light of the regulations and enforcement exposures;
- Explore insurance, indemnification and other options for mitigating risks and associated investigation and defense costs; and
- Consider self-correction within the new PAID Program or otherwise.
If you need more information or have questions, contact the author, Cynthia Marcotte Stamer.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
The author of the “Texas Payday Act,” and numerous other highly regarded publications on wage and hour and other human resources, employee benefits and compensation publications, Ms. Stamer is well-known for her 30 years of extensive wage and hour, compensation and other management advice and representation of restaurant and other hospitality, health, insurance, financial services, technology, energy, manufacturing, retail, governmental and other domestic and international businesses of all types and sizes.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here including:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2019 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on Give Labor Department Feedback On Proposed $124 Per Week Increase In FLSA Salary Threshold & Other Burdensome Rules |
Comments Off on Give Labor Department Feedback On Proposed $124 Per Week Increase In FLSA Salary Threshold & Other Burdensome Rules |  Attorney-Client Privilege, board of directors, Brokers, business travel, Child Labor, compensation, compliance, Construction, Corporate Compliance, corporate governance, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Policies, enforcement, Executive Compensation, Exempt, Fair Labor Standards Act, FLSA, HR, Human Resources, Insurance, Internal Controls, Internal Investigations, Labor Management Relations, Management, Managment, officers, Overtime, Telecommuting, Uncategorized, Union, Workforce | Tagged: Employer, FLSA, wage, Wage & Hour |
Attorney-Client Privilege, board of directors, Brokers, business travel, Child Labor, compensation, compliance, Construction, Corporate Compliance, corporate governance, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Policies, enforcement, Executive Compensation, Exempt, Fair Labor Standards Act, FLSA, HR, Human Resources, Insurance, Internal Controls, Internal Investigations, Labor Management Relations, Management, Managment, officers, Overtime, Telecommuting, Uncategorized, Union, Workforce | Tagged: Employer, FLSA, wage, Wage & Hour |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
March 15, 2019
Tax exempt organizations and tax exempt employee benefit plans take note. The Internal Revenue Service (IRS) exempt organization determination procedures are changing.
Revenue Procedure 2019-5 updates the Exempt Organization determination letters procedures. Changes include:
Adding references to “new” Form 1024-A, Application for Recognition of Exemption Under Section 501(c)(4) of the Internal Revenue Code
Clarifying that the IRS won’t rule on a request under IRC Section 501(c)(6) for an organization whose purpose relates to a controlled substance that is illegal under federal law
Increasing user fees for certain miscellaneous determinations from $1,000 to $2,000
Changing the name of the Office of Associate Chief Counsel, Tax Exempt and Government Entities, to the Office of Associate Chief Counsel, Employee Benefits, Exempt Organizations and Employment Taxes.
These changes will impact processes for submitting approval applications and other exempt organization, VEBA, fraternal benefit association and qualified employee plan dealings with the IRS. Impacted organizations, their leaders and advisors will want to adjust accordingly.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of management focused employment, employee benefit and insurance, workforce and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Highly valued for her rare ability to find pragmatic client-centric solutions by combining her detailed legal and operational knowledge and experience with her talent for creative problem-solving, Ms. Stamer’s clients include employers and other workforce management organizations; employer, union, association, government and other insured and self-insured health and other employee benefit plan sponsors, benefit plans, fiduciaries, administrators, and other plan vendors; domestic and international public and private health care, education and other community service and care organizations; managed care organizations; insurers, third-party administrative services organizations and other payer organizations; and other private and government organizations and their management leaders.
Throughout her 30 plus year career, Ms. Stamer has continuously worked with these and other management clients to design, implement, document, administer and defend hiring, performance management, compensation, promotion, demotion, discipline, reduction in force and other workforce, employee benefit, insurance and risk management, health and safety, and other programs, products and solutions, and practices; establish and administer compliance and risk management policies; comply with requirements, investigate and respond to government, accreditation and quality organizations, regulatory and contractual audits, private litigation and other federal and state reviews, investigations and enforcement actions; evaluate and influence legislative and regulatory reforms and other regulatory and public policy advocacy; prepare and present training and discipline; handle workforce and related change management associated with mergers, acquisitions, reductions in force, re-engineering, and other change management; and a host of other workforce related concerns. Ms. Stamer’s experience in these matters includes supporting these organizations and their leaders on both a real-time, “on demand” basis with crisis preparedness, intervention and response as well as consulting and representing clients on ongoing compliance and risk management; plan and program design; vendor and employee credentialing, selection, contracting, performance management and other dealings; strategic planning; policy, program, product and services development and innovation; mergers, acquisitions, bankruptcy and other crisis and change management; management, and other opportunities and challenges arising in the course of workforce and other operations management to improve performance while managing workforce, compensation and benefits and other legal and operational liability and performance.
Past Chair of the ABA Managed Care & Insurance Interest Group and, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, heavily involved in health benefit, health care, health, financial and other information technology, data and related process and systems development, policy and operations throughout her career, and scribe of the ABA JCEB annual Office of Civil Rights agency meeting, Ms. Stamer also is widely recognized for her extensive work and leadership on leading edge health care and benefit policy and operational issues. She regularly helps employer and other health benefit plan sponsors and vendors, health industry, insurers, health IT, life sciences and other health and insurance industry clients design, document and enforce plans, practices, policies, systems and solutions; manage regulatory, contractual and other legal and operational compliance; vendors and suppliers; deal with Medicare, Medicaid, CHIP, Medicare/Medicaid Advantage, ERISA, state insurance law and other private payer rules and requirements; contracting; licensing; terms of participation; medical billing, reimbursement, claims administration and coordination, and other provider-payer relations; reporting and disclosure, government investigations and enforcement, privacy and data security; and other compliance and enforcement; Form 990 and other nonprofit and tax-exemption; fundraising, investors, joint venture, and other business partners; quality and other performance measurement, management, discipline and reporting; physician and other workforce recruiting, performance management, peer review and other investigations and discipline, wage and hour, payroll, gain-sharing and other pay-for performance and other compensation, training, outsourcing and other human resources and workforce matters; board, medical staff and other governance; strategic planning, process and quality improvement; HIPAA administrative simplification, meaningful use, EMR, HIPAA and other technology, data security and breach and other health IT and data; STARK, antikickback, insurance, and other fraud prevention, investigation, defense and enforcement; audits, investigations, and enforcement actions; trade secrets and other intellectual property; crisis preparedness and response; internal, government and third-party licensure, credentialing, accreditation, HCQIA, HEDIS and other peer review and quality reporting, audits, investigations, enforcement and defense; patient relations and care; internal controls and regulatory compliance; payer-provider, provider-provider, vendor, patient, governmental and community relations; facilities, practice, products and other sales, mergers, acquisitions and other business and commercial transactions; government procurement and contracting; grants; tax-exemption and not-for-profit; 1557 and other Civil Rights; privacy and data security; training; risk and change management; regulatory affairs and public policy; process, product and service improvement, development and innovation, and other legal and operational compliance and risk management, government and regulatory affairs and operations concerns.
A former lead consultant to the Government of Bolivia on its Pension Privatization Project with extensive domestic and international public policy concerns in pensions, healthcare, workforce, immigration, tax, education and other areas, Ms. Stamer has been extensively involved in U.S. federal, state and local health care and other legislative and regulatory reform impacting these concerns throughout her career. Her public policy and regulatory affairs experience encompasses advising and representing domestic and multinational private sector health, insurance, employee benefit, employer, staffing and other outsourced service providers, and other clients in dealings with Congress, state legislatures, and federal, state and local regulators and government entities, as well as providing advice and input to U.S. and foreign government leaders on these and other policy concerns.
Author of leading works on a multitude of labor and employment, compensation and benefits, internal controls and compliance, and risk management matters and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other related concerns by her service in the leadership of the Solutions Law Press, Inc. Coalition for Responsible Health Policy, its PROJECT COPE: Coalition on Patient Empowerment, and a broad range of other professional and civic organizations including North Texas Healthcare Compliance Association, a founding Board Member and past President of the Alliance for Healthcare Excellence, past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children (now Warren Center For Children); current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee, current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Section, a current Defined Contribution Plan Committee Co-Chair, former Group Chair and Co-Chair of the ABA RPTE Section Employee Benefits Group, past Representative and chair of various committees of ABA Joint Committee on Employee Benefits; an ABA Health Law Coordinating Council representative, former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, a former member of the Board of Directors of the Southwest Benefits Association and others.
For more information about Ms. Stamer or her health industry and other experience and involvements, see here or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here such as the following:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advise or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2019 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication or the topic of this article, please contact the author directly. All other rights reserved.
 Comments Off on IRS Updates Plan Exemption & Exempt Organization Approval Procedures & Group Name |
Comments Off on IRS Updates Plan Exemption & Exempt Organization Approval Procedures & Group Name |  401(k), compensation, compliance, Corporate Compliance, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, Employee Benefits, Employer, Employers, Employment Tax, ESOP, Exempt, HR, Human Resources, MEWA, multiple employer plan (Meps), Patient Protection & Affordable Care Act, Plan Admistrator, Retirement Plans, Tax, tax exemption, Tax Qualification, third party administrators, Union |
401(k), compensation, compliance, Corporate Compliance, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, Employee Benefits, Employer, Employers, Employment Tax, ESOP, Exempt, HR, Human Resources, MEWA, multiple employer plan (Meps), Patient Protection & Affordable Care Act, Plan Admistrator, Retirement Plans, Tax, tax exemption, Tax Qualification, third party administrators, Union |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
March 14, 2019
Employee benefit plan sponsors, fiduciaries, administrators and advisors should review and update their benefit and compensation plan designs and testing in response to the just released tables of covered compensation under § 401(l)(5)(E) of the Internal Revenue Code and related regulations for the 2019 plan year in new Revenue Ruling 2019-06.
The new tables are available in the advance release copy of Revenue Ruling 2019-06, scheduled for official publication in Internal Revenue Bulletin 2019-14 on April 1, 2019.
The Revenue Ruling provides tables of covered compensation under § 401(l)(5)(E) of the Internal Revenue Code and related regulations for the 2019 plan year.
For this purpose, covered compensation is average of the contribution and benefit bases in effect under section 230 of the Social Security Act for each year in the 35 year period ending with the year in which an employee attains social security retirement age.
As the change will impact plan contribution limits, discrimination testing and other plan and contribution design and administration, employer and other plan sponsors, fiduciaries, administrators and service providers should evaluate the effects of the adjustments so as to maximize their ability to anticipate and respond to the adjustments.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of management focused employment, employee benefit and insurance, workforce and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Highly valued for her rare ability to find pragmatic client-centric solutions by combining her detailed legal and operational knowledge and experience with her talent for creative problem-solving, Ms. Stamer’s clients include employers and other workforce management organizations; employer, union, association, government and other insured and self-insured health and other employee benefit plan sponsors, benefit plans, fiduciaries, administrators, and other plan vendors; domestic and international public and private health care, education and other community service and care organizations; managed care organizations; insurers, third-party administrative services organizations and other payer organizations; and other private and government organizations and their management leaders.
Throughout her 30 plus year career, Ms. Stamer has continuously worked with these and other management clients to design, implement, document, administer and defend hiring, performance management, compensation, promotion, demotion, discipline, reduction in force and other workforce, employee benefit, insurance and risk management, health and safety, and other programs, products and solutions, and practices; establish and administer compliance and risk management policies; comply with requirements, investigate and respond to government, accreditation and quality organizations, regulatory and contractual audits, private litigation and other federal and state reviews, investigations and enforcement actions; evaluate and influence legislative and regulatory reforms and other regulatory and public policy advocacy; prepare and present training and discipline; handle workforce and related change management associated with mergers, acquisitions, reductions in force, re-engineering, and other change management; and a host of other workforce related concerns. Ms. Stamer’s experience in these matters includes supporting these organizations and their leaders on both a real-time, “on demand” basis with crisis preparedness, intervention and response as well as consulting and representing clients on ongoing compliance and risk management; plan and program design; vendor and employee credentialing, selection, contracting, performance management and other dealings; strategic planning; policy, program, product and services development and innovation; mergers, acquisitions, bankruptcy and other crisis and change management; management, and other opportunities and challenges arising in the course of workforce and other operations management to improve performance while managing workforce, compensation and benefits and other legal and operational liability and performance.
Past Chair of the ABA Managed Care & Insurance Interest Group and, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, heavily involved in health benefit, health care, health, financial and other information technology, data and related process and systems development, policy and operations throughout her career, and scribe of the ABA JCEB annual Office of Civil Rights agency meeting, Ms. Stamer also is widely recognized for her extensive work and leadership on leading edge health care and benefit policy and operational issues. She regularly helps employer and other health benefit plan sponsors and vendors, health industry, insurers, health IT, life sciences and other health and insurance industry clients design, document and enforce plans, practices, policies, systems and solutions; manage regulatory, contractual and other legal and operational compliance; vendors and suppliers; deal with Medicare, Medicaid, CHIP, Medicare/Medicaid Advantage, ERISA, state insurance law and other private payer rules and requirements; contracting; licensing; terms of participation; medical billing, reimbursement, claims administration and coordination, and other provider-payer relations; reporting and disclosure, government investigations and enforcement, privacy and data security; and other compliance and enforcement; Form 990 and other nonprofit and tax-exemption; fundraising, investors, joint venture, and other business partners; quality and other performance measurement, management, discipline and reporting; physician and other workforce recruiting, performance management, peer review and other investigations and discipline, wage and hour, payroll, gain-sharing and other pay-for performance and other compensation, training, outsourcing and other human resources and workforce matters; board, medical staff and other governance; strategic planning, process and quality improvement; HIPAA administrative simplification, meaningful use, EMR, HIPAA and other technology, data security and breach and other health IT and data; STARK, antikickback, insurance, and other fraud prevention, investigation, defense and enforcement; audits, investigations, and enforcement actions; trade secrets and other intellectual property; crisis preparedness and response; internal, government and third-party licensure, credentialing, accreditation, HCQIA, HEDIS and other peer review and quality reporting, audits, investigations, enforcement and defense; patient relations and care; internal controls and regulatory compliance; payer-provider, provider-provider, vendor, patient, governmental and community relations; facilities, practice, products and other sales, mergers, acquisitions and other business and commercial transactions; government procurement and contracting; grants; tax-exemption and not-for-profit; 1557 and other Civil Rights; privacy and data security; training; risk and change management; regulatory affairs and public policy; process, product and service improvement, development and innovation, and other legal and operational compliance and risk management, government and regulatory affairs and operations concerns.
A former lead consultant to the Government of Bolivia on its Pension Privatization Project with extensive domestic and international public policy concerns in pensions, healthcare, workforce, immigration, tax, education and other areas, Ms. Stamer has been extensively involved in U.S. federal, state and local health care and other legislative and regulatory reform impacting these concerns throughout her career. Her public policy and regulatory affairs experience encompasses advising and representing domestic and multinational private sector health, insurance, employee benefit, employer, staffing and other outsourced service providers, and other clients in dealings with Congress, state legislatures, and federal, state and local regulators and government entities, as well as providing advice and input to U.S. and foreign government leaders on these and other policy concerns.
Author of leading works on a multitude of labor and employment, compensation and benefits, internal controls and compliance, and risk management matters and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other related concerns by her service in the leadership of the Solutions Law Press, Inc. Coalition for Responsible Health Policy, its PROJECT COPE: Coalition on Patient Empowerment, and a broad range of other professional and civic organizations including North Texas Healthcare Compliance Association, a founding Board Member and past President of the Alliance for Healthcare Excellence, past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children (now Warren Center For Children); current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee, current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Section, a current Defined Contribution Plan Committee Co-Chair, former Group Chair and Co-Chair of the ABA RPTE Section Employee Benefits Group, past Representative and chair of various committees of ABA Joint Committee on Employee Benefits; an ABA Health Law Coordinating Council representative, former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, a former member of the Board of Directors of the Southwest Benefits Association and others.
For more information about Ms. Stamer or her health industry and other experience and involvements, see here or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here such as the following:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advise or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2019 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication or the topic of this article, please contact the author directly. All other rights reserved.
 Comments Off on IRS Updates 2019 Compensation Table |
Comments Off on IRS Updates 2019 Compensation Table |  105(h), 401(k), 4980H, ACA, board of directors, Brokers, church plan, compensation, compliance, Corporate Compliance, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, directors, Employee Benefits, Employer, Employers, Employment, Employment Policies, Employment Tax, ESOP, FICA, Health Benefits, health insurance, Health Plans, HR, Human Resources, Internal Revenue Code, IRC, multiple employer plan (Meps), pension plan, retirement plan, Retirement Plans, Retirements, Tax Qualification, Uncategorized |
105(h), 401(k), 4980H, ACA, board of directors, Brokers, church plan, compensation, compliance, Corporate Compliance, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, directors, Employee Benefits, Employer, Employers, Employment, Employment Policies, Employment Tax, ESOP, FICA, Health Benefits, health insurance, Health Plans, HR, Human Resources, Internal Revenue Code, IRC, multiple employer plan (Meps), pension plan, retirement plan, Retirement Plans, Retirements, Tax Qualification, Uncategorized |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
March 7, 2019
Employers concerned about managing their overtime liability should review and provide prompt feedback to the U.S. Department of Labor (Department) on a Notice of Proposed Rulemaking (NPRM) that would make an additional million plus American workers eligible for overtime under the Fair Labor Standards Act (“FLSA”) by increasing the minimum amount an employee must earn to be eligible for treatment as FLSA exempt to $679 per week.
Under currently enforced FLSA rules, employers generally must treat any employee earning less than $455 per week ($23,660 annually) as a non-exempt employee. This generally means that the employer must pay the employee at least minimum wage for regular time and must pay overtime to the worker for any hours worked in excess of 40 hours per week.
The minimum weekly earnings level of $455 per week was set in 2004. The proposed regulation would increase the salary threshold using current wage data projected to January 1, 2020 from $455 to $679 per week (equivalent to $35,308 per year).
The Department also is asking for public comment on the NPRM’s language for periodic review to update the salary threshold. An update would continue to require notice-and-comment rulemaking.
The NPRM maintains overtime protections for police officers, fire fighters, paramedics, nurses, and laborers including: non-management production-line employees and non-management employees in maintenance, construction and similar occupations such as carpenters, electricians, mechanics, plumbers, iron workers, craftsmen, operating engineers, longshoremen, and construction workers. The proposal does not call for automatic adjustments to the salary threshold.
The proposal to change the salary threshold in the NPRM follows a prior attempt by the Department of raise the threshold in 2016. The U.S. District Court for the Eastern District of Texas enjoined a 2016 final regulation that would have raised the threshold on November 22, 2016. Since November 6, 2017, the U.S. Court of Appeals for the Fifth Circuit has held in abeyance the Department’s appeal of the District Court’s ruling pending further rulemaking by the Department. In the 15 years since the District Court enjoined its 2016 final rule, the Department consistently has enforced the 2004 salary threshold level.
Employers concerned about the proposed increase in the salary threshold or other elements of the NPRM should submit comments about the proposed rule electronically at www.regulations.gov within the 60 day period following publication, in the rulemaking docket RIN 1235-AA20.
The NPRM proposing to increase the salary threshold for qualification as a FLSA-exempt employee is only one of a number of proposed rule changes that could significantly impact employer liabilities and costs.
Coupled with the Department’s continuing aggressive attacks against contract labor and other worker misclassification as well as other minimum wage, overtime and other FLSA rules, all employers should shore up the defensibility of their existing practices for classifying and compensating workers under existing Federal and state wage and hour laws, tighten contracting and other compliance oversight in relation to outsourced services, weigh options to clean up exposure areas, review insurance coverages and consider other options to minimize their potential liability under applicable wages and hour laws. Conducting this analysis within the scope of attorney-client privilege is important because the analysis and discussions are highly sensitive both as potential evidence for wage and hour and other legal purposes. Consequently, businesses and their leaders generally will want to arrange for this work to be protected to the extent by attorney-client privilege, work product and other evidentiary protections against discovery by Department, employees or others for FLSA or other workforce enforcement actions.
As a part of this process, businesses and their leaders generally should plan to:
- Review subcontractor, temporary, lease employee, independent contractor and other outsourced labor and services relationship for potential risk of worker reclassification and tighten contracting and other procedures;
- Audit the position of each employee currently classified as exempt to assess its continued sustainability and to develop documentation justifying that characterization;
- Audit characterization of workers obtained from staffing, employee leasing, independent contractor and other arrangements and implement contractual and other oversight arrangements to minimize risks that these relationships could create if workers are recharacterized as employed by the employer receiving these services;
- Review the characterization of on-call and other time demands placed on employees to confirm that all compensable time is properly identified, tracked, documented, compensated and reported;
- If the employer hires any individuals under age 18, audit and implement appropriate procedures to ensure its ability to demonstrate compliance with all applicable FLSA child labor rules;
- If the employer is a government contractor or subcontractor or otherwise performs any services on projects funded with federal or state funds, evaluate the applicability and fulfillment of any special wage, fringe benefit, recordkeeping or other government contracting wage and hour requirements;
- If the employer hires foreign agricultural or other workers subject to special conditions and requirements, to review compliance with those special requirements;
- Review and tighten existing practices for tracking compensable hours and paying non-exempt employees for compliance with applicable regulations and to identify opportunities to minimize costs and liabilities arising out of the regulatory mandates;
- If the employer uses leased, temporary, or other outsourced labor, evaluate contractual, process and other options to support the employer’s ability cost effectively to respond to an audit, investigation or enforcement action by WHD or private litigants and if necessary, obtain indemnification or other recovery in the event the employer incurs liability due to the use or practices of the outsourced labor supplier;
- If the audit raises questions about the appropriateness of the classification of an employee as exempt, self-initiation of proper corrective action after consultation with qualified legal counsel;
- Review and document all workers classified as exempt;
- Review of existing documentation and record keeping practices for hourly employees;
- Evaluate potential exposures under other employment, labor, tax or related laws or contracts that might be impacted by the findings or actions taken in response to those findings;
- Explore available options and alternatives for calculating required wage payments to non-exempt employees and assessing and resolving other concerns;
- Identify and calculate other employee benefit, tax or other corrections and associated costs and procedures that may be required as a result of findings or corrective actions resulting from their redress;
- Re-engineer work rules, policies, contracts and practices to minimize costs and liabilities as appropriate in light of the regulations and enforcement exposures;
- Explore insurance, indemnification and other options for mitigating risks and associated investigation and defense costs; and
- Consider self-correction within the new PAID Program or otherwise.
If you need more information or have questions, contact the author, Cynthia Marcotte Stamer.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
The author of the “Texas Payday Act,” and numerous other highly regarded publications on wage and hour and other human resources, employee benefits and compensation publications, Ms. Stamer is well-known for her 30 years of extensive wage and hour, compensation and other management advice and representation of restaurant and other hospitality, health, insurance, financial services, technology, energy, manufacturing, retail, governmental and other domestic and international businesses of all types and sizes.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here including:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2019 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on Labor Department Proposes Increasing FLSA Salary Threshold To $679 Per Week |
Comments Off on Labor Department Proposes Increasing FLSA Salary Threshold To $679 Per Week |  Attorney-Client Privilege, board of directors, Brokers, business travel, Child Labor, compensation, compliance, Construction, Corporate Compliance, corporate governance, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Policies, enforcement, Executive Compensation, Exempt, Fair Labor Standards Act, FLSA, HR, Human Resources, Insurance, Internal Controls, Internal Investigations, Labor Management Relations, Management, Managment, officers, Overtime, Telecommuting, Uncategorized, Union, Workforce | Tagged: Employer, FLSA, wage, Wage & Hour |
Attorney-Client Privilege, board of directors, Brokers, business travel, Child Labor, compensation, compliance, Construction, Corporate Compliance, corporate governance, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Policies, enforcement, Executive Compensation, Exempt, Fair Labor Standards Act, FLSA, HR, Human Resources, Insurance, Internal Controls, Internal Investigations, Labor Management Relations, Management, Managment, officers, Overtime, Telecommuting, Uncategorized, Union, Workforce | Tagged: Employer, FLSA, wage, Wage & Hour |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
February 7, 2019
Health plans and their employer and other sponsors, fiduciaries, administrators and other service providers, as well as health care providers, health care clearinghouses and their business associates (“Covered Entities”) should reconfirm the adequacy of their Health Insurance Portability and Accountability Act (“HIPAA”) compliance and risk management in light the U.S Department of Health and Human Services Office of Civil Rights (“OCR”) February 7, 2019 announcement that its 2018 year-end $3 Million Resolution Agreement with California-based Cottage Health increased OCR’s already record-setting enforcement recoveries in 2018 to nearly $28.7 million in a year already distinguished by OCR’s collection of a record-setting $16 million resolution payment against health insurance giant Anthem. Along with acting to ensure their own organization’s ability to defend their HIPAA compliance, Covered Entities and their leaders also should take advantage of the opportunity to provide input to OCR on opportunities for simplifying and improving OCR’s HIPAA regulations and enforcement by submitting relevant comments by February 12, 2019 to a Request for Information published by OCR in December that invites suggestions for simplifying or making other improvements to OCR’s current HIPAA guidance as well as monitoring and responding to other new and proposed regulatory developments.
2018 Cottage Health Resolution Agreement
According to OCR’s February 7, 2019 announcement, Cottage Health agreed in OCR’s final settlement of 2017 to pay OCR $3 million and to adopt a substantial corrective action plan to settle charges of HIPAA violations resulting from OCR’s investigations into two HIPAA Breach notifications Cottage Health filed regarding breaches of unsecured electronic protected health information (ePHI) affecting over 62,500 individuals.
- A December 2, 2013 breach notification that the removal of electronic security protections by a Cottage Health contractor rendered ePHI such as patient names, addresses, dates of birth, diagnoses/conditions, lab results and other treatment information of 33,349 individuals on a Cottage Health server accessible for download without a username or password from the internet to anyone outside Cottage Health. In an update to its original report filed on July 2, 2014, Cottage Health increased the number of individuals affected by this breach to 50,917. OCR’s investigation determined that security configuration settings of the Windows operating system permitted access to files containing ePHI without requiring a username and password. As a result, patient names, addresses, dates of birth, diagnoses, conditions, lab results and other treatment information were available to anyone with access to Cottage Health’s server.
- A December 1, 2015, that the misconfiguration of a server following an IT response to a troubleshooting ticket, exposed unsecured ePHI including patient names, addresses, dates of birth, social security numbers, diagnoses, conditions, and other treatment information of 11,608 individuals over the internet.
Based upon its investigation into the two breach reports, OCR concluded Cottage Health violated HIPAA by failing to conduct an accurate and thorough assessment of the potential risks and vulnerabilities to the confidentiality, integrity, and availability of the ePHI; failed to implement security measures sufficient to reduce risks and vulnerabilities to a reasonable and appropriate level; failed to perform periodic technical and non-technical evaluations in response to environmental or operational changes affecting the security of ePHI; and failed to obtain a written business associate agreement with a contractor that maintained ePHI on its behalf.
To resolve its exposure to potentially must greater civil monetary sanctions that OCR might seek for such potential violations under HIPAA’s civil monetary sanction rules, Cottage Health entered into December, 2018 Resolution Agreement to pay the $3 million settlement and undertake what OCR characterizes as “a robust corrective action plan to comply with the HIPAA Rules.” Among other things, the corrective action plan requires Cottage Health to:
- Conduct an enterprise-wide risk analysis of the potential risks and vulnerabilities to the confidentiality, integrity, and availability of ePHI held by Cottage Health (“Risk Analysis”) that OCR views as satisfactory to meet the requirements of 45 CFR 164.308(a)(1)(ii)(A);
- Develop and implement a risk management plan to address and mitigate any security risks and vulnerabilities identified in the Risk Analysis acceptable to OCR;
- Implement a process for regularly evaluating environmental and operational changes that affect the security of Cottage Health’s ePHI;
- Develop, maintain, and revise, as necessary, written policies and procedures to comply with the Federal standards that govern the privacy and security of individually identifiable health information under 45 C.F.R. Part 160 and Subparts A, C, and E of Part 164 (the “Privacy Rule” and “Security Rule”).
- Distribute to and conduct training on the HIPAA policies and procedures from all existing and new members of the Cottage Health workforce with access to PHI. Additionally, Cottage Health require all workforce members that have access to PHI to certify their receipt of, understanding and commitment to comply with the HIPAA Policies before allowing access to PHI and must deny access to PHI to any workforce member that has not provided the required certification.
- Submit to ongoing notification and reporting requirements to keep OCR informed about its compliance efforts.
2018 Record Setting HIPAA Enforcement Year
The final Resolution Agreement negotiated by OCR in 2018, the $3 million Cottage Health Resolution Agreement signed on December 11, 2018 added to an already record-setting year of HIPAA enforcement recoveries by OCR. In addition to recovering the single largest individual HIPAA settlement in history of $16 million with Anthem, Inc. OCR’s recovery of the following HIPAA settlements and fines totaling nearly $28.7 million surpassed its previous 2016 record of $23.5 million by 22 percent.
| Date |
Name |
Amount
|
| Jan. 2018 |
Filefax, Inc (settlement) |
$ 100,000 |
| Jan. 2018 |
Fresenius Medical Care North America (settlement) |
$ 3,500,000 |
| June 2018 |
MD Anderson (judgment) |
$ 4,348,000 |
| Aug. 2018 |
Boston Medical Center (settlement) |
$ 100,000 |
| Sep. 2018 |
Brigham and Women’s Hospital (settlement) |
$ 384,000 |
| Sep. 2018 |
Massachusetts General Hospital (settlement) |
$ 515,000 |
| Sep. 2018 |
Advanced Care Hospitalists (settlement) |
$ 500,000 |
| Oct. 2018 |
Allergy Associates of Hartford (settlement) |
$ 125,000 |
| Oct. 2018 |
Anthem, Inc (settlement) |
$ 16,000,000 |
| Nov. 2018 |
Pagosa Springs (settlement) |
$ 111,400 |
| Dec. 2018 |
Cottage Health (settlement) |
$ 3,000,000 |
| Total (settlements and judgment) |
$ 28,683,400 |
Aside from the previously discussed Cottage Health Resolution Agreement OCR announced on February 7, 2019, these OCR 2018 enforcement recoveries included:
- FileFax Resolution Agreement. In January 2018, OCR settled for $100,000 with Filefax, Inc., a medical records maintenance, storage, and delivery services provider. OCR’s investigation found that Filefax impermissibly disclosed protected health information (PHI) by leaving the PHI in an unlocked truck in the Filefax parking lot, or by granting permission to an unauthorized person to remove the PHI from Filefax, and leaving the PHI unsecured outside the Filefax facility.
- Fresenius Medical Care North America Resolution Agreement. In January 2018, OCR also settled for $3.5 million with Fresenius Medical Care North America (FMCNA), a provider of products and services for people with chronic kidney failure. FMCNA filed five breach reports for separate incidents occurring between February 23, 2012 and July 18, 2012, implicating the electronic protected health information (ePHI) of five FMCNA owned covered entities. OCR’s investigation revealed that FMCNA failed to conduct an accurate and thorough risk analysis of potential risks and vulnerabilities to the confidentiality, integrity, and availability of all of its ePHI. Additional potential violations included failure to implement policies and procedures and failure to implement a mechanism to encrypt and decrypt ePHI, when it was reasonable and appropriate to do so under the circumstances.
- MD Anderson ALJ Ruling. In June 2018, an HHS Administrative Law Judge ruled in favor of OCR and required The University of Texas MD Anderson Cancer Center (MD Anderson), a Texas cancer center, to pay $4.3 million in civil money penalties for HIPAA violations. OCR investigated MD Anderson following three separate data breach reports in 2012 and 2013 involving the theft of an unencrypted laptop from the residence of an MD Anderson employee and the loss of two unencrypted universal serial bus (USB) thumb drives containing the unencrypted ePHI of over 33,500 individuals. OCR’s investigation found that MD Anderson had written encryption policies going back to 2006 and that MD Anderson’s own risk analyses had found that the lack of device-level encryption posed a high risk to the security of ePHI. Despite the encryption policies and high risk findings, MD Anderson did not begin to adopt an enterprise-wide solution to encrypt ePHI until 2011, and even then it failed to encrypt its inventory of electronic devices containing ePHI between March 24, 2011 and January 25, 2013. This matter is under appeal with the HHS Departmental Appeals Board.
- MMC/BWH/MGH Resolution Agreements. In September 2018, OCR announced that it has reached separate settlements totaling $999,000, with Boston Medical Center (BMC), Brigham and Women’s Hospital (BWH), and Massachusetts General Hospital (MGH) for compromising the privacy of patients’ PHI by inviting film crews on premises to film an ABC television network documentary series, without first obtaining authorization from patients.
- ACH Resolution Agreement. In September 2018, OCR also settled with Advanced Care Hospitalists (ACH), a contractor physician group, for $500,000. ACH filed a breach report confirming that ACH patient information was viewable on a medical billing services’ website. OCR’s investigation revealed that ACH never had a business associate agreement with the individual providing medical billing services to ACH, and failed to adopt any policy requiring business associate agreements until April 2014. Although ACH had been in operation since 2005, it had not conducted a risk analysis or implemented security measures or any other written HIPAA policies or procedures before 2014.
- Allergy Associates Resolution Agreement. In October 2018, OCR settled with Allergy Associates, a health care practice that specializes in treating individuals with allergies, for $125,000. In February 2015, a patient of Allergy Associates contacted a local television station to speak about a dispute that had occurred between the patient and an Allergy Associates’ doctor. OCR’s investigation found that the reporter subsequently contacted the doctor for comment and the doctor impermissibly disclosed the patient’s PHI to the reporter.
- Anthem Resolution Agreement. In October 2018, Anthem, Inc. also paid $16 million to OCR and agreed to take substantial corrective action to settle potential violations of the HIPAA Rules after a series of cyberattacks led to the largest U.S. health data breach in history. Anthem filed a breach report after discovering cyber-attackers had gained access to their IT system via an undetected continuous and targeted cyberattack for the apparent purpose of extracting data, otherwise known as an advanced persistent threat attack. After filing their breach report, Anthem discovered cyber-attackers had infiltrated their system through spear phishing emails sent to an Anthem subsidiary after at least one employee responded to the malicious email and opened the door to further attacks. OCR’s investigation revealed that between December 2, 2014 and January 27, 2015, the cyber-attackers stole the ePHI of almost 79 million individuals, including names, social security numbers, medical identification numbers, addresses, dates of birth, email addresses, and employment information.
- Pegosa Springs Medical Center. In November 2018, Pagosa Springs Medical Center (PSMC), a critical access hospital, paid $111,400 to OCR to resolve potential violations concerning a former PSMC employee that continued to have remote access to PSMC’s web-based scheduling calendar, which contained patients’ ePHI, after separation of employment. OCR’s investigation revealed that PSMC impermissibly disclosed the ePHI of 557 individuals to its former employee and to the web-based scheduling calendar vendor without a business associate agreement in place.
These 2018 Resolution Agreements reaffirm the growing risks that Covered Entities and their business associates run by failing to take adequate steps to prevent and respond to breaches of ePHI and otherwise to maintain their compliance with HIPAA. Covered entities and business associates and their leaders should recognize and respond to these growing risks by reevaluating and strengthening their HIPAA compliance and risk management efforts to minimize the likelihood of violations and enhance their ability to mitigate potential liability that can result from breaches of HIPAA by responding efficiently and effectively.
Other Regulatory & Enforcement Developments
In addition to reaffirming their ongoing compliance with the longstanding requirements of HIPAA and other related federal and state laws, Covered Entities also should use care to carefully monitor and respond to new regulatory and other developments that might create new responsibilities or new opportunities to simplify their HIPAA compliance. In this respect, Covered Entities should take note of the 2018 and ongoing efforts by OCR to develop and publish new rules and other guidance intended to help health care providers and other Covered Entities, patients and caregivers and others understand their rights and responsibilities when dealing with protected health information in relation to patients afflicted with substance abuse and mental illness. Undertaken as part of the Trump Administration’s broader effort to combat opiate and other substance abuse within the United States, OCR in October published a package of guidance on How HIPAA Allows Doctors To Respond To The Opioid Crisis. Covered Entities and others concerned with the management of patients afflicted with substance abuse and mental illness should evaluate this guidance to understand and tailor their practices to respond to OCR’s perspectives of how HIPAA impacts the use, access and disclosure of protected health information as part of these efforts.
Covered Entities and others concerned about HIPAA compliance and interpretation also should carefully monitor and provide appropriate and timely input on developing HIPAA guidance that could impact their operations. In this regard, Covered Entities with ideas about opportunities for improving existing HIPAA guidance are encouraged to submit comments to OCR by February 12, 2019 in response to its Request for Information on improving care coordination and reducing the regulatory burdens of the HIPAA Rules published on December 12, 2018. In that RFI, OCR invites input from the public on how the HIPAA Privacy Rule, could be modified to:
- Encourage information-sharing for treatment and care coordination;
- Facilitate parental involvement in care;
- Address the opioid crisis and serious mental illness;
- Account for disclosures of PHI for treatment, payment, and health care operations as required by the HITECH Act;
- Change the current requirement for certain providers to make a good faith effort to obtain an acknowledgment of receipt of the Notice of Privacy Practices; and/or
- Otherwise simplify or improve the existing HIPAA rules.
As a part of these efforts, Covered Entities and other concerned parties also should anticipate that OCR will be focusing heavily in the upcoming year on the potential HIPAA privacy and security implications of efforts by its sister agency, the Office of the National Coordinator for Health Information Technology (“ONC”), to promote greater interoperability of electronic medical records discussed in ONC’s recent 2018 Report to Congress: Annual Update on the Adoption of a Nationwide System for the Electronic Use and Exchange of Health Information (“Report”).
Under the 21st Century Cures Act, Congress gave ONC authority to enhance innovation, scientific discovery, and expand the access and use of health information through provisions related to:
- The development and use of upgraded health IT capabilities;
- Transparent expectations for data sharing, including through open application programming interfaces (APIs); and
- Improvement of the health IT end-user experience, including by reducing administrative burden.
These priorities seek to increase nationwide interoperability of health information and reduce clinician burden. The Report says increases in the adoption of health IT means most Americans receiving health care services now have their health data recorded electronically. However, this information is not always accessible across systems and by all end users—such as patients, health care providers, and payers—in the market in productive ways. While the Report states ONC intends to move forward to promote efforts to help ensure that electronic health information can be shared safely and securely where appropriate to improve the health and care of all Americans, these activities inherently will raise many HIPAA concerns and challenges. Covered Entities and others concerned with these activities will want to carefully monitor the concurrent activities of OCR and ONC as these efforts progress, both to help tailor their planning and compliance efforts to respond to the anticipated demand for greater interoperability as required by ONC and to help shape these rules by providing timely input as appropriate in response to these developments.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of managed care and other health industry, health and other benefit and insurance, workforce and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Past Chair of the ABA Managed Care & Insurance Interest Group and, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer has been continuously involved the design, regulation, administration and defense of managed care and other health and employee benefit, health care, human resources and other staffing and workforce arrangements, contracts, systems, and processes. As a continuous component of this work, Ms. Stamer has worked closely with these and other clients on the design, development, administration, defense, and breach and data recovery of health care, workforce, insurance and financial services, trade secret and other information technology, data and related process and systems development, policy and operations throughout her career.
Scribe of the ABA JCEB annual Office of Civil Rights agency meeting, Ms. Stamer also is widely recognized for her extensive work and leadership on leading edge health care and benefit policy and operational issues.
Ms. Stamer’s clients include employers and other workforce management organizations; employer, union, association, government and other insured and self-insured health and other employee benefit plan sponsors, benefit plans, fiduciaries, administrators, and other plan vendors; managed care organizations, insurers, self-insured health plans and other payers and their management; public and private, domestic and international hospitals, health care systems, clinics, skilled nursing, long-term care, rehabilitation and other health care providers and facilities; medical staff, health care accreditation, peer review and quality committees and organizations; managed care organizations, insurers, third-party administrative services organizations and other payer organizations; billing, utilization management, management services organizations; group purchasing organizations; pharmaceutical, pharmacy, and prescription benefit management and organizations; claims, billing and other health care and insurance technology and data service organizations; other health, employee benefit, insurance and financial services product and solutions consultants, developers and vendors; and other health, employee benefit, insurance, technology, government and other management clients.
A former lead consultant to the Government of Bolivia on its Pension Privatization Project with extensive domestic and international public policy concerns in pensions, healthcare, workforce, immigration, tax, education and other areas, Ms. Stamer has been extensively involved in U.S. federal, state and local health care and other legislative and regulatory reform impacting these concerns throughout her career. Her public policy and regulatory affairs experience encompasses advising and representing domestic and multinational private sector health, insurance, employee benefit, employer, staffing and other outsourced service providers, and other clients in dealings with Congress, state legislatures, and federal, state and local regulators and government entities, as well as providing advice and input to U.S. and foreign government leaders on these and other policy concerns.
Beyond her public policy and regulatory affairs involvement, Ms. Stamer also has extensive experience helping these and other clients to design, implement, document, administer and defend workforce, employee benefit, insurance and risk management, health and safety, and other programs, products and solutions, and practices; establish and administer compliance and risk management policies; comply with requirements, investigate and respond to government; accreditation and quality organizations; private litigation and other federal and state health care industry investigations and enforcement actions; evaluate and influence legislative and regulatory reforms and other regulatory and public policy advocacy; training and discipline; enforcement, and a host of other related concerns. Ms. Stamer’s experience in these matters includes supporting these organizations and their leaders on both a real-time, “on demand” basis with crisis preparedness, intervention and response as well as consulting and representing clients on ongoing compliance and risk management; plan and program design; vendor and employee credentialing, selection, contracting, performance management and other dealings; strategic planning; policy, program, product and services development and innovation; mergers, acquisitions, and change management; workforce and operations management, and other opportunities and challenges arising in the course of their operations.
Ms. Stamer also has extensive health care reimbursement and insurance experience advising and defending plan sponsors, administrators, insurance and managed care organizations, health care providers, payers, and others about Medicare, Medicaid, Medicare and Medicaid Advantage, Tri-Care, self-insured group, association, individual and employer and association group and other health benefit programs and coverages including but not limited to advising public and private payers about coverage and program design and documentation, advising and defending providers, payers and systems and billing services entities about systems and process design, audits, and other processes; provider credentialing, and contracting; providers and payer billing, reimbursement, claims audits, denials and appeals, coverage coordination, reporting, direct contracting, False Claims Act, Medicare & Medicaid, ERISA, state Prompt Pay, out-of-network and other nonpar insured, and other health care claims, prepayment, post-payment and other coverage, claims denials, appeals, billing and fraud investigations and actions and other reimbursement and payment related investigation, enforcement, litigation and actions. Scribe for the ABA JCEB annual agency meeting with HHS OCR, she also has worked extensively on health and health benefit coding, billing and claims, meaningful use and EMR, billing and reimbursement, quality measurement and reimbursement, HIPAA, FACTA, PCI, trade secret, physician and other medical, workforce, consumer financial and other data confidentiality and privacy, federal and state data security, data breach and mitigation, and other information privacy and data security concerns.
Author of leading works on a multitude of health care, health plan and other health industry matters, the American Bar Association (ABA) International Section Life Sciences Committee Vice Chair, a Scribe for the ABA Joint Committee on Employee Benefits (JCEB) Annual OCR Agency Meeting, former Vice President of the North Texas Health Care Compliance Professionals Association, past Chair of the ABA Health Law Section Managed Care & Insurance Section, past ABA JCEB Council Representative and CLE and Marketing Committee Chair, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, Ms. Stamer’s health industry clients include public health organizations; public and private hospitals, healthcare systems, clinics and other health care facilities; physicians, physician practices, medical staff, and other provider organizations; skilled nursing, long-term care, assisted living, home health, ambulatory surgery, dialysis, telemedicine, DME, Pharma, clinics, and other health care providers; billing, management and other administrative services organizations; insured, self-insured, association and other health plans; PPOs, HMOs and other managed care organizations, insurance, claims administration, utilization management, and other health care payers; public and private peer review, quality assurance, accreditation and licensing; technology and other outsourcing; healthcare clearinghouse and other data; research; public and private social and community organizations; real estate, technology, clinical pathways, and other developers; investors, banks and financial institutions; audit, accounting, law firm; consulting; document management and recordkeeping, business associates, vendors, and service providers and other professional and other health industry organizations; academic medicine; trade associations; legislative and other law making bodies and others.
A popular lecturer and widely published author on health industry concerns, Ms. Stamer continuously advises health industry clients about contracting, credentialing and quality assurance, compliance and internal controls, workforce and medical staff performance, quality, governance, reimbursement, privacy and data security, and other risk management and operational matters. Author of works on Payer and Provider Contracting and many other managed care concerns, Ms. Stamer also publishes and speaks extensively on health and managed care industry regulatory, staffing and human resources, compensation and benefits, technology, public policy, reimbursement and other operations and risk management concerns.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other related concerns by her service in the leadership of the Solutions Law Press, Inc. Coalition for Responsible Health Policy, its PROJECT COPE: Coalition on Patient Empowerment, and a broad range of other professional and civic organizations including North Texas Healthcare Compliance Association, a founding Board Member and past President of the Alliance for Healthcare Excellence, past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children (now Warren Center For Children); current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee, current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Section, a current Defined Contribution Plan Committee Co-Chair, former Group Chair and Co-Chair of the ABA RPTE Section Employee Benefits Group, past Representative and chair of various committees of ABA Joint Committee on Employee Benefits; an ABA Health Law Coordinating Council representative, former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, a former member of the Board of Directors of the Southwest Benefits Association and others.
For more information about Ms. Stamer or her health industry and other experience and involvements, see here or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here such as:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advise or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2019. Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on Record-Setting 2018 Enforcement Show Proactive Health Plan HIPAA Compliance & Risk Management Need |
Comments Off on Record-Setting 2018 Enforcement Show Proactive Health Plan HIPAA Compliance & Risk Management Need |  21st Century Cures Act, Cafeteria Plans, Civil Monetary Penalties, Civil Rights, Cybercrime, Data Breach, Data Security, Discrimination, Electronic Medical Record, employee, Employee Benefits, Employer, Employers, fiduciary duty, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, Health IT, health plan, Health Plans, HIPAA, HIPAA, HR, Human Resources, Identity Theft, Insurance, insurers, Internal Controls, Managed Care, Mental Health, Mental Health Parity, Patient Empowerment, Uncategorized | Tagged: Data Breach, Data Security, Employer, Health Plan, HIPAA, Privacy |
21st Century Cures Act, Cafeteria Plans, Civil Monetary Penalties, Civil Rights, Cybercrime, Data Breach, Data Security, Discrimination, Electronic Medical Record, employee, Employee Benefits, Employer, Employers, fiduciary duty, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, Health IT, health plan, Health Plans, HIPAA, HIPAA, HR, Human Resources, Identity Theft, Insurance, insurers, Internal Controls, Managed Care, Mental Health, Mental Health Parity, Patient Empowerment, Uncategorized | Tagged: Data Breach, Data Security, Employer, Health Plan, HIPAA, Privacy |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
December 27, 2018
Today’s diverse business environment creates a demand for businesses to think creatively about their employment relationships, including creative scheduling and pay arrangements. While many of these arrangements produce win/win solutions for both the business and its employees, businesses need to use care properly to evaluate and manage minimum wage, overtime, and other wage and hour law responsibilities under the Fair Labor Standards Act (“FLSA”) and applicable state law.
A new Department of Labor Wage and Hour Division (WHD) Fair Labor Standards Act (FLSA) opinion letter published December 21 illustrates this point. WHD Opinion Letter FLSA 2018-28 (Dec. 21, 2018) evaluates FLSA minimum wage and overtime compliance of one employer’s innovative strategy of paying certain hourly employees one hourly rate while the employee was working with clients and a second, lower hourly rate of pay for time that the employee spent traveling between client sites throughout the day.
In WHD Opinion Letter FLSA 2018-28 (Dec. 21, 2018), the WHD expresses reservations about whether the specific practices of the requesting employer for calculating overtime for workers paid different hourly rates for different categories of work during the same work week fulfill the FLSA overtime requirements under certain circumstances, but blessed the compliance of the practice of the employer with the FLSA minimum wage rules.
While only the employer that actually requested the ruling that resulted in the Opinion actually may rely upon the Opinion, the ruling highlights both the potential opportunity for businesses to structure innovative compensation and scheduling arrangements within the requirements of the FLSA and other laws, as well as the legal exposures that employers using innovative staffing and compensation arrangement risk by failing to appropriately manage these responsibilities.
FLSA Minimum Wage & Overtime Requirements Generally
The FLSA generally requires that employers pay covered, nonexempt employees receive at least the federal minimum wage (currently $7.25 per hour) for all hours worked. See 29 U.S.C. § 206(a)(1). According to previously published WHD guidance, WHD will consider an employer to have fulfilled this requirement “if the employee’s total wages for the workweek divided by compensable hours equal or exceed the applicable minimum wage.” See WHD Opinion Letter FLSA2004-8NA (Aug. 12, 2004)(different pay rates for trucking company workers); WHD Field Operations Handbook § 30b02.
In addition to the requirement to pay at least the minimum wage, the FLSA also requires that covered, nonexempt employees receive overtime compensation of at least one and one-half times their regular rate of pay for time worked in excess of 40 hours per workweek. See 29 U.S.C. § 207(a)(1). To determine the regular rate of pay for purposes of calculating the required overtime, an employer generally divides the employee’s “remuneration for employment” (subject to the exclusions in 29 U.S.C. § 207(e)) by the total hours worked for the workweek. See 29 C.F.R. § 778.109.
WHD Opinion Letter FLSA 2018-28
In WHD Opinion Letter FLSA 2018-28 (Dec. 21, 2018), WHD addressed its views regarding a home health provider’s practice for calculating the wages due to home health aide services that traveled to home health clients’ homes, who were required to travel to different client home locations during the workday. The employer establishes different rates of pay for time spent working with clients versus time spent traveling from location to location. To calculate weekly pay, that employer multiplied an employee’s time with clients by his hourly pay rate established by the employer for time spent working with clients. The employer then divides the product by the employee’s total hours worked, which includes both the client time and the travel time. The employer guarantees that the quotient meets both federal and state minimum wage rate requirements.
According to the facts published in the WHD Opinion Letter, the home health provider represented that a typical standard rate of pay is $10.00 per hour with a client including travel time,” and that “[i]f any employee works over 40 hours (total paid hours and [travel] time) in any given workweek, the employer pays the employee time and a half for all time over 40 hours at a rate of $10.00.”
Based upon the factual representations made by the home health agency, WHD ruled the employer’s compensation plan complies with the FLSA’s minimum wage requirements but expressed concern about whether the employer’s practices for calculating overtime complied with the FLSA.
Concerning the FLSA minimum wage compliance, the WHD found that the employers practice fulfilled the FLSA minimum wage requirements because even though the employee’s average hourly pay rate varied from workweek to workweek, the employer always ensured that the average hourly pay rate exceeded the FLSA’s minimum wage requirement for all hours worked.
In contrast, however, WHD expressed concern about the compliance of the employer’s compensation plan with the FLSA’s overtime requirements under certain circumstances. WHD states in the Opinion that the employer will not pay all overtime due to employees whose actual rate of pay exceeds $10 per hour if the employer always assumes a regular rate of pay of $10 per hour when calculating overtime due. See 29 C.F.R. § 778.107.
The Opinion notes that “neither an employer nor an employee may arbitrarily choose the regular rate of pay; it is an “actual fact” based on “mathematical computation.” Walling v. Youngerman-Reynolds Hardwood Co., Inc., 325 U.S. 419, 424–25 (1945); 29 C.F.R. § 778.108.
On the other hand, the Opinion also states that the employer’s compensation plan would comply with the FLSA’s overtime requirements for all employees whose actual regular rates of pay are less than $10 per hour, as an employer may choose to pay an overtime premium in excess of the required amount. See, e.g., Molina v. First Line Solutions LLC, 566 F. Supp. 2d 770, 779 (N.D. Ill. 2007).
The cautionary lessons from FLSA Opinion 2018-28 echo those WHD previously has issued alerting businesses to the need to use care to properly understand and meet FLSA requirements when structuring and administering two-tier hourly pay or other innovative pay and scheduling arrangements.
egular drivers a specified hourly rate with a minimum guarantee of two hours driving time pay per route/additional assignment. The contract also provided that for an assigned trip of less than two hours, a driver that wanted to receive pay for hte minimum guaranteed time had to perform regular maintenance in the bus garage or other work as assigned by the School District to complete the two hours. Furthermore, the contract also specified that “Any regular driver may complete a voucher for payment for additional time if their morning or afternoon route exceeds his/her assigned time by one half hour or more” and that the employers only would pay additional wages for the actual added time worked to employees that worked at least 30 minutes or more without rounding to the next hour for calculating wages. Thus, an employee that worked an additional twenty-five minutes beyond his/her normal shiftwould not be compensated for the extra time worked. Meanwhile, a bus driver that returned fifty minutes past the scheduled time received pay for an additional 50 minutes of work.
WHD’s issue with the arrangement was that the rounding practices applied under the arrangement meant that the school district did not ensure that workers were paid at least the minimum wage per hour for all hours worked and might under some circumstances not properly pay overtime due to workers.
While acknowledging that Labor Regulation Section 785.47 allows employers to disregard ‘insubstantial or insignificant periods of time outside the scheduled working hours that cannot practically be precisely recorded as de minimis, WHD noted that the de minimis rule applies only where a few seconds or minutes of work are involved and where the failure to count such time is due to considerations justified by industrial realities. It does not allow an employer by contract or otherwise to arbitrarily fail to count as hours worked any part, however small, of the employee’s fixed or regular working time. Where an employer fails to pay an employee for any part of the employee’s fixed or regular working time, however small, this would be considered a violation of the FLSA.
Concerning the FLSA’s requirement that the employer pay hourly employees at least the minimum wage, WHD noted that in non-overtime workweeks or in workweeks in which the overtime provisions do not apply, WHD would consider the employer to have met the minimum wage requirement if the employee’s total wages for the workweek divided by compensable hours equal or exceed the applicable minimum wage. WHD added that this principle would apply even if the employer technically did not compensate the emploeye for time which is compensable under the FLSA.
Concerning the overtime requirements of the FLSA, however, WHD had greater reservations. As WHD noted in the 2004 Opinion, when a covered and non-exempt employee works overtime, a different rule applies. The FLSA overtime rule requires that an employer pay the employee for all hours worked at the agreed rate plus the overtime premium (one-half the regular rate) for all overtime hours. Therefore, before an employee can be said to be paid statutory overtime compensation due, the employee must first be paid all straight time wages due for all hours worked under any express or implied contract or under any applicable statute (see 29 CFR Part 778.315). As a result, WHD found that the FLSA overtime requirements would require the employer both to ensure that the employee actually was paid for each hour of straight time at the regular rate of pay plus time and a half of the regular rate of pay for each overtime hour worked.
WHD additionally noted in the 2004 Opinion that the employer also risked violation of Labor Regulation 516.2(a)(7)’s requirement that the employer maintain accurate recordkeeping of hours worked each workday and total hours worked each workweek for covered, nonexempt employees if the payroll records do not accurately record the number of hours worked in one or more of the workdays.
Takeaways For Other Employers About Using Variable Pay Rates & Other Innovative Scheduling & Pay Practices
While other employers actually cannot rely upon either WHD Opinion Letter FLSA 2018-28, , or most other WHD Opinion Letters, WHD Opinion Letters and other publishe guidance, as well as judicial precedent and the enforcement conduct by WHD provide a wealth of valuable insights for other employers about the potential FLSA opportunities and pitfalls of using variable rates of pay or other innovative compensation, scheduling and timekeeping practices for compensating hourly employees. Employers using or contemplating using innovative compensation, scheduling or recordkeeping practices should should seek assistance from experienced legal counsel with accessing and using this guidance to help reduce the risk that a proposed innovative compensation or other practice for scheduling or paying nonexempt hourly workers will trigger unanticipated FLSA or other liabilities..
Make Wage & Hour Compliance & Risk Management Priority To Reduce Exposures
Aside from using caution to properly calculate and pay overtime for workers paid different rates for different types of work, employers also need to use care to avoid other common FLSA and other wage and hour overtime violations.
With the Trump Administration U.S. Department of Labor Wage and Hour Division (WHD) continuing its aggressive investigation and enforcement of minimum wage, overtime and other Fair Labor Standards Act (FLSA) and other wage and hour laws it used to recover more than $1.2 billion in back pay for workers over the past five years, Agriculture, Amusement, Apparel Manufacturing, Auto Repair, Child Care Services, Construction, Food Services, Guard Services, Hair, Nail & Skin Care Services, Health Care, Hotels and Motels, Janitorial Services, Landscaping Services, Retail, and Temporary Help and other U.S. employers should evaluate their current and past potential liability exposures and consider using the new pilot WHD self-audit Payroll Audit Independent Determination (PAID) program announced by WHD on March 6 or other options to mitigate their liability for their own or temporary or other contract labor’s existing or past minimum wage and hour law violations.
U.S. employers and leaders with wage and hour management authority risk substantial liability from unresolved violations of the FLSA and other federal and state wage and hour laws.
One of the most frequently violated and litigated federal employment laws, the FLSA generally requires that U.S. employers pay nonexempt employees at least $7.25 per hour for all regular compensable hours worked, plus time and one-half their regular rates, including commissions, bonuses and incentive pay, for hours worked beyond 40 per week. In general, FLSA “hours worked” includes all time an employee must be on duty, or on the employer’s premises or at any other prescribed place of work, from the beginning of the first principal work activity to the end of the last principal activity of the workday. Similar state or local laws often also impose higher minimum wage, compensable hour, break and other requirements than federal law requires.
The FLSA and most applicable state and local wage and hour laws also mandate that employers maintain records of the hours worked by employees by non-exempt employees, documentation of the employer’s proper payment of its non-exempt employees in accordance with the minimum wage and overtime mandates of the FLSA, and certain other records and prohibit retaliation by an employer or other person again an employee or other person for asserting rights under the law or cooperating in a WHD investigation about FLSA compliance.
Beyond these FLSA minimum wage and overtime requirements, WHD regulations and court decisions provide guidance on when an employer must treat “on-call” time, travel time, meal and break times, and certain other time periods as compensable hours worked by a non-exempt employee, when “comp time” in lieu of the payment of wages is permitted, various alternative methods for calculating overtime under certain special circumstances, and various other rules applicable to various special circumstances. Other special rules also can apply to businesses employing tipped employees, home workers, child labor, certain farm workers, workers working with special visas, and other special classes or workers. Furthermore, collective bargaining agreements or other contracts or other federal, state or local laws also sometimes impose additional requirements for employers to pay higher “prevailing wages,” apply special rules for counting compensable work hours, and provide specified fringe benefits or other special compensation or protections or other wages, when the employer is a government contractor or subcontractor covered by the Service Contract Act, the Davis Bacon Act or other similar federal or state statutes.
Over the past decade, WHD and private enforcement of the FLSA and other wage and hour laws generally has skyrocketed in part driven by the Obama Administration’s prioritization on raising the minimum wage, extending federal wage and hour protections, and expanding WHD and other enforcement. WHD’s success in recovering more than $1.2 billion in back pay for workers over the past five years and other achievements in expanding its own and private oversight and enforcement and the continuation of these efforts under the Trump Administration means all employers need to view wage and hour law as a major liability risk requiring conscientious management. However, the risk of enforcement is particularly acute for businesses in the following industries, designed for heightened enforcement and other attention as “Low Wage High Violation Industries” based on their particularly high record of noncompliance: Agriculture, Amusement, Apparel Manufacturing, Auto Repair, Child Care Services, Construction, Food Services, Guard Services, Hair, Nail & Skin Care Services, Health Care, Hotels and Motels, Janitorial Services, Landscaping Services, Retail, and Temporary Help.
Scrutiny & Challenges To Contract & Outsourced Labor Relationships Rising
Beyond assessing their FLSA and other wage and hour compliance and associated exposures from the worker on their own payroll, U.S. employers and their leaders also should take care to carefully evaluate potential exposures from nontraditional services relationships and act to manage those risks.
Misclassification of workers providing services as non-employees increasingly causes U.S. businesses to incur unanticipated FLSA and other wage and hour law liability for back pay, liquidated punitive damages, civil monetary penalties and other liability, in part because of WHD’s stepped up worker education, scrutiny, investigation, and enforcement challenging employers’ treatment of workers as non-employees.
The FLSA and state and local rules generally apply to any workers that the employer who receives its services cannot prove is not its common law employee or an exempt employee within the meaning of the FLSA. The FLSA and most other wage and hour laws generally rules presume that workers rendering services are common law employees of the business in most circumstances. Businesses should evaluate their FLSA exposures from both workers they recognize as common law employees and those performing services in capacities that the business typically does not view as common law or otherwise covered by the FLSA when managing FLSA compliance and evaluating exposures, employers should exercise care not to overlook potential responsibilities and exposures associated with outsourced services provided through relationships characterized by the employer as subcontractors, independent contractors, lease employees, or other common outsourced relationships.
Court decisions and regulations provide guidance for determining when leased, contract, jointly employed, independent contractor or other non-traditionally employed workers will be treated as employees of a business, As in many other enforcement areas, The WHD and many other agencies increasingly view the misclassification of workers as something other than employees, such as independent contractors, leased employees and other common “outsourced” relationship as a serious problem for affected employees, employers and to the entire economy.
According to the Labor Department, misclassified employees are often denied access to critical benefits and protections, such as family and medical leave, overtime, minimum wage and unemployment insurance and other rights. The Labor Department also says employee misclassification also generates substantial losses to state and federal treasuries, and to the Social Security and Medicare funds, as well as to state unemployment insurance and workers compensation funds. To address these and other concerns, the Labor Department has joined other agencies like the Internal Revenue Service increasingly is challenging employers’ treatment of workers as exempt from FLSA and other legal obligations as independent contractors or otherwise.
In response to these concerns, WHD published guidance warning employers about misclassification of workers about potential violation of the FLSA by improper misclassification of workers as independent contractors or non-employed. See Department of Labor Issues Guidance of Misclassification of Workers. DOL’s key points in the guidance are that:
- Most workers are employees under the broad definitions of the FLSA;
- No single factor is determinative;
- Employers should be wary of classifying workers as independent contractors merely because the workers control some aspects of their work; and
- The ultimate question is whether a worker “is really in business for him or herself (and thus is an independent contractor) or is economically dependent on the employer (and thus is an employee).
Other guidance makes clear that WHD and other agencies concerns about misclassification extend beyond workers labeled independent contractors to include scrutiny of subcontractor, day labor, temporary, leased employee and a broad range of other outsourced services relationships. See here,
Consistent with these principles, WHD and private litigants in recent years have increasingly scrutinized and successfully challenged employers’ failure to comply with the FLSA’s minimum wage, overtime, recordkeeping and other rules with respect to these outsourced workers. See e.g., $1.4M FLSA Back Pay Award Demonstrates Worker Misclassification Risks; Employer Faces $2M FLSA Lawsuit For Alleged Worker Misclassification; $754,578 FLSA Settlement Shows Employer Risks From Worker Misclassification, Underpayment; WHD now both conducts significant worker education outreach and regularly requests and scrutinizes the characterization of and FLSA compliance of outsourced workers in connection with its FLSA investigations and audits. See e.g. Get the Facts on Misclassification Under the FLSA; Am I an Employee?: Employment Relationship Under the Fair Labor Standards Act (FLSA); Compliance Assistance Page – Fair Labor Standards Act; Elaws: Independent Contractors; Know Your Rights Video Series: Misclassification as an Independent Contractor; WHD Press Releases about employee Misclassification as Independent Contractors. These and other developments are significantly increasing the likelihood that businesses will face WHD or private litigants challenges to its FLSA compliance relating to workers rendering services as independent contractors, subcontractors or other outsourced services providers.
Employers often face substantial challenges responding to, much less, containing their FLSA exposures when a WHD or a private litigant successfully challenges the employer’s classification of the worker as a non-employee for a variety of reasons. Beyond the likelihood of violations resulting from the employer’s failure to recognize it might owe minimum wage and overtime duties to the worker, an employer often lacks records and other data needed to fulfill recordkeeping and posting requirements and to accurately demonstrate hours worked and hourly rates to limit resulting back pay exposures because these workers are not treated as part of the employer’s workforce. Obtaining the necessary records to respond to a WHD or other investigation, lawsuit or other action often proves challenging because the independent contractor, leasing company, or other provider or of the services often becomes unavailable, is disincentivized by its own noncompliance or other interests, has failed to maintain necessary documentation or otherwise fails to cooperate in the delivery of these materials. Furthermore, as leased employee, staffing, independent contractor and other outsourced arrangements invoice services at higher rates of compensation payment than the employer might otherwise have paid a traditionally employed worker, the lack of records and elevated compensation rates tend to push up the compensation used to calculate back pay and other awards. Accordingly, employers utilizing these arrangements should use care in structuring and administering these arrangements properly to evaluate their likely FLSA and other treatment and to manage these risks.
FLSA Big Liability Risk
Under the FSLA and applicable state wage and hour laws, violations of the FLSA and other federal or state wage and hour laws expose employers to substantial back pay, interest and punitive damages, civil monetary penalties for willful or and in the case of willful or repeated violations and in the case of willful violations, criminal prosecution.
Because of the ability to recover liquidated damages and attorneys’ fees in addition to unpaid back pay, private enforcement of the FLSA is common. The FLSA generally allows employees wrongfully denied wages in violation of the FLSA to bring lawsuits to enforce their rights provided that the WHD has not or does not intervene to enforce those rights on the worker’s behalf. Workers successfully proving an employer violated their FLSA rights typically can recover back pay, plus liquidated damages, interest, attorneys’ fees and other costs of enforcement from the breaching employer. In some cases, Corporate officers such as CEOs, CFOs or COOs and other management leaders with control over the breaching employer’s financial affairs also be held personally liable for the unpaid wages See e.g., Lamonica v. Safe Hurricane Shutters, +2013 U.S. App. LEXIS 4599 (11th Cir. 2013)(ruling personal liability for FLSA violations can attach to any individual with control over an employer’s financial affairs who could potentially cause an employer to violate FLSA).
As an alternative to private litigation, the FLSA empowers the WHD to supervise or if necessary, enforce through litigation the rights of workers against a breaching employer to recover back pay plus liquidated damages in an amount equal to the wrongfully denied wages. WHD also can pursue injunctive relief against noncompliant employers.
When the employer is a repeat offender or willfully violated the FLSA, additional consequences attach. A violation is “willful” for purposes of FLSA criminal prosecution if it is deliberate, voluntary, and intentional. A fine of up to $10,000 on the first conviction
When an employer’s violation of the FLSA is repetitious or willful, the FLSA empowers WHD to impose civil money penalties (CMPs) against the noncompliant employer in addition to the recovery of back pay and liquidated damages. Intended to discourage future noncompliance by an employer guilty of violating the FLSA, CMPs for a “repeated” violation are assessable when the employer had previously violated the minimum wage or overtime requirements of the FLSA. CMPs for a “willful” violation may be assessed when it can be shown that the employer knew that its conduct was prohibited by the FLSA or showed reckless disregard for the requirements of the FLSA. CMPs ordinarily are imposed based on violations occurring within the normal two-year investigation period. Where violations are determined to be willful, the investigation will cover a three-year period.
The applicable 2018 CMP amounts, which are adjusted annually for inflation, are as follows:
| Type of Violation |
Statutory Citation |
CFR Citation |
Maximum Civil Monetary Penalty on or before 1/2/2018 |
Maximum Civil Monetary Penalty on or after 1/3/2018 |
| Homeworker:
Violation of recordkeeping, monetary, certificate or other statutes, regulations or employer assurances. |
29 USC 211(d) |
29 CFR 530.302 |
$1,005 |
$1,026 |
| Child labor:
(1) Violation of child labor standards (sec 212 or 213(c)); |
29 USC 216(e)(1)(A)(i) |
29 CFR 570.140(b)(1) and 29 CFR 579.1(a)(1)(i)(A) |
$12,278 |
$12,529 |
| (2) Violation of child labor standards (sec 212 or 213(c)) that causes the serious injury or death of a minor; |
29 USC 216(e)(1)(A)(ii) |
29 CFR 570.140(b)(2) and 29 CFR 579.1(a)(1)(i)(B) |
$55,808 |
$56,947 |
| (3) Willful or repeated violation of child labor standards (sec 212 or 213(c)) that causes the serious injury or death of a minor |
29 USC 216(e)(1)(A)(ii) |
29 CFR 570.140(b)(2) and 29 CFR 579.1(a)(1)(i)(B) |
$111,616 |
$113,894 |
| (4) Repeated or willful violation of section 206 or 207. |
29 USC 216(e) |
29 CFR 579.1(a)(2) |
$1,925 |
$1,964 |
|
|
|
|
|
| Minimum Wage and Overtime:
Repeated or willful violation of section 206 or 207. |
29 USC 216(e)(2) |
29 CFR 578.3(a) |
$1,925 |
$1,964 |
Although typically reserved for more egregious violations, “willful” violations of the FLSA can trigger criminal prosecution by the Department of Justice. A fine of up to $10,000, or a term of imprisonment of up to six months, or both, on all convictions after the first conviction
In addition to or instead of lawsuits by the Secretary of Labor for back wages or injunctive relief, willful violation of the FLSA also can trigger criminal prosecutions against an employer by the Department of Justice. Criminal penalties for willful FLSA violations include a fine of up to $10,000, or a term of imprisonment of up to six months, or both, on all convictions after the first conviction. Since enforcement actions by the DOJ can be brought instead of or in addition to lawsuits by WHD for back wages or injunctive relief, an employer that willfully violates the FLSA can be ordered to pay liquidated damages and back-pay, as well as any court imposed criminal fine or penalty.
Always popular, WHD and private enforcement of the FLSA initially spiked upward following the highly publicized George W. Bush Administration’s implementation of updated FLSA “white collar” regulations regarding the classification of workers as exempt. The Obama Administration’s highly publicized, but unsuccessful, campaign to increase the minimum wage and aggressive FLSA educational outreach and enforcement further fueled this trend. While President Trump has opposed proposals to increase the federal minimum wage, he has expressed his commitment to protect workers’ FLSA rights through continued vigorous enforcement of the FLSA minimum wage, overtime and other rules.
As a result of its aggressive enforcement commitments, WHD takes credit for having recovered more than $1.2 billion in back wages on behalf of more than 1.3 million workers over the past five years. See here. The following WHD enforcement statistics reflect that its commitment to FLSA enforcement has continued during President Trump’s tenure in office.
|
|
Cases with Violations |
Back Wages |
Employees Receiving Back Wages(duplicated 1) |
| FY 2011 |
Minimum Wage |
12,450 |
$29,327,527 |
89,305 |
| Overtime |
11,990 |
$140,328,012 |
204,243 |
| FY 2012 |
Minimum Wage |
12,532 |
$35,270,524 |
107,005 |
| Overtime |
12,462 |
$148,560,700 |
218,137 |
| FY 2013 |
Minimum Wage |
12,403 |
$38,470,100 |
103,671 |
| Overtime |
12,108 |
$130,703,222 |
174,197 |
| FY 2014 |
Minimum Wage |
11,042 |
$36,732,407 |
106,184 |
| Overtime |
11,238 |
$136,239,001 |
174,365 |
| FY 2015 |
Minimum Wage |
10,642 |
$37,828,554 |
86,229 |
| Overtime |
10,496 |
$137,701,703 |
173,330 |
| FY 2016 |
Minimum Wage |
10,722 |
$34,964,350 |
81,870 |
| Overtime |
10,884 |
$171,917,225 |
209,819 |
| FY 2017 |
Minimum Wage |
10,687 |
$31,213,737 |
69,588 |
| Overtime |
10,823 |
$157,592,682 |
183,272 |
Pilot PAID Program May Offer New Option To Resolve WHD Exposures
When an audit uncovers potential violations, some employers may want to explore options to voluntarily resolve their exposures. To encourage voluntary compliance, the WHD on March 6, 2018 announced a new pilot self-audit Payroll Audit Independent Determination (PAID) program that offered employers accepted into the program after voluntarily disclosing violations to resolve their exposure WHD penalties and liquidated damages commonly assessed by WHD against employers for violating the FLSA minimum wage and overtime violations by:
- Voluntarily disclosing the violations to WHD before becoming subject to investigation or enforcement and requesting admission to the program;
- Paying affected workers 100 percent of the unpaid back pay due wrongfully denied by the end of the next full pay period after receiving the summary of unpaid wages from WHD confirming the back pay amount;
- Working with WHD prospectively to correct noncompliant practices; and
- Taking other actions to correct and prevent a recurrence of those violations.
Originally slated as a pilot program set to expire after six months, the PAID program remains an opportunity offered by WHD on its website, which also shares “testimonials” from various employers that report having participated in the PAID program.
While participation in the PAID program purpoerts to offer allows a participating employer to settle its exposure to prosecution for those violations by WHD without incurring some of themore extraordinary penalties that WHD is authorized to assess, many practitioners and employers report having achieved similar and in some cases even more favorable outcomes through negotiations conducted outside the PAID program. Furthermore, many employers may face challenges in using the program as a result of the inability to marshal the required capital to pay 100 percent of the back pay due within the required time period.
Beyond this challenge, employers evaluating whether to seek relief through the new PAID program also may need to weigh a variety of other concerns.
For instance, employers considering participation need to understand that the settlement only addresses potential liability from WHD enforcement. While WHD’s requirement that a participating employer pay affect 100 percent of any wrongfully denied back pay to the impacted employees generally would reduce the actual back pay damages recoverable by an employee in a private enforcement action, WHD says settlements reached with the WHD under the PAID program does not prevent employees wrongfully denied wages in violation of FSLA from bringing private lawsuits. Rather, WHD states that it will be purely the employee’s choice whether to accept the payment of back wages the employer agrees to pay under the PAID program settlement. If the employee chooses to not accept the payment, the employee will not release any private right of action. Additionally, if the employee chooses to accept the payment, the employee will not grant a broad release of all potential claims under the FLSA. Rather, the releases are tailored to only the identified violations and time period for which the employer is paying the back wages. The WHD also cautions that regardless of whether the employee accepts or rejects the back pay specified in the PAID program, the FLSA will prohibit employers from retaliating against the employee for his or her choice. Furthermore, while the payment of previously unpaid amounts could reduce the amount of unpaid wages for purposes of determining liability for state wage and hour law violations, the WHD settlement does not directly impact or release liability for any state wage and hour violations.
While any FLSA covered employer may use the program, interested employers should understand that acceptance into the program is not automatic and is not available for all FLSA violations. Rather, the PAID program only covers potential violations of the FLSA’s overtime and minimum wage requirements that an employer self-identifies and voluntarily discloses and resolves in accordance with its PAID program settlement with WHD. An employer cannot use the PAID program to resolve any issues for which WHD is already investigating the employer, or which the employer is already litigating in court, arbitration, or otherwise. An employer likewise may not initiate the process when an employee’s representative or counsel has already communicated an interest in litigating or settling the issue. Employers using the Paid program also must be prepared to correct the noncompliant practices that resulted in the violations settled under the PAID program. According to the WHD, WHD will not allow employers to use the program to repeatedly resolve the same violations, as this program is designed to identify and correct non-compliant practices. By allowing employers to participate in the PAID program, WHD also does not waive its right to conduct any future investigations of the employer.
Employers contemplating participation in the PAID program generally should conduct a self-audit after updating their understanding of WHD program and compliance assistance materials and other WHD guidance. Because the information, analysis and discussions conducted in this process may be legally sensitive, employers generally will want to engage qualified legal counsel before initiating these processes to advise and assist the employer about the adequacy and risks of its existing practices, recommendations for redressing known compliance issues and other risks as well as opportunities and procedures for qualifying certain of these actions and discussions for coverage under attorney-client privilege, attorney work product or other evidentiary protections.
Whether or not an employer decides based on the audit to pursue compliance resolution through the PAID program, employers generally should work with their legal counsel within the scope of attorney client privilege to organize and retain documentation of their audit, its findings of compliance and, for any potential compliance issues, corrective actions taken to redress those issues retrospectively and prospectively, and other documentation that the employer might need to pursue resolution under the PAID program or otherwise respond to and defend against a WHD or private charges brought by an employee in the future.
If the employer wishes to pursue resolution of potential violations under the PAID program based on review of the audit findings in conjunction with their legal counsel, the employer in coordination with the legal counsel within the scope of attorney client privilege should work together to prepare and assemble the records and information WHD will expect the employer to provide in the initial phases of the process including:
- A list of the specific potential violations uncovered
- The specific employees affected
- The specific timeframes in which each employee was affected, and
- The calculation of the amount of back wages the employer believes are owed to each employee.
- Each of the calculations described above—accompanied by both evidence and explanation concerning how the calculations were made;
- A concise explanation of the scope of the potential violations for possible inclusion in a release of liability;
- A certification that the employer reviewed all of the information, terms, and compliance assistance materials;
- A certification that the employer is not litigating the compensation practices at issue in court, arbitration, or otherwise, and likewise has not received any communications from an employee’s representative or counsel expressing interest in litigating or settling the same issues; and
- A certification that the employer will adjust its practices to avoid the same potential violations in the future.
After preparing this information, the employer generally will want to arrange for legal counsel to make the preliminary contact to the WHD to request that the WHD admit the employer to the PAID program. During the preliminary contact, the WHD will require that a list of the specific potential violations, and the identity, specific time frame and back pay amount that employer believes it owes to each affected employee as a prerequisite to considering the request for admission to the program. If the WHD approves the employer’s request, WHD will require that the employer or its legal counsel on its behalf provide the remaining information listed above. After evaluating this information, WHD will provide notification of the next steps, including the collection of any other information necessary for WHD to assess and confirm the back wages due for the identified violations.
Current published guidance states that after WHD assesses the back wages due, it will issue a summary of unpaid wages. WHD will also issue forms describing the settlement terms for each employee, which employees may sign to receive payment. The release of claims provided in the form will match the previously agreed-upon language and, again, must be limited to only the potential violations for which the employer had paid back wages. The PAID program settlement will require the employers to pay the back pay amounts confirmed in the summary of unpaid wages promptly and in full by the end of the next payroll period after receiving the WHD summary of wages confirming the back pay amounts required.
Audit & Act To Mitigate FLSA & Other Wage & Hour Risks
Regardless of whether an employer elects to pursue using the new PAID program, all FLSA covered employers generally should consult with legal counsel within the scope of attorney-client privilege to assess the defensibility of their existing practices for classifying and compensating workers under existing Federal and state wage and hour laws, tighten contracting and other compliance oversight in relation to outsourced services, and about using the PAID program and other options to minimize their potential liability under applicable wages and hour laws. Conducting this analysis within the scope of attorney-client privilege is important because the analysis and discussions are highly sensitive both as potential evidence for wage and hour and other legal purposes. Consequently, businesses and their leaders generally will want to arrange for this work to be protected to the extent by attorney-client privilege, work product and other evidentiary protections against discovery by WHD, employees or others for FLSA or other workforce enforcement actions.
As a part of this process, businesses and their leaders generally should plan to:
- Review subcontractor, temporary, lease employee, independent contractor and other outsourced labor and services relationship for potential risk of worker reclassification and tighten contracting and other procedures;
- Audit the position of each employee currently classified as exempt to assess its continued sustainability and to develop documentation justifying that characterization;
- Audit characterization of workers obtained from staffing, employee leasing, independent contractor and other arrangements and implement contractual and other oversight arrangements to minimize risks that these relationships could create if workers are recharacterized as employed by the employer receiving these services;
- Review the characterization of on-call and other time demands placed on employees to confirm that all compensable time is properly identified, tracked, documented, compensated and reported;
- If the employer hires any individuals under age 18, audit and implement appropriate procedures to ensure its ability to demonstrate compliance with all applicable FLSA child labor rules;
- If the employer is a government contractor or subcontractor or otherwise performs any services on projects funded with federal or state funds, evaluate the applicability and fulfillment of any special wage, fringe benefit, recordkeeping or other government contracting wage and hour requirements;
- If the employer hires foreign agricultural or other workers subject to special conditions and requirements, to review compliance with those special requirements;
- Review and tighten existing practices for tracking compensable hours and paying non-exempt employees for compliance with applicable regulations and to identify opportunities to minimize costs and liabilities arising out of the regulatory mandates;
- If the employer uses leased, temporary, or other outsourced labor, evaluate contractual, process and other options to support the employer’s ability cost effectively to respond to an audit, investigation or enforcement action by WHD or private litigants and if necessary, obtain indemnification or other recovery in the event the employer incurs liability due to the use or practices of the outsourced labor supplier;
- If the audit raises questions about the appropriateness of the classification of an employee as exempt, self-initiation of proper corrective action after consultation with qualified legal counsel;
- Review and document all workers classified as exempt;
- Review of existing documentation and record keeping practices for hourly employees;
- Evaluate potential exposures under other employment, labor, tax or related laws or contracts that might be impacted by the findings or actions taken in response to those findings;
- Explore available options and alternatives for calculating required wage payments to non-exempt employees and assessing and resolving other concerns;
- Identify and calculate other employee benefit, tax or other corrections and associated costs and procedures that may be required as a result of findings or corrective actions resulting from their redress;
- Re-engineer work rules, policies, contracts and practices to minimize costs and liabilities as appropriate in light of the regulations and enforcement exposures;
- Explore insurance, indemnification and other options for mitigating risks and associated investigation and defense costs .
- Pursue self-correction within the new PAID Program or otherwise.
Many employers also will want to consider adopting or strengthening their use of arbitration agreements, strengthening contract compliance, audit, indemnification and other contractual safeguards in staffing and other outsourcing contracts and broadening employment practices and other liability insurance coverage to mitigate and manage these exposures.
For additional information, please contact the author or other qualified legal counsel with health industry wage and hour and other labor and employment experience.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer is nationally and internationally recognized for her work assisting businesses, governments, and other entities to develop, implement, administer and defend pragmatic strategies for dealing with employment and other workforce and related compensation, employee benefit, performance management and internal controls, insurance, health care and finance concerns to manage risk, operations and other business objectives.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
The author of the “Texas Payday Act,” and numerous other highly regarded publications on wage and hour and other human resources, employee benefits and compensation publications, Ms. Stamer is well-known for her 30 years of extensive wage and hour, compensation and other management advice and representation of restaurant and other hospitality, health, insurance, financial services, technology, energy, manufacturing, retail, governmental and other domestic and international businesses of all types and sizes.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here including:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on Creative Pay & Time Keeping Requires FLSA Compliance & Risk Management |
Comments Off on Creative Pay & Time Keeping Requires FLSA Compliance & Risk Management |  Attorney-Client Privilege, board of directors, Brokers, business travel, Child Labor, compensation, compliance, Construction, Corporate Compliance, corporate governance, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Policies, enforcement, Executive Compensation, Exempt, Fair Labor Standards Act, FLSA, HR, Human Resources, Insurance, Internal Controls, Internal Investigations, Labor Management Relations, Management, Managment, officers, Overtime, Telecommuting, Uncategorized, Union, Workforce | Tagged: Employer, FLSA, wage, Wage & Hour |
Attorney-Client Privilege, board of directors, Brokers, business travel, Child Labor, compensation, compliance, Construction, Corporate Compliance, corporate governance, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Policies, enforcement, Executive Compensation, Exempt, Fair Labor Standards Act, FLSA, HR, Human Resources, Insurance, Internal Controls, Internal Investigations, Labor Management Relations, Management, Managment, officers, Overtime, Telecommuting, Uncategorized, Union, Workforce | Tagged: Employer, FLSA, wage, Wage & Hour |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
December 18, 2018
Businesses that reimburse employee moving expenses should review their practices in response to changes to the Internal Revenue Code rules on qualified moving expenses. The requirement to treat moving expenses as taxable is just one of many changes to the treatment of fringe benefits and compensation under the Internal Revenue Code (“IRC”) as part of the tax reforms enacted last year.
Under previous law, payment or reimbursement of an employee’s qualified moving expenses were not subject to income or employment taxes.
Under last year’s tax reform legislation, however, employers generally must include all moving expenses, in employees’ wages, subject to income and employment taxes.
Exception
Generally, members of the U.S. Armed Forces can still exclude qualified moving expense reimbursements from their income if:
- They are on active duty
- They move pursuant to a military order and incident to a permanent change of station
- The moving expenses would qualify as a deduction if the employee didn’t get a reimbursement
Transition rule
There is a transition rule under the new law. Under this rule, certain payments or reimbursements aren’t subject to federal income or employment taxes. This includes amounts that:
- An employer pays a third party in 2018 for qualified moving services provided to an employee prior to 2018.
- An employer reimburses an employee in 2018 for qualified moving expenses incurred prior to 2018.
To qualify for the transition rule, the payments or reimbursements must be for qualified expenses which would have been deductible by the employee if the employee had directly paid them before Jan. 1, 2018. The employee must not have deducted them in 2017.
Corrections
Employers who have included amounts covered by the exception or the transition rule in individuals’ wages or compensation can take steps to correct taxable wages and employment taxes.
More information:
The changes to the tax treatment of moving expense reimbursements is one of many changes passed last year. For more information or help with these or other workforce, compensation and benefits concerns, contact the author.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of management focused employment, employee benefit and insurance, workforce and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Highly valued for her rare ability to find pragmatic client-centric solutions by combining her detailed legal and operational knowledge and experience with her talent for creative problem-solving, Ms. Stamer’s clients include employers and other workforce management organizations; employer, union, association, government and other insured and self-insured health and other employee benefit plan sponsors, benefit plans, fiduciaries, administrators, and other plan vendors; domestic and international public and private health care, education and other community service and care organizations; managed care organizations; insurers, third-party administrative services organizations and other payer organizations; and other private and government organizations and their management leaders.
Throughout her 30 plus year career, Ms. Stamer has continuously worked with these and other management clients to design, implement, document, administer and defend hiring, performance management, compensation, promotion, demotion, discipline, reduction in force and other workforce, employee benefit, insurance and risk management, health and safety, and other programs, products and solutions, and practices; establish and administer compliance and risk management policies; comply with requirements, investigate and respond to government, accreditation and quality organizations, regulatory and contractual audits, private litigation and other federal and state reviews, investigations and enforcement actions; evaluate and influence legislative and regulatory reforms and other regulatory and public policy advocacy; prepare and present training and discipline; handle workforce and related change management associated with mergers, acquisitions, reductions in force, re-engineering, and other change management; and a host of other workforce related concerns. Ms. Stamer’s experience in these matters includes supporting these organizations and their leaders on both a real-time, “on demand” basis with crisis preparedness, intervention and response as well as consulting and representing clients on ongoing compliance and risk management; plan and program design; vendor and employee credentialing, selection, contracting, performance management and other dealings; strategic planning; policy, program, product and services development and innovation; mergers, acquisitions, bankruptcy and other crisis and change management; management, and other opportunities and challenges arising in the course of workforce and other operations management to improve performance while managing workforce, compensation and benefits and other legal and operational liability and performance.
Past Chair of the ABA Managed Care & Insurance Interest Group and, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, heavily involved in health benefit, health care, health, financial and other information technology, data and related process and systems development, policy and operations throughout her career, and scribe of the ABA JCEB annual Office of Civil Rights agency meeting, Ms. Stamer also is widely recognized for her extensive work and leadership on leading edge health care and benefit policy and operational issues. She regularly helps employer and other health benefit plan sponsors and vendors, health industry, insurers, health IT, life sciences and other health and insurance industry clients design, document and enforce plans, practices, policies, systems and solutions; manage regulatory, contractual and other legal and operational compliance; vendors and suppliers; deal with Medicare, Medicaid, CHIP, Medicare/Medicaid Advantage, ERISA, state insurance law and other private payer rules and requirements; contracting; licensing; terms of participation; medical billing, reimbursement, claims administration and coordination, and other provider-payer relations; reporting and disclosure, government investigations and enforcement, privacy and data security; and other compliance and enforcement; Form 990 and other nonprofit and tax-exemption; fundraising, investors, joint venture, and other business partners; quality and other performance measurement, management, discipline and reporting; physician and other workforce recruiting, performance management, peer review and other investigations and discipline, wage and hour, payroll, gain-sharing and other pay-for performance and other compensation, training, outsourcing and other human resources and workforce matters; board, medical staff and other governance; strategic planning, process and quality improvement; HIPAA administrative simplification, meaningful use, EMR, HIPAA and other technology, data security and breach and other health IT and data; STARK, antikickback, insurance, and other fraud prevention, investigation, defense and enforcement; audits, investigations, and enforcement actions; trade secrets and other intellectual property; crisis preparedness and response; internal, government and third-party licensure, credentialing, accreditation, HCQIA, HEDIS and other peer review and quality reporting, audits, investigations, enforcement and defense; patient relations and care; internal controls and regulatory compliance; payer-provider, provider-provider, vendor, patient, governmental and community relations; facilities, practice, products and other sales, mergers, acquisitions and other business and commercial transactions; government procurement and contracting; grants; tax-exemption and not-for-profit; 1557 and other Civil Rights; privacy and data security; training; risk and change management; regulatory affairs and public policy; process, product and service improvement, development and innovation, and other legal and operational compliance and risk management, government and regulatory affairs and operations concerns.
A former lead consultant to the Government of Bolivia on its Pension Privatization Project with extensive domestic and international public policy concerns in pensions, healthcare, workforce, immigration, tax, education and other areas, Ms. Stamer has been extensively involved in U.S. federal, state and local health care and other legislative and regulatory reform impacting these concerns throughout her career. Her public policy and regulatory affairs experience encompasses advising and representing domestic and multinational private sector health, insurance, employee benefit, employer, staffing and other outsourced service providers, and other clients in dealings with Congress, state legislatures, and federal, state and local regulators and government entities, as well as providing advice and input to U.S. and foreign government leaders on these and other policy concerns.
Author of leading works on a multitude of labor and employment, compensation and benefits, internal controls and compliance, and risk management matters and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other related concerns by her service in the leadership of the Solutions Law Press, Inc. Coalition for Responsible Health Policy, its PROJECT COPE: Coalition on Patient Empowerment, and a broad range of other professional and civic organizations including North Texas Healthcare Compliance Association, a founding Board Member and past President of the Alliance for Healthcare Excellence, past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children (now Warren Center For Children); current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee, current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Section, a current Defined Contribution Plan Committee Co-Chair, former Group Chair and Co-Chair of the ABA RPTE Section Employee Benefits Group, past Representative and chair of various committees of ABA Joint Committee on Employee Benefits; an ABA Health Law Coordinating Council representative, former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, a former member of the Board of Directors of the Southwest Benefits Association and others.
For more information about Ms. Stamer or her health industry and other experience and involvements, see here or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here such as the following:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advise or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication or the topic of this article, please contact the author directly. All other rights reserved.
 Comments Off on Reminder To Report Moving Expense Reimbursements As Taxable Income |
Comments Off on Reminder To Report Moving Expense Reimbursements As Taxable Income |  compensation, compensation transparency, compliance, employee, Employee Benefits, Employee Handbook, Employer, Employers, Executive Compensation, Fringe Benefits, HR, Human Resources, Income Tax, Internal Revenue Code, IRC, Job, Labor Management Relations, Management, Managment, Moving expense reimbursement, Payroll Tax, Public Policy, TCJA Tax Reform, Technology, Uncategorized, Wage & Hour |
compensation, compensation transparency, compliance, employee, Employee Benefits, Employee Handbook, Employer, Employers, Executive Compensation, Fringe Benefits, HR, Human Resources, Income Tax, Internal Revenue Code, IRC, Job, Labor Management Relations, Management, Managment, Moving expense reimbursement, Payroll Tax, Public Policy, TCJA Tax Reform, Technology, Uncategorized, Wage & Hour |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
December 15, 2018
A ruling by a Federal District judge on Friday (December 14, 2018) ruled unconstitutional the Patient Protection and Affordable Care Act (ACA) touches off a new wave of uncertainty about the future of the massive healthcare reform law commonly known as Obamacare just as the enrollment period for 2019 health coverage ended. While Federal District Judge Reed O’Connor finds in his ruling released on Friday that amendments passed by Congress last December robbed the ACA of its original constitutionality, only time will tell if the ruling actually will end the ACA reforms or the effect of such ruling on the hotly debated ACA reforms and other statutory and regulatory reforms Congress and the Trump Administration subsequently prospectively or retrospectively. Consequently, health plans, their employer and other sponsors, insurers, administrators, and fiduciaries; health care providers, consumers and others will need to watch developments closely.
Justice O’Connor’s decision was released one day before the last day of the enrollment period for Americans to elect whether and what coverage, if any, to enroll in through the Obamacare exchanges for calendar 2019.
In Texas v. US, Texas Governor Greg Abbott and other Republican governors challenged the constitutionality of the ACA following passage of the Tax Cuts and Jobs Act of 2017 (TCJA). The plaintiffS argued the TCJA rendered the ACA unconstitutional because it repealed the individual mandate of the ACA upon which the Supreme Court previously found the ACA constitutional.
In the 2012 decision in Nat’l Fed’n of Indep. Businesses v. Sebelius (NFIB), 567 U.S. 519, 530–38 (2012) written by Chief Justice Roberts, the Supreme Court ruled that Congress could not rely upon the Commerce Clause for Constitutional authority to enact the ACA. However, the Supreme Court nevertheless found the Individual Mandate provisions of the ACA preserved the constitutionality of the ACA as a constitutional exercise of Congress’ Taxing Power.
In Texas v. US, the plaintiff governors argue that the repeal of the Individual Mandate as part of Congress’ passage of the TCJA last December robbed the ACA of its constitutionality. They say it is no longer fairly readable as an exercise of Congress’s Tax Power and continues to be unsustainable under the Interstate Commerce Clause. They further urge that if they are correct, the balance of the ACA is untenable as inseverable from the Invalid Mandate. Judge O’Connor agreed with the plaintiff’s in his ruling on Friday. Now it remains to be seen if his ruling will face and withstand the appeal and if so, what effect it will have on Obamacare overall and other subsequent statutory and regulatory reforms.
While only time will tell whether the decision stands and its effect, the path to clarity promises to be filled with more drama and uncertainty. Former US Attorney General Jeff Sessions previously had stated that the Justice Department under his leadership would not expend resources to defend the ACA. It remains to be seen how the Justice Department will not respond in light of his recent resignation. Even if the Justice Department does not step up to defend Obamacare, it is likely that states like California that have intervened in support of the ACA in the litigation will attempt to appeal the action. Assuming that an appeal proceeds, a Court of Appeals would hear the appeal before an almost certain appeal by the losing side in that appeal to the United States Supreme Court, where President Trump’s new appointee would hear the action. Along with the possibility that these Courts will uphold the trial court’s ruling, either of these appeals courts could overrule the trial court in whole or in part. Thus, subsequent appeals decisions could:
- Reverse Judge O’Connor’s ruling entirely, leaving The ACA intact in its current form; or
- Uphold part but not all of the decision, leaving some parts in place but not others.
pending further decisions, it remains unclear if subsidies, prohibitions against preexisting conditions, guaranteed issue, cost regulations, benefit and coverage mandates and other insurance reforms, health care billing and other reforms will survive.
Meanwhile, regardless of the outcome of the appeals, the decision and its fallout almost certainly will touch off more debate in Congress. With health care reform already a hot topic, more Congressional battles were inevitable. However the decision adds a new and significant wrinkle to the politics of the health reform fight.
In January November’s election will cause the leadership of the House of Representatives is set to transfer from Republicans to Democrats while leaving control over the Senate in the hands of Republications. With leadership of the two legislative bodies split, Democrats are unlikely to be able to use their new control of the House to enact legislation that would overrule outright an adverse decision by the courts. Consequently, Democrats will have an uphill battle if the court decision stands unless and until they can regain Senate control. Instead they are likely to be related to the role occupied by the House the past 4 years in which bills to enact the Democrat vision will pass the House only to die a quick death in the Republican controlled Senate or face veto by the Republican President.
On the other hand, Republicans also could not overcome a decision unfavorable to their agenda for the opposite reason: Despite control of the majority in the Senate and having a Republican President opposed to the ACA, Republicans can’t enact legislation without winning a majority of votes in the House.
On the other hand, either party can and almost certainly will use its veto power over the other party’s agenda. The fight likely will spill over into budget, immigration, workforce and other jet legislation that otherwise might and should enjoy bipartisan support in Congress.
As the litigation proceeds, concerned parties will want to keep a close eye of the Courts, the regulation and enforcement actions of the Trump Administration and the Congress.
Meanwhile, it is important to keep in mind that implementation of Judge O’Connor’s decision is stayed pending appeal.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of managed care and other health industry, health and other benefit and insurance, workforce and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Past Chair of the ABA Managed Care & Insurance Interest Group, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer is nationally recognized as a thoughtleader in health benefits and health care matters domestically and internationally. She has been continuously involved the design, regulation, administration and defense of managed care and other health and employee benefit, health care, human resources and other staffing and workforce arrangements, contracts, systems, and processes. As a continuous component of this work, Ms. Stamer has worked closely with these and other clients on the design, development, administration, defense, and breach and data recovery of health care, workforce, insurance and financial services, trade secret and other information technology, data and related process and systems development, policy and operations throughout her career.
Scribe of the ABA JCEB annual Office of Civil Rights agency meeting, Ms. Stamer also is widely recognized for her extensive work and leadership on leading edge health care and benefit policy and operational issues.
Ms. Stamer’s clients include employers and other workforce management organizations; employer, union, association, government and other insured and self-insured health and other employee benefit plan sponsors, benefit plans, fiduciaries, administrators, and other plan vendors; managed care organizations, insurers, self-insured health plans and other payers and their management; public and private, domestic and international hospitals, health care systems, clinics, skilled nursing, long-term care, rehabilitation and other health care providers and facilities; medical staff, health care accreditation, peer review and quality committees and organizations; managed care organizations, insurers, third-party administrative services organizations and other payer organizations; billing, utilization management, management services organizations; group purchasing organizations; pharmaceutical, pharmacy, and prescription benefit management and organizations; claims, billing and other health care and insurance technology and data service organizations; other health, employee benefit, insurance and financial services product and solutions consultants, developers and vendors; and other health, employee benefit, insurance, technology, government and other management clients.
A former lead consultant to the Government of Bolivia on its Pension Privatization Project with extensive domestic and international public policy concerns in pensions, healthcare, workforce, immigration, tax, education and other areas, Ms. Stamer has been extensively involved in U.S. federal, state and local health care and other legislative and regulatory reform impacting these concerns throughout her career. Her public policy and regulatory affairs experience encompasses advising and representing domestic and multinational private sector health, insurance, employee benefit, employer, staffing and other outsourced service providers, and other clients in dealings with Congress, state legislatures, and federal, state and local regulators and government entities, as well as providing advice and input to U.S. and foreign government leaders on these and other policy concerns.
Beyond her public policy and regulatory affairs involvement, Ms. Stamer also has extensive experience helping these and other clients to design, implement, document, administer and defend workforce, employee benefit, insurance and risk management, health and safety, and other programs, products and solutions, and practices; establish and administer compliance and risk management policies; comply with requirements, investigate and respond to government; accreditation and quality organizations; private litigation and other federal and state health care industry investigations and enforcement actions; evaluate and influence legislative and regulatory reforms and other regulatory and public policy advocacy; training and discipline; enforcement, and a host of other related concerns. Ms. Stamer’s experience in these matters includes supporting these organizations and their leaders on both a real-time, “on demand” basis with crisis preparedness, intervention and response as well as consulting and representing clients on ongoing compliance and risk management; plan and program design; vendor and employee credentialing, selection, contracting, performance management and other dealings; strategic planning; policy, program, product and services development and innovation; mergers, acquisitions, and change management; workforce and operations management, and other opportunities and challenges arising in the course of their operations.
Ms. Stamer also has extensive health care reimbursement and insurance experience advising and defending plan sponsors, administrators, insurance and managed care organizations, health care providers, payers, and others about Medicare, Medicaid, Medicare and Medicaid Advantage, Tri-Care, self-insured group, association, individual and employer and association group and other health benefit programs and coverages including but not limited to advising public and private payers about coverage and program design and documentation, advising and defending providers, payers and systems and billing services entities about systems and process design, audits, and other processes; provider credentialing, and contracting; providers and payer billing, reimbursement, claims audits, denials and appeals, coverage coordination, reporting, direct contracting, False Claims Act, Medicare & Medicaid, ERISA, state Prompt Pay, out-of-network and other nonpar insured, and other health care claims, prepayment, post-payment and other coverage, claims denials, appeals, billing and fraud investigations and actions and other reimbursement and payment related investigation, enforcement, litigation and actions. Scribe for the ABA JCEB annual agency meeting with HHS OCR, she also has worked extensively on health and health benefit coding, billing and claims, meaningful use and EMR, billing and reimbursement, quality measurement and reimbursement, HIPAA, FACTA, PCI, trade secret, physician and other medical, workforce, consumer financial and other data confidentiality and privacy, federal and state data security, data breach and mitigation, and other information privacy and data security concerns.
Author of leading works on a multitude of health care, health plan and other health industry matters, the American Bar Association (ABA) International Section Life Sciences Committee Vice Chair, a Scribe for the ABA Joint Committee on Employee Benefits (JCEB) Annual OCR Agency Meeting, former Vice President of the North Texas Health Care Compliance Professionals Association, past Chair of the ABA Health Law Section Managed Care & Insurance Section, past ABA JCEB Council Representative and CLE and Marketing Committee Chair, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, Ms. Stamer’s health industry clients include public health organizations; public and private hospitals, healthcare systems, clinics and other health care facilities; physicians, physician practices, medical staff, and other provider organizations; skilled nursing, long-term care, assisted living, home health, ambulatory surgery, dialysis, telemedicine, DME, Pharma, clinics, and other health care providers; billing, management and other administrative services organizations; insured, self-insured, association and other health plans; PPOs, HMOs and other managed care organizations, insurance, claims administration, utilization management, and other health care payers; public and private peer review, quality assurance, accreditation and licensing; technology and other outsourcing; healthcare clearinghouse and other data; research; public and private social and community organizations; real estate, technology, clinical pathways, and other developers; investors, banks and financial institutions; audit, accounting, law firm; consulting; document management and recordkeeping, business associates, vendors, and service providers and other professional and other health industry organizations; academic medicine; trade associations; legislative and other law making bodies and others.
A popular lecturer and widely published author on health industry concerns, Ms. Stamer continuously advises health industry clients about contracting, credentialing and quality assurance, compliance and internal controls, workforce and medical staff performance, quality, governance, reimbursement, privacy and data security, and other risk management and operational matters. Author of works on Payer and Provider Contracting and many other managed care concerns, Ms. Stamer also publishes and speaks extensively on health and managed care industry regulatory, staffing and human resources, compensation and benefits, technology, public policy, reimbursement and other operations and risk management concerns.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other related concerns by her service in the leadership of the Solutions Law Press, Inc. Coalition for Responsible Health Policy, its PROJECT COPE: Coalition on Patient Empowerment, and a broad range of other professional and civic organizations including North Texas Healthcare Compliance Association, a founding Board Member and past President of the Alliance for Healthcare Excellence, past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children (now Warren Center For Children); current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee, current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Section, a current Defined Contribution Plan Committee Co-Chair, former Group Chair and Co-Chair of the ABA RPTE Section Employee Benefits Group, past Representative and chair of various committees of ABA Joint Committee on Employee Benefits; an ABA Health Law Coordinating Council representative, former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, a former member of the Board of Directors of the Southwest Benefits Association and others.
For more information about Ms. Stamer or her health industry and other experience and involvements, see here or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here such as:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advise or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on Court Ruling Obamacare Unconstitutional Leaves Obamacare Future Uncertain As Annual Enrollment Period Ends |
Comments Off on Court Ruling Obamacare Unconstitutional Leaves Obamacare Future Uncertain As Annual Enrollment Period Ends |  4980D, 4980H, 5000, 6039D, ACA, Affordable Care Act, Association Health Plan, Claims, Claims Administration, compensation, compliance, Consumer Protection, Corporate Compliance, EBSA, Employee Benefits, Employer, Employers, EMR, ERISA, Fiduciary Responsibility, Form 5500, health benefit, Health Benefits, health Care, Health Care Reform, health insurance, health insurance marketplace, health plan, Health Plans, health reform, HIPAA, HR, HSA, Human Resources, Insurance, insurers, Managed Care, Managment, Medicare Part D, Mental Health, Mental Health Parity, MEWA, Obamacare, Patient Empowerment, Patient Protection & Affordable Care Act, Patient Protection and Affordabel Care Act, Patient Protection and Affordable Care Act, Physician, Plan Admistrator, PPO, Premium Subsidies, Prescription Drugs, preventive care, Protected Health Information, Provider, provider contracting, Reporting & Disclosure, Risk Management, SBC, Tax, Tax Credit, Tax Qualification, TCJA Tax Reform, third party administrators, Uncategorized, Wellness Programs, Worker Classification, Workers' Compensation, Workforce, zane benefits |
4980D, 4980H, 5000, 6039D, ACA, Affordable Care Act, Association Health Plan, Claims, Claims Administration, compensation, compliance, Consumer Protection, Corporate Compliance, EBSA, Employee Benefits, Employer, Employers, EMR, ERISA, Fiduciary Responsibility, Form 5500, health benefit, Health Benefits, health Care, Health Care Reform, health insurance, health insurance marketplace, health plan, Health Plans, health reform, HIPAA, HR, HSA, Human Resources, Insurance, insurers, Managed Care, Managment, Medicare Part D, Mental Health, Mental Health Parity, MEWA, Obamacare, Patient Empowerment, Patient Protection & Affordable Care Act, Patient Protection and Affordabel Care Act, Patient Protection and Affordable Care Act, Physician, Plan Admistrator, PPO, Premium Subsidies, Prescription Drugs, preventive care, Protected Health Information, Provider, provider contracting, Reporting & Disclosure, Risk Management, SBC, Tax, Tax Credit, Tax Qualification, TCJA Tax Reform, third party administrators, Uncategorized, Wellness Programs, Worker Classification, Workers' Compensation, Workforce, zane benefits |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
December 13, 2018
Employers should invite employees to update their Form W-4 withholding and finalize other 2019 payroll and income tax withholding arrangements based on guidance for 2019 published by the IRS and Treasury Department in Notice 2018-92 on November 26, 2018.
Many U.S. employers had delayed making changes to their income and payroll tax withholding pending the anticipated release by the IRS and Treasury Department of a revised Form W-4 and related income and payroll tax guidance updated to reflect changes to the Internal Revenue Code enacted as part of the Tax Cut and Jobs Act (P.L. 115-97)(“Trump Tax”) at the end of 2017.
Following the enactment of Trump Tax, most businesses have operated in reliance upon interim guidance published by the agencies at the beginning of the year to carryout their 2018 withholding obligations.
Until recently, the IRS and Treasury Department were expected to complete for use in 2019 the major overhaul of the Form W-4 and related guidance in response to the Trump Tax amendments to Sections 3402, 3405 and other Code rules. When the revision of the Form W-4 proved more complex than anticipated, however, the IRS and Treasury Department in September, 2018 announced that release of the newly designed and updated Form W-4 would be delayed from 2019 to 2020.
In Notice 2018-92, IRS and the Treasury Department provides interim guidance to employers and their workers on income tax withholding for 2019 pending agencies issuance of regulations implementing the changes, as well as requests comments on certain withholding procedures from concerned parties. For the most part, Notice 2018-92 continues the interim guidance that IRS and Treasury previously published for 2018. Specifically, Notice 2018-92:
- Announces that the 2019 Form W-4 will be similar to the 2018 Form W-4,
- Addresses new TCJA “withholding allowance” terminology,
- Continues until April 30, 2019 Notice 2018-14’s temporary suspension of the requirement to furnish new Forms W-4 within 10 days for changes resulting solely from the TCJA,
- Provides that, for 2019, the default rule when an employee fails to furnish a Form W-4 will continue to be single with zero withholding allowances,
- Allows taxpayers to take into account the qualified business income deduction under section 199A to reduce withholding under section 3402(m),
- Announces that the IRS and Treasury intend to update the regulations under section 3402 to explicitly allow taxpayers to use the online withholding calculator or Publication 505, Tax Withholding and Estimated Tax, in lieu of the worksheets to Form W-4,
- Requests comments on alternative withholding methods under section 3402(h),
- Announces that the IRS and the Treasury Department intend to eliminate the combined income tax withholding and employee FICA tax withholding tables under Treas. Reg. § 31.3402(h)(4)-1(b),
- Modifies notification requirements for the withholding compliance program, and
- Provides that for 2019, withholding on annuities or similar periodic payments where no withholding certificate is in effect is based on treating the payee as a married individual claiming 3 withholding allowances under § 3405(a)(4).
The Code generally requires employees that experience a change that reduces the number of withholding exemptions that the employee qualifies to claim to notify their employer and complete a new Form W-4 within 10 days of a specified event date. Interim relief published by the IRS and Treasury Department provides relief to workers whether the change in withholding eligibility results solely due to a Code change enacted as part of Trump Tax. Otherwise, however, employees generally still remain obligated to keep their withholding up-to-date. Since employees often are unaware of or overlook this responsibility, employers generally should encourage workers to review and update their Form W-4 withholding elections in connection with annual enrollment periods and in conjunction with other life or other changes likely to affect the withholding eligibility of the worker.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of management focused employment, employee benefit and insurance, workforce and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Highly valued for her rare ability to find pragmatic client-centric solutions by combining her detailed legal and operational knowledge and experience with her talent for creative problem-solving, Ms. Stamer’s clients include employers and other workforce management organizations; employer, union, association, government and other insured and self-insured health and other employee benefit plan sponsors, benefit plans, fiduciaries, administrators, and other plan vendors; domestic and international public and private health care, education and other community service and care organizations; managed care organizations; insurers, third-party administrative services organizations and other payer organizations; and other private and government organizations and their management leaders.
Throughout her 30 plus year career, Ms. Stamer has continuously worked with these and other management clients to design, implement, document, administer and defend hiring, performance management, compensation, promotion, demotion, discipline, reduction in force and other workforce, employee benefit, insurance and risk management, health and safety, and other programs, products and solutions, and practices; establish and administer compliance and risk management policies; comply with requirements, investigate and respond to government, accreditation and quality organizations, regulatory and contractual audits, private litigation and other federal and state reviews, investigations and enforcement actions; evaluate and influence legislative and regulatory reforms and other regulatory and public policy advocacy; prepare and present training and discipline; handle workforce and related change management associated with mergers, acquisitions, reductions in force, re-engineering, and other change management; and a host of other workforce related concerns. Ms. Stamer’s experience in these matters includes supporting these organizations and their leaders on both a real-time, “on demand” basis with crisis preparedness, intervention and response as well as consulting and representing clients on ongoing compliance and risk management; plan and program design; vendor and employee credentialing, selection, contracting, performance management and other dealings; strategic planning; policy, program, product and services development and innovation; mergers, acquisitions, bankruptcy and other crisis and change management; management, and other opportunities and challenges arising in the course of workforce and other operations management to improve performance while managing workforce, compensation and benefits and other legal and operational liability and performance.
Past Chair of the ABA Managed Care & Insurance Interest Group and, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, heavily involved in health benefit, health care, health, financial and other information technology, data and related process and systems development, policy and operations throughout her career, and scribe of the ABA JCEB annual Office of Civil Rights agency meeting, Ms. Stamer also is widely recognized for her extensive work and leadership on leading edge health care and benefit policy and operational issues. She regularly helps employer and other health benefit plan sponsors and vendors, health industry, insurers, health IT, life sciences and other health and insurance industry clients design, document and enforce plans, practices, policies, systems and solutions; manage regulatory, contractual and other legal and operational compliance; vendors and suppliers; deal with Medicare, Medicaid, CHIP, Medicare/Medicaid Advantage, ERISA, state insurance law and other private payer rules and requirements; contracting; licensing; terms of participation; medical billing, reimbursement, claims administration and coordination, and other provider-payer relations; reporting and disclosure, government investigations and enforcement, privacy and data security; and other compliance and enforcement; Form 990 and other nonprofit and tax-exemption; fundraising, investors, joint venture, and other business partners; quality and other performance measurement, management, discipline and reporting; physician and other workforce recruiting, performance management, peer review and other investigations and discipline, wage and hour, payroll, gain-sharing and other pay-for performance and other compensation, training, outsourcing and other human resources and workforce matters; board, medical staff and other governance; strategic planning, process and quality improvement; HIPAA administrative simplification, meaningful use, EMR, HIPAA and other technology, data security and breach and other health IT and data; STARK, antikickback, insurance, and other fraud prevention, investigation, defense and enforcement; audits, investigations, and enforcement actions; trade secrets and other intellectual property; crisis preparedness and response; internal, government and third-party licensure, credentialing, accreditation, HCQIA, HEDIS and other peer review and quality reporting, audits, investigations, enforcement and defense; patient relations and care; internal controls and regulatory compliance; payer-provider, provider-provider, vendor, patient, governmental and community relations; facilities, practice, products and other sales, mergers, acquisitions and other business and commercial transactions; government procurement and contracting; grants; tax-exemption and not-for-profit; 1557 and other Civil Rights; privacy and data security; training; risk and change management; regulatory affairs and public policy; process, product and service improvement, development and innovation, and other legal and operational compliance and risk management, government and regulatory affairs and operations concerns.
A former lead consultant to the Government of Bolivia on its Pension Privatization Project with extensive domestic and international public policy concerns in pensions, healthcare, workforce, immigration, tax, education and other areas, Ms. Stamer has been extensively involved in U.S. federal, state and local health care and other legislative and regulatory reform impacting these concerns throughout her career. Her public policy and regulatory affairs experience encompasses advising and representing domestic and multinational private sector health, insurance, employee benefit, employer, staffing and other outsourced service providers, and other clients in dealings with Congress, state legislatures, and federal, state and local regulators and government entities, as well as providing advice and input to U.S. and foreign government leaders on these and other policy concerns.
Author of leading works on a multitude of labor and employment, compensation and benefits, internal controls and compliance, and risk management matters and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other related concerns by her service in the leadership of the Solutions Law Press, Inc. Coalition for Responsible Health Policy, its PROJECT COPE: Coalition on Patient Empowerment, and a broad range of other professional and civic organizations including North Texas Healthcare Compliance Association, a founding Board Member and past President of the Alliance for Healthcare Excellence, past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children (now Warren Center For Children); current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee, current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Section, a current Defined Contribution Plan Committee Co-Chair, former Group Chair and Co-Chair of the ABA RPTE Section Employee Benefits Group, past Representative and chair of various committees of ABA Joint Committee on Employee Benefits; an ABA Health Law Coordinating Council representative, former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, a former member of the Board of Directors of the Southwest Benefits Association and others.
For more information about Ms. Stamer or her health industry and other experience and involvements, see here or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here such as the following:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advise or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication or the topic of this article, please contact the author directly. All other rights reserved.
 Comments Off on Finalize 2019 Withholding Prep In Light of Notice 2018-92 |
Comments Off on Finalize 2019 Withholding Prep In Light of Notice 2018-92 |  105(h), 401(k), 4980D, 4980H, 6039D, board of directors, Brokers, Cafeteria Plans, compensation, compliance, Corporate Compliance, corporate governance, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, directors, EBSA, employee, Employee Benefits, Employer, Employment, Employment Tax, Excise Tax, Executive Compensation, Fringe Benefit, Health Benefits, health insurance, HR, HSA, Human Resources, Income Tax, Payroll Tax, Tax Credit, Tax Qualification, TCJA Tax Reform, Uncategorized | Tagged: Tax, Withholding |
105(h), 401(k), 4980D, 4980H, 6039D, board of directors, Brokers, Cafeteria Plans, compensation, compliance, Corporate Compliance, corporate governance, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, directors, EBSA, employee, Employee Benefits, Employer, Employment, Employment Tax, Excise Tax, Executive Compensation, Fringe Benefit, Health Benefits, health insurance, HR, HSA, Human Resources, Income Tax, Payroll Tax, Tax Credit, Tax Qualification, TCJA Tax Reform, Uncategorized | Tagged: Tax, Withholding |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
December 7, 2018
The Internal Revenue Service is warning human resources and other business leaders about a growing wave of identity theft and W-2 scams targeting sensitive tax data employers collect on their employees. The warning highlights one of the many growing data breach exposures businesses must manage as identity thieves become ever more sophisticated.
Such data like Form W-2 data – is highly valued by identity thieves. While identity thieves use a variety of tactics to steal this information including hacking into the IRS’ own systems, the IRS this week is warning about one scheme that the IRS says has become one of the more dangerous email scams.
All employers are targets for the W-2 scam, according to the IRS.
Here’s how it works:
- These emails appear to be from an executive or organization leader to a payroll or human resources employee.
- The message usually starts with a simple greeting, like: “Hey, you in today?”
- By the end of the email exchange, all of an organization’s Forms W-2 for their employees may be in the hands of cybercriminals.
- Because payroll officials believe they are corresponding with an executive, it may take weeks for someone to realize a data theft has occurred.
- Generally, the criminals are trying to quickly take advantage of their theft, sometimes filing fraudulent tax returns a day or two.
The IRS warns this scam is such a threat to taxpayers that a special IRS reporting process has been established. The IRS says employers victimized should:
- Email dataloss@irs.gov to notify the IRS of a W-2 data loss and provide contact information. In the subject line, type “W2 Data Loss” so that the email can be routed properly. The business should not attach any employee personally identifiable information data.
- Email the Federation of Tax Administrators at StateAlert@taxadmin.org to get information on how to report victim information to the states.
- File a complaint with the FBI’s Internet Crime Complaint Center. Businesses and payroll service providers may be asked to file a report with their local law enforcement agency.
- Notify employees. The employee may then take steps to protect themselves from identity theft. The Federal Trade Commission’s www.identitytheft.govprovides guidance on general steps employees should take.
- Forward the scam email to phishing@irs.gov.
The IRS also recommends the following resources:
The IRS alert reminds businesses again about the growing challenges they face guarding sensitive tax, health and other employee benefit plan and other data about employees, customers, business partners and others. Aside from the disruptions businesses incur to organizations and relationships with employees, customers, business partners or others and often tremendous costs of investigation and mitigation, breaches also commonly trigger substantial legal liability under a myriad of federal and state laws and regulations, contracts, and common law tort claims. Businesses generally and Human Resources, tax and other systems and operations should take well documented steps to prevent and prepare for a potential breach.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of management focused employment, employee benefit and insurance, workforce and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Highly valued for her rare ability to find pragmatic client-centric solutions by combining her detailed legal and operational knowledge and experience with her talent for creative problem-solving and author of “What To Do When Your Employee’s Personal Life Becomes Your Business@ and a multitude of other highly regarded works on data protection and breach, her work includes career-long, leading edge involvement counseling and representing human resources, employee benefit, insurance and financial, tax, healthcare and other businesses about data and other sensitive information privacy and breach.
Ms. Stamer’s clients include employers and other workforce management organizations; employer, union, association, government and other insured and self-insured health and other employee benefit plan sponsors, benefit plans, fiduciaries, administrators, and other plan vendors; domestic and international public and private health care, education and other community service and care organizations; managed care organizations; insurers, third-party administrative services organizations and other payer organizations; and other private and government organizations and their management leaders.
Throughout her 30 plus year career, Ms. Stamer has continuously worked with these and other management clients to design, implement, document, administer and defend hiring, performance management, compensation, promotion, demotion, discipline, reduction in force and other workforce, employee benefit, insurance and risk management, health and safety, and other programs, products and solutions, and practices; establish and administer compliance and risk management policies; comply with requirements, investigate and respond to government, accreditation and quality organizations, regulatory and contractual audits, private litigation and other federal and state reviews, investigations and enforcement actions; evaluate and influence legislative and regulatory reforms and other regulatory and public policy advocacy; prepare and present training and discipline; handle workforce and related change management associated with mergers, acquisitions, reductions in force, re-engineering, and other change management; and a host of other workforce related concerns. Ms. Stamer’s experience in these matters includes supporting these organizations and their leaders on both a real-time, “on demand” basis with crisis preparedness, intervention and response as well as consulting and representing clients on ongoing compliance and risk management; plan and program design; vendor and employee credentialing, selection, contracting, performance management and other dealings; strategic planning; policy, program, product and services development and innovation; mergers, acquisitions, bankruptcy and other crisis and change management; management, and other opportunities and challenges arising in the course of workforce and other operations management to improve performance while managing workforce, compensation and benefits and other legal and operational liability and performance.
Past Chair of the ABA Managed Care & Insurance Interest Group and, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, heavily involved in health benefit, health care, health, financial and other information technology, data and related process and systems development, policy and operations throughout her career, and scribe of the ABA JCEB annual Office of Civil Rights agency meeting, Ms. Stamer also is widely recognized for her extensive work and leadership on leading edge health care and benefit policy and operational issues. She regularly helps employer and other health benefit plan sponsors and vendors, health industry, insurers, health IT, life sciences and other health and insurance industry clients design, document and enforce plans, practices, policies, systems and solutions; manage regulatory, contractual and other legal and operational compliance; vendors and suppliers; deal with Medicare, Medicaid, CHIP, Medicare/Medicaid Advantage, ERISA, state insurance law and other private payer rules and requirements; contracting; licensing; terms of participation; medical billing, reimbursement, claims administration and coordination, and other provider-payer relations; reporting and disclosure, government investigations and enforcement, privacy and data security; and other compliance and enforcement; Form 990 and other nonprofit and tax-exemption; fundraising, investors, joint venture, and other business partners; quality and other performance measurement, management, discipline and reporting; physician and other workforce recruiting, performance management, peer review and other investigations and discipline, wage and hour, payroll, gain-sharing and other pay-for performance and other compensation, training, outsourcing and other human resources and workforce matters; board, medical staff and other governance; strategic planning, process and quality improvement; HIPAA administrative simplification, meaningful use, EMR, HIPAA and other technology, data security and breach and other health IT and data; STARK, antikickback, insurance, and other fraud prevention, investigation, defense and enforcement; audits, investigations, and enforcement actions; trade secrets and other intellectual property; crisis preparedness and response; internal, government and third-party licensure, credentialing, accreditation, HCQIA, HEDIS and other peer review and quality reporting, audits, investigations, enforcement and defense; patient relations and care; internal controls and regulatory compliance; payer-provider, provider-provider, vendor, patient, governmental and community relations; facilities, practice, products and other sales, mergers, acquisitions and other business and commercial transactions; government procurement and contracting; grants; tax-exemption and not-for-profit; 1557 and other Civil Rights; privacy and data security; training; risk and change management; regulatory affairs and public policy; process, product and service improvement, development and innovation, and other legal and operational compliance and risk management, government and regulatory affairs and operations concerns.
A former lead consultant to the Government of Bolivia on its Pension Privatization Project with extensive domestic and international public policy concerns in pensions, healthcare, workforce, immigration, tax, education and other areas, Ms. Stamer has been extensively involved in U.S. federal, state and local health care and other legislative and regulatory reform impacting these concerns throughout her career. Her public policy and regulatory affairs experience encompasses advising and representing domestic and multinational private sector health, insurance, employee benefit, employer, staffing and other outsourced service providers, and other clients in dealings with Congress, state legislatures, and federal, state and local regulators and government entities, as well as providing advice and input to U.S. and foreign government leaders on these and other policy concerns.
Author of leading works on a multitude of labor and employment, compensation and benefits, internal controls and compliance, and risk management matters and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other related concerns by her service in the leadership of the Solutions Law Press, Inc. Coalition for Responsible Health Policy, its PROJECT COPE: Coalition on Patient Empowerment, and a broad range of other professional and civic organizations including North Texas Healthcare Compliance Association, a founding Board Member and past President of the Alliance for Healthcare Excellence, past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children (now Warren Center For Children); current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee, current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Section, a current Defined Contribution Plan Committee Co-Chair, former Group Chair and Co-Chair of the ABA RPTE Section Employee Benefits Group, past Representative and chair of various committees of ABA Joint Committee on Employee Benefits; an ABA Health Law Coordinating Council representative, former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, a former member of the Board of Directors of the Southwest Benefits Association and others.
For more information about Ms. Stamer or her health industry and other experience and involvements, see here or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here such as the following:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advise or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication or the topic of this article, please contact the author directly. All other rights reserved.
 Comments Off on Identity Theft Scan Targets Employee Tax Records |
Comments Off on Identity Theft Scan Targets Employee Tax Records |  ADA, Attorney-Client Privilege, Civil Rights, Claims Administration, Consumer Protection, Corporate Compliance, corporate governance, Cybercrime, Data Breach, Data Security, defined benefit plan, defined contribution plan, directors, Disability, Disability Plans, Discrimination, Educational Privacy, Employee Benefits, Employer, Employers, Employment, Employment Policies, Employment Tax, ERISA, fiduciary duty, Fiduciary Responsibility, Government Contractors, Identity Theft, Insurance, insurers, Non-Compete, Non-compete, Non-Competition Agreement, Protected Health Information, Retail, Tax, third party administrators, Trade secret, Uncategorized |
ADA, Attorney-Client Privilege, Civil Rights, Claims Administration, Consumer Protection, Corporate Compliance, corporate governance, Cybercrime, Data Breach, Data Security, defined benefit plan, defined contribution plan, directors, Disability, Disability Plans, Discrimination, Educational Privacy, Employee Benefits, Employer, Employers, Employment, Employment Policies, Employment Tax, ERISA, fiduciary duty, Fiduciary Responsibility, Government Contractors, Identity Theft, Insurance, insurers, Non-Compete, Non-compete, Non-Competition Agreement, Protected Health Information, Retail, Tax, third party administrators, Trade secret, Uncategorized |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
November 6, 2018
State and local political subdivisions employing fewer than 20 employees should reconfirm the defensibility of their employment policies and practices under the Age Discrimination and Employment Act (ADEA) and the Fair Labor Standards Act (FLSA) and various other laws in light of the unanimous[1] ruling issued this morning by the United State Supreme Court holding that the ADEA applies to all state and local political subdivisions regardless of size.
In its ruling in Mount Lemmon Fire District v. Guido, – U.S. -, 2018 WL 5794639 (November 6, 2018) released this morning, the United States Supreme Court unanimously ruled that the ADEA applies to all state and local subdivisions regardless of the number of employees the political subdivision employs.
The Supreme Court’s ruling arose from an ADEA lawsuit brought by John Guido and Dennis Rankin against a small Arizona fire department, the Mount Lemmon Fire District (District) challenging their layoff by the District. Faced with a budget shortfall, the District laid off Guido and Rankin, who at the time were the District’s two oldest full-time firefighters. Guido and Rankin sued the Fire District, alleging that their termination violated the Age Discrimination in Employment Act of 1967 (ADEA), 81 Stat. 602, as amended, 29 U. S. C. §621 et seq. The Fire District sought dismissal of the suit on the ground that the District was too small to qualify as an “employer” within the ADEA’s compass.
In response to Guido and Rankin’s lawsuit, the District asserted that was not covered by the ADEA because its employment of fewer than 20 employees rendered it “too small” to qualify as an “employer” as defined by 29 U. S. C. §630(b). In its ruling against the Fire District this morning, the Supreme Court rejected this numerosity defense, holding instead that the ADEA applies to all political subdivisions regardless of the size of their workforce.
In the unanimous opinion authored by Justice Ginsburg, the Supreme Court pointed out that the ADEA definition of “employer” distinguishes between private sector employers and State and local political subdivisions. The Supreme Court noted that before 1974, State and local political subdivisions were exempt from the ADEA. In 1974, however, Congress added a special definition of “employer” for States and political subdivisions to the ADEA and FLSA when it amended the ADEA and FLSA to apply to all State and local government employers regardless of their size. Thus, since 1974, the ADEA and FLSA definitions of “employer” have read as follows:
“The term ‘employer’ means a person engaged in an industry affecting commerce who has twenty or more employees . . . . The term also means (1) any agent of such a person, and (2) a State or political subdivision of a State . . . .” 29 U. S. C. §630(b); 29 U. S. C. §203(d), (x).
In construing this definition, the Supreme Court weighed whether the phrase “also means” added new categories to the definition of “employer” or merely clarified that States and their political subdivisions are a type of “person” included in §630(b)’s first sentence. While acknowledging that various Courts of Appeals previously have reached differing conclusions concerning the appropriate interpretation, the Supreme Court ruled that the phase “also means” added a new category to the definition of “employer” for purposes of the ADEA. Accordingly, the Supreme Court rejected the District’s claim that the ADEA definition of “employer” includes the requirement of employment of at least 20 employees applicable to the ADEA’s private sector definition of “employer. Accordingly, the Supreme Court unanimously ruled that the ADEA applies to all State and local political subdivisions.
In light of the Supreme Court’s ruling, any State or local subdivision that has operated in reliance upon the now discredited interpretations of the ADEA or FLSA definitions of “employer” as applicable only to State or local governmental entities employing at least 20 employees immediately should take all necessary corrective action to bring their policies into compliance with the ADEA and FLSA. These governmental entities also should seek the advice of qualified legal counsel about the advisability of taking any retrospective action to self-correct any potential past deficiencies in compliance, if any, for which the entity might bear potential liability to the extent that the applicable state of limitations has not run on those claims.
[1] Justice Kavanaugh did not join in the opinion as he took no part in the consideration or decision of the case.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of management focused employment, employee benefit and insurance, workforce and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Highly valued for her rare ability to find pragmatic client-centric solutions by combining her detailed legal and operational knowledge and experience with her talent for creative problem-solving, Ms. Stamer’s clients include employers and other workforce management organizations; employer, union, association, government and other insured and self-insured health and other employee benefit plan sponsors, benefit plans, fiduciaries, administrators, and other plan vendors; domestic and international public and private health care, education and other community service and care organizations; managed care organizations; insurers, third-party administrative services organizations and other payer organizations; and other private and government organizations and their management leaders.
Throughout her 30 plus year career, Ms. Stamer has continuously worked with these and other management clients to design, implement, document, administer and defend hiring, performance management, compensation, promotion, demotion, discipline, reduction in force and other workforce, employee benefit, insurance and risk management, health and safety, and other programs, products and solutions, and practices; establish and administer compliance and risk management policies; comply with requirements, investigate and respond to government, accreditation and quality organizations, regulatory and contractual audits, private litigation and other federal and state reviews, investigations and enforcement actions; evaluate and influence legislative and regulatory reforms and other regulatory and public policy advocacy; prepare and present training and discipline; handle workforce and related change management associated with mergers, acquisitions, reductions in force, re-engineering, and other change management; and a host of other workforce related concerns. Ms. Stamer’s experience in these matters includes supporting these organizations and their leaders on both a real-time, “on demand” basis with crisis preparedness, intervention and response as well as consulting and representing clients on ongoing compliance and risk management; plan and program design; vendor and employee credentialing, selection, contracting, performance management and other dealings; strategic planning; policy, program, product and services development and innovation; mergers, acquisitions, bankruptcy and other crisis and change management; management, and other opportunities and challenges arising in the course of workforce and other operations management to improve performance while managing workforce, compensation and benefits and other legal and operational liability and performance.
Past Chair of the ABA Managed Care & Insurance Interest Group and, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, heavily involved in health benefit, health care, health, financial and other information technology, data and related process and systems development, policy and operations throughout her career, and scribe of the ABA JCEB annual Office of Civil Rights agency meeting, Ms. Stamer also is widely recognized for her extensive work and leadership on leading edge health care and benefit policy and operational issues. She regularly helps employer and other health benefit plan sponsors and vendors, health industry, insurers, health IT, life sciences and other health and insurance industry clients design, document and enforce plans, practices, policies, systems and solutions; manage regulatory, contractual and other legal and operational compliance; vendors and suppliers; deal with Medicare, Medicaid, CHIP, Medicare/Medicaid Advantage, ERISA, state insurance law and other private payer rules and requirements; contracting; licensing; terms of participation; medical billing, reimbursement, claims administration and coordination, and other provider-payer relations; reporting and disclosure, government investigations and enforcement, privacy and data security; and other compliance and enforcement; Form 990 and other nonprofit and tax-exemption; fundraising, investors, joint venture, and other business partners; quality and other performance measurement, management, discipline and reporting; physician and other workforce recruiting, performance management, peer review and other investigations and discipline, wage and hour, payroll, gain-sharing and other pay-for performance and other compensation, training, outsourcing and other human resources and workforce matters; board, medical staff and other governance; strategic planning, process and quality improvement; HIPAA administrative simplification, meaningful use, EMR, HIPAA and other technology, data security and breach and other health IT and data; STARK, antikickback, insurance, and other fraud prevention, investigation, defense and enforcement; audits, investigations, and enforcement actions; trade secrets and other intellectual property; crisis preparedness and response; internal, government and third-party licensure, credentialing, accreditation, HCQIA, HEDIS and other peer review and quality reporting, audits, investigations, enforcement and defense; patient relations and care; internal controls and regulatory compliance; payer-provider, provider-provider, vendor, patient, governmental and community relations; facilities, practice, products and other sales, mergers, acquisitions and other business and commercial transactions; government procurement and contracting; grants; tax-exemption and not-for-profit; 1557 and other Civil Rights; privacy and data security; training; risk and change management; regulatory affairs and public policy; process, product and service improvement, development and innovation, and other legal and operational compliance and risk management, government and regulatory affairs and operations concerns.
A former lead consultant to the Government of Bolivia on its Pension Privatization Project with extensive domestic and international public policy concerns in pensions, healthcare, workforce, immigration, tax, education and other areas, Ms. Stamer has been extensively involved in U.S. federal, state and local health care and other legislative and regulatory reform impacting these concerns throughout her career. Her public policy and regulatory affairs experience encompasses advising and representing domestic and multinational private sector health, insurance, employee benefit, employer, staffing and other outsourced service providers, and other clients in dealings with Congress, state legislatures, and federal, state and local regulators and government entities, as well as providing advice and input to U.S. and foreign government leaders on these and other policy concerns.
Author of leading works on a multitude of labor and employment, compensation and benefits, internal controls and compliance, and risk management matters and a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other related concerns by her service in the leadership of the Solutions Law Press, Inc. Coalition for Responsible Health Policy, its PROJECT COPE: Coalition on Patient Empowerment, and a broad range of other professional and civic organizations including North Texas Healthcare Compliance Association, a founding Board Member and past President of the Alliance for Healthcare Excellence, past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children (now Warren Center For Children); current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee, current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Section, a current Defined Contribution Plan Committee Co-Chair, former Group Chair and Co-Chair of the ABA RPTE Section Employee Benefits Group, past Representative and chair of various committees of ABA Joint Committee on Employee Benefits; an ABA Health Law Coordinating Council representative, former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, a former member of the Board of Directors of the Southwest Benefits Association and others.
For more information about Ms. Stamer or her health industry and other experience and involvements, see here or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here such as the following:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advise or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication or the topic of this article, please contact the author directly. All other rights reserved.
 Comments Off on ADEA Age Discrimination Ban Applies To All State & Local Government Employers |
Comments Off on ADEA Age Discrimination Ban Applies To All State & Local Government Employers |  adea, Age Discrimination, board of directors, compliance, Corporate Compliance, corporate governance, directors, Discrimination, EBSA, Education, EEOC, employee, Employee Benefits, Employee Handbook, Employers, Employment, Employment Discrimination, Employment Policies, Exempt, Fair Labor Standards Act, FLSA, Government Accountability, government employer, government plan, HR, Human Resources, Insurance, Labor Management Relations, Leadership, Management, Managment, officers, Overtime, Restructuring, retirement plan, Retirement Plans, Retirements, Risk Management, Schools, Supreme Court, Uncategorized | Tagged: #agediscrimination, #mountlemmon #adea, #schooldistrict #publichospital #firedepartment #publicschool #university #publichealth, Mount Lemmon |
adea, Age Discrimination, board of directors, compliance, Corporate Compliance, corporate governance, directors, Discrimination, EBSA, Education, EEOC, employee, Employee Benefits, Employee Handbook, Employers, Employment, Employment Discrimination, Employment Policies, Exempt, Fair Labor Standards Act, FLSA, Government Accountability, government employer, government plan, HR, Human Resources, Insurance, Labor Management Relations, Leadership, Management, Managment, officers, Overtime, Restructuring, retirement plan, Retirement Plans, Retirements, Risk Management, Schools, Supreme Court, Uncategorized | Tagged: #agediscrimination, #mountlemmon #adea, #schooldistrict #publichospital #firedepartment #publicschool #university #publichealth, Mount Lemmon |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
September 12, 2018
On Thursday, August 13, the House Ways & Means Committee will hold hearings on retirement rule reforms intended to change multiemployer plan rules to make it easier for small businesses to offer and their employees and independent contractors to participate in retirement plans and provide retirement plan relief for participants proposed in the Family Savings Act of 2018, H.R. 6757.
Part of recently 3-bill tax package dubbed “Tax Reform 2.0” introduced on Monday, September 10, H.R. 6757 would remove certain regulatory barriers restricting the types of small-business employers who are permitted to band together to offer a retirement plan through a multiple employer plan (MEP).
H.R. 6757 also includes relief for certain plan participants. Among other things, it would:
- End required minimum distributions of funds from 401(k) plans and other retirement savings accounts for retirees with balances under $50,000; and
- Protect the ability of participants invested in lifetime income options through an employment-based retirement plan against losing these investment guarantees when their employer changes recordkeepers.
Sponsored by Rep. Mike Kelly (R-PA), and cosponsored by Rep. Paul Mitchell (R-MI), House Ways and Means Committee Chairman Kevin Brady (R-TX), and all other Ways and Means Committee Republicans, H.R. 6757, the bill enjoys strong support among House Republicans and President Trump.
House Ways and Means Committee Chair Kevin Brady expressed strong support for its reforms, saying: “We are creating financial security. The Family Savings Act focuses on helping families save more and earlier for the future by making it easier for businesses to offer retirement savings plans while ensuring workers can easily participate in these plans. This will help give our families the financial stability they need for whatever life throws their way.”
The Ways and Means Committee will address the H.R. 6757 proposals during its scheduled Tax Reform 2.0 markup on Thursday, September 13, 2018 at 10:00 a.m. in Room 1100 of the Longworth House Office Building. Use these links to read these bills:
About The Author
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation; Former Chair of the RPTE Employee Benefits and Compensation Committee, a current Co-Chair of the Committee, and the former Chair of its Welfare Benefit and its Defined Compensation Plan Committees and former RPTE Joint Committee on Employee Benefits Council (JCEB) Representative, Cynthia Marcotte Stamer is a Martindale-Hubble “AV-Preeminent” practicing attorney and management consultant, author, public policy advocate, author and lecturer repeatedly recognized for her 30 plus years’ of work and pragmatic thought leadership, publications and training on health, pension and other employee benefit, insurance, labor and employment, and health care fiduciary responsibility, payment, investment, contracting and other design, administration and compliance concerns as among the “Top Rated Labor & Employment Lawyers in Texas,” a “Legal Leader,” a “Top Woman Lawyer” and with other awards by LexisNexis® Martindale-Hubbell®; as among the “Best Lawyers In Dallas” for her work in the field of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, in International Who’s Who of Professionals and with numerous other awards and distinctions.
Highly valued for her ability to meld her extensive legal and industry knowledge and experience with her talents as an insightful innovator and pragmatic problem solver, Ms. Stamer advises, represents and defends employer, union, multi-employer, association and other employee benefit plan sponsors, insurers and managed care organizations, fiduciaries, plan administrators, technology and other service providers, government and community leaders and others about health and other employee benefit and insurance program and policy design and innovation, funding, documentation, administration, communication, data security and use, contracting, plan, public and regulatory reforms and enforcement, and other risk management, compliance and operations matters. Her experience encompasses leading and supporting the development and defense of innovative new policies, programs, practices and solutions; advising and representing clients on routine plan establishment, plan documentation and contract drafting and review, administration, change and other compliance and operations; crisis prevention and response, compliance and risk management audits and investigations, enforcement actions and other dealings with the US Congress, Departments of Labor, Treasury, Health & Human Services, Federal Trade Commission, Justice, Securities and Exchange Commission, Education and other federal agencies, state legislatures, attorneys general, insurance, labor, worker’s compensation, and other agencies and regulators, and various other foreign and domestic governmental bodies and agencies. She also provides strategic and other supports clients in defending litigation as lead strategy counsel, special counsel and as an expert witness. Alongside her extensive legal and operational experience, Ms. Stamer also is recognized for her work as a public and regulatory policy advocate and community leader with a gift for finding pragmatic solutions and helping to forge the common ground necessary to build consensus. Best known for her domestic public policy and community leadership on health care and insurance reform, Ms. Stamer’s lifelong public policy and community service involvement includes service as a lead consultant to the Government of Bolivia on its pension privatization project, as well as extensive legislative and regulatory reform, advocacy and input workforce, worker classification, employee benefit, public health and healthcare, social security and other disability and aging in place, education, migration reforms domestically and internationally throughout her adult life. In addition to her public and regulatory policy involvement, Ms. Stamer also contributes her service and leadership to a professional and civic organizations and efforts including her involvement as the Founder and Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE; Coalition on Patient Empowerment, a founding Board Member and past President of the Alliance for Healthcare Excellence; Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; Vice Chair, Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group; current Fiduciary Responsibility Committee Co-Chair and Membership Committee member of the ABA RPTE Section; former RPTE Employee Benefits and Other Compensation Group Chair, former Chair and Co-Chair of its Welfare Plans Committee, and Defined Contribution Plans Committee; former RPTE Representative to ABA Joint Committee on Employee Benefits Council; former RPTE Representative to the ABA Health Law Coordinating Counsel; former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, former Board Member, Continuing Education Chair and Treasurer of the Southwest Benefits Association; Vice President of the North Texas Healthcare Compliance Professionals Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; past Dallas World Affairs Council Board Member, and in leadership of many other professional, civic and community organizations. Ms. Stamer also is a highly popular lecturer, symposia chair and author, who publishes and speaks extensively on health and managed care industry, human resources, employment and other privacy, data security and other technology, regulatory and operational risk management for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, the Society of Professional Benefits Administrators, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients, serves on the faculty and planning committee of many workshops, seminars, and symposia, and on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Beyond these involvements, Ms. Stamer also is active in the leadership of a broad range of other public policy advocacy and other professional and civic organizations and involvements. Through these and other involvements, she helps develop and build solutions, build consensus, garner funding and other resources, manage compliance and other operations, and take other actions to identify promote tangible improvements in health care and other policy and operational areas.
Before founding her current law firm, Cynthia Marcotte Stamer, P.C., Ms. Stamer practiced law as a partner with several prominent national and international law firms for more than 10 years before founding Cynthia Marcotte Stamer, P.C. to practice her unique brand of “Solutions law™” and to devote more time to the pragmatic policy and system reform, community education and innovation, and other health system improvement efforts of her PROJECT COPE: the Coalition on Patient Empowerment initiative.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com such as the following
▪DOL Spending Reports Required As Taxpayer Tool Need Improvement
▪Check & Protect Health & Other Electronic Systems & Data Against New Security Threat
▪April 1 New Deadline To Update Benefit Plan Disability Determination Claims & Appeals Procesures; Hear More on 1/26
▪Arizona Proposal To Ban Sexual Harassment Confidentiality Agreements Sign Of Growing Employer Risks
▪$23M Penalty Small Part of 21st Century’s Data Breach Fallout; Offers Data Breach Lessons For Other Businesses
▪Take Care of Your Good People
▪Read Tax Cuts and Jobs Act Conference Report For Tax Reform From Source
▪Check How IRS 2018 Retirement & Saving Plan Limits and Amounts Cost Of Living Adjustments Impact Your HR & Retirement Plan Administration & Planning
▪IRS Prepares To Nail Employers Under Obamacare Mandate While Giving Some Individual Mandate Relief
▪Hiring & Retaining Workers Growing Business Challenge
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on House W&M Committee To Markup Retirement and Other “Tax Reform 2.0” Bills Thursday |
Comments Off on House W&M Committee To Markup Retirement and Other “Tax Reform 2.0” Bills Thursday |  401(k), Banking, Brokers, compensation, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, employee, Employee Benefits, Employer, Employers, Employment Policies, Employment Tax, ERISA, ESOP, Fiduciary Responsibility, Human Resources, Income Tax, multiple employer plan (Meps), Retirement Plans, Retirements, Tax, Tax Qualification, TCJA Tax Reform, Uncategorized |
401(k), Banking, Brokers, compensation, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, employee, Employee Benefits, Employer, Employers, Employment Policies, Employment Tax, ERISA, ESOP, Fiduciary Responsibility, Human Resources, Income Tax, multiple employer plan (Meps), Retirement Plans, Retirements, Tax, Tax Qualification, TCJA Tax Reform, Uncategorized |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
July 31, 2018
Employees should heed the warning provided by a federal grand jury’s indictment today charging a Walled Lake, Michigan restaurant owner with 24 counts of failing to account for and pay over employment taxes and one count of willful failure to file an income tax return, announced Principal Deputy Assistant Attorney General Richard E. Zuckerman of the Justice Department’s Tax Division.
According to the indictment, Johni Semma owned Bayside Sports Bar & Grill (“Bayside”), a restaurant, and The Coliseum, an adult entertainment business. As the owner of Bayside, Semma was allegedly responsible for collecting and paying over Bayside’s employment taxes. The indictment charges that during 2008 to 2015, Bayside accrued employment tax liabilities of more than $1 million and that Semma withheld those taxes from the pay of the restaurant’s employees. Semma then allegedly failed to fully pay over the amounts he withheld to the Internal Revenue Service (IRS).
The indictment further alleges that in 2012, Semma sold The Coliseum for more than $6 million with approximately $3.5 million of the purchase price paid during 2012. Despite receiving considerable income from the sale of The Coliseum and other sources, Semma allegedly did not file a 2012 income tax return.
If convicted, Semma faces a statutory maximum of five years in prison for each count of failure to pay over the employment taxes. He faces a statutory maximum of one year in prison for the one count of willful failure to file his income tax return. In addition, he faces a period of supervised release, restitution, and monetary penalties. An indictment is an accusation. A defendant is presumed innocent unless and until proven guilty.
Employers should recognize the indictment as a reminder to ensure they timely collect and deposit all employment taxes withheld in accordance with applicable law.
About The Author
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation; Former Chair of the RPTE Employee Benefits and Compensation Committee, a current Co-Chair of the Committee, and the former Chair of its Welfare Benefit and its Defined Compensation Plan Committees and former RPTE Joint Committee on Employee Benefits Council (JCEB) Representative, Cynthia Marcotte Stamer is a Martindale-Hubble “AV-Preeminent” practicing attorney and management consultant, author, public policy advocate, author and lecturer repeatedly recognized for her 30 plus years’ of work and pragmatic thought leadership, publications and training on health, pension and other employee benefit, insurance, labor and employment, and health care fiduciary responsibility, payment, investment, contracting and other design, administration and compliance concerns as among the “Top Rated Labor & Employment Lawyers in Texas,” a “Legal Leader,” a “Top Woman Lawyer” and with other awards by LexisNexis® Martindale-Hubbell®; as among the “Best Lawyers In Dallas” for her work in the field of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, in International Who’s Who of Professionals and with numerous other awards and distinctions.
Highly valued for her ability to meld her extensive legal and industry knowledge and experience with her talents as an insightful innovator and pragmatic problem solver, Ms. Stamer advises, represents and defends employer, union, multi-employer, association and other employee benefit plan sponsors, insurers and managed care organizations, fiduciaries, plan administrators, technology and other service providers, government and community leaders and others about health and other employee benefit and insurance program and policy design and innovation, funding, documentation, administration, communication, data security and use, contracting, plan, public and regulatory reforms and enforcement, and other risk management, compliance and operations matters. Her experience encompasses leading and supporting the development and defense of innovative new policies, programs, practices and solutions; advising and representing clients on routine plan establishment, plan documentation and contract drafting and review, administration, change and other compliance and operations; crisis prevention and response, compliance and risk management audits and investigations, enforcement actions and other dealings with the US Congress, Departments of Labor, Treasury, Health & Human Services, Federal Trade Commission, Justice, Securities and Exchange Commission, Education and other federal agencies, state legislatures, attorneys general, insurance, labor, worker’s compensation, and other agencies and regulators, and various other foreign and domestic governmental bodies and agencies. She also provides strategic and other supports clients in defending litigation as lead strategy counsel, special counsel and as an expert witness. Alongside her extensive legal and operational experience, Ms. Stamer also is recognized for her work as a public and regulatory policy advocate and community leader with a gift for finding pragmatic solutions and helping to forge the common ground necessary to build consensus. Best known for her domestic public policy and community leadership on health care and insurance reform, Ms. Stamer’s lifelong public policy and community service involvement includes service as a lead consultant to the Government of Bolivia on its pension privatization project, as well as extensive legislative and regulatory reform, advocacy and input workforce, worker classification, employee benefit, public health and healthcare, social security and other disability and aging in place, education, migration reforms domestically and internationally throughout her adult life. In addition to her public and regulatory policy involvement, Ms. Stamer also contributes her service and leadership to a professional and civic organizations and efforts including her involvement as the Founder and Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE; Coalition on Patient Empowerment, a founding Board Member and past President of the Alliance for Healthcare Excellence; Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; Vice Chair, Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group; current Fiduciary Responsibility Committee Co-Chair and Membership Committee member of the ABA RPTE Section; former RPTE Employee Benefits and Other Compensation Group Chair, former Chair and Co-Chair of its Welfare Plans Committee, and Defined Contribution Plans Committee; former RPTE Representative to ABA Joint Committee on Employee Benefits Council; former RPTE Representative to the ABA Health Law Coordinating Counsel; former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, former Board Member, Continuing Education Chair and Treasurer of the Southwest Benefits Association; Vice President of the North Texas Healthcare Compliance Professionals Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; past Dallas World Affairs Council Board Member, and in leadership of many other professional, civic and community organizations. Ms. Stamer also is a highly popular lecturer, symposia chair and author, who publishes and speaks extensively on health and managed care industry, human resources, employment and other privacy, data security and other technology, regulatory and operational risk management for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, the Society of Professional Benefits Administrators, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients, serves on the faculty and planning committee of many workshops, seminars, and symposia, and on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Beyond these involvements, Ms. Stamer also is active in the leadership of a broad range of other public policy advocacy and other professional and civic organizations and involvements. Through these and other involvements, she helps develop and build solutions, build consensus, garner funding and other resources, manage compliance and other operations, and take other actions to identify promote tangible improvements in health care and other policy and operational areas.
Before founding her current law firm, Cynthia Marcotte Stamer, P.C., Ms. Stamer practiced law as a partner with several prominent national and international law firms for more than 10 years before founding Cynthia Marcotte Stamer, P.C. to practice her unique brand of “Solutions law™” and to devote more time to the pragmatic policy and system reform, community education and innovation, and other health system improvement efforts of her PROJECT COPE: the Coalition on Patient Empowerment initiative.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com such as the following
▪DOL Spending Reports Required As Taxpayer Tool Need Improvement
▪Check & Protect Health & Other Electronic Systems & Data Against New Security Threat
▪April 1 New Deadline To Update Benefit Plan Disability Determination Claims & Appeals Procesures; Hear More on 1/26
▪Arizona Proposal To Ban Sexual Harassment Confidentiality Agreements Sign Of Growing Employer Risks
▪$23M Penalty Small Part of 21st Century’s Data Breach Fallout; Offers Data Breach Lessons For Other Businesses
▪Take Care of Your Good People
▪Read Tax Cuts and Jobs Act Conference Report For Tax Reform From Source
▪Check How IRS 2018 Retirement & Saving Plan Limits and Amounts Cost Of Living Adjustments Impact Your HR & Retirement Plan Administration & Planning
▪IRS Prepares To Nail Employers Under Obamacare Mandate While Giving Some Individual Mandate Relief
▪Hiring & Retaining Workers Growing Business Challenge
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on Employer’s Employment Tax Fraud Indictment Warns Employers To Properly Pay Withheld Employment Taxes |
Comments Off on Employer’s Employment Tax Fraud Indictment Warns Employers To Properly Pay Withheld Employment Taxes |  4980D, 4980H, 5000, 6039D, ACA, board of directors, Brokers, compensation, compliance, Corporate Compliance, corporate governance, directors, employee, Employee Benefits, Employer, Employers, Employment, Employment Tax, Executive Compensation, Uncategorized, Unemployment Benefits, Unemployment Insurance, Wage & Hour, Whistleblower |
4980D, 4980H, 5000, 6039D, ACA, board of directors, Brokers, compensation, compliance, Corporate Compliance, corporate governance, directors, employee, Employee Benefits, Employer, Employers, Employment, Employment Tax, Executive Compensation, Uncategorized, Unemployment Benefits, Unemployment Insurance, Wage & Hour, Whistleblower |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
July 14, 2018
A flurry of activity in the House Ways & Means Committee and other Congressional committees over the past few weeks signals the advisability of keeping a close eye on health care and health benefit reform proposals this Summer in anticipation of both the Fall health benefit enrollment and renewal season and the mid-term November Congressional elections.
Coupled with the Trump Administration’s recent rollout of its long promised association health plan, short-term coverage and other regulatory reforms and promises of more changes to come, the ongoing attention paid by the Administration and Congress to health insurance and health care reform raises a strong possibility that employer, association, and other health plan sponsors, fiduciaries and their vendors that they and their plan members should be on watch for late-breaking developments that may require or warrant last minute changes to health benefit plan designs, communications, contracts or other key decisions.
With President Trump continuing to push for a wide range of health care reforms and health care and health benefit issues recognized as key voter concerns for the upcoming mid-term elections in November, the continued emphasis of the Republican-led Congress and federal regulators talking about their health care reform legislative agenda is not surprising. What may be more surprising to many is the intensity of the ongoing efforts in Congress to try to pass reform over the summer when many members of the House and Senate face tightly contested races in November.
Certainly continued Congressional commitment to pursue reform is evident from the House Ways & Means Committee’s health care heavy agenda of hearings and votes that this week alone resulted in its voting in favor of 11 health care reform bills promising new flexibility for employers about how to design their health plans and American families more health care choices and choice about how to pay for it and what coverage to buy popular with many providers, patients and employer and other health plan sponsors. While it remains to be seen if the House and Senate can agree on any or all of these proposal, the bi-partisan sponsorship of many of these proposals and the intensity of the focus of the Committee and others in Congress reflects a strong interest in health care reform by both parties leading up to November that could impact health benefit and other health care choices for providers, employers and American families in the Fall annual enrollment season.
The legislation passed by the Ways & Means Committee this weeks include bills that would:
- Provide relief for employers relief from the Obamacare’s employer mandate and delay for an additional year the effective date of the widely disliked “Cadillac Tax;”
- Overrule the “Use it Or Lose It” requirement in current Internal Revenue Regulations for healthcare flexible spending arrangement plans (HFSAs) that currently forces employers sponsoring HFSAs to draft their plans to require employees to forfeit unused salary reduction contributions in their HFSA accounts at the end of the year;
- Offer individuals and families eligible for Obamacare created health premium subsidies more choice about where to obtain that coverage using their subsidies; and
- Expand expand the availability and usability of HSAs in a multitude of ways.
Furthermore, a review of the Committee’s schedule makes clear that it isn’t finished with health care reform. After holding hearings on health savings account reforms and passing a flurry of health care reform bills intended to give employers relief from two key Obamacare mandates, to allow Obamacare subsidy-eligible Americans the choice to use the subsidies to purchase health care coverage not offered by the Obamacare exchanges, and a host of bills that would expand availability and usability of health savings account (HSA) and health care flexible spending account (HFSA) programs this week, the House Ways and Means Committee will turn its attention to health care fraud oversight and reform next week by holding hearings Tuesday on those health concerns. Health care providers, employer and other health plan sponsors, individual Americans and their families, and others interested in health benefit and health care reform will want to keep a close eye on these and other developments as Congress continues to debate health care reform in the runup to the upcoming 2018 health benefit plan renewal and annual enrollment season and November’s mid-term elections.
Committee Approved 11 Health Care Reform Bills This Week
As a part of its health reform efforts this week, the Committee voted to advance 11 health care reform bills offering new flexibility for employers about how to design their health plans and American families more health care choices and choice about how to pay for it and what coverage to buy popular with many providers, patients and employer and other health plan sponsors.
Among the approved legislation is a bill that would provide key relief for employers from certain key Obamacare mandates that have been widely unpopular with employers. H.R. 4616, the “Employer Relief Act of 2018,” sponsored by Rep. Devin Nunes (R-CA) and Rep. Mike Kelly (R-PA), which would give employers sponsoring health plans for their employees retroactive relief from Obamacare’s onerous employer mandate and delay for an additional year the effective date of another Obamacare requirement that when effective, will forces employers to pay the 40 percent tax on amounts paid for employer sponsored health care coverage that exceeds cost limits specified in the Obamacare legislation commonly known as the “Cadillac Tax.” Relief from the Cadillac Tax is widely perceived as benefiting bother employers and their employees, as its provisions penalize employers for spending more for employee health coverage than limits specified in the Obamacare law. These provisions also are particularly viewed by many as unfair because rising health plan costs since Obamacare’s passage make it likely that many employers will incur the tax penalty simply by sponsoring relatively basic health plans meeting the Obamacare mandates.
In addition to H.R. 4616, the Committee also voted to approve H.R. 6313, the “Responsible Additions and Increases to Sustain Employee Health Benefits Act of 2018,” sponsored by Rep. Steve Stivers (R-OH), which would overrule the “Use it Or Lose It” requirement in current Internal Revenue Regulations for HFSAs. Currently, this rule forces employers sponsoring HFSAs to draft their plans to require employees to forfeit unused salary reduction contributions in their HFSA accounts at the end of the year. The bill would allow employers to eliminate this forfeiture requirement so that employees could carry over any remaining unused balances in their HFSAs at the end of the year to use in a later year.
The Committee also voted to advance legislation to offer individuals and families eligible for Obamacare created health premium subsidies more choice about where to obtain that coverage. H.R. 6311, the “Increasing Access to Lower Premium Plans Act of 2018,” sponsored by Chairman Peter Roskam (R-IL) and Rep. Michael C. Burgess, M.D. (R-TX), would provide individuals receiving subsidies to help purchase health care coverage through the Obamacare-created health insurance exchange the option to use their premium tax credit to purchase health care coverage from qualified plans offered outside of the exchanges. Currently, subsidies may only be used to purchase coverage from health plans offered through the exchange, which often are much more costly and offer substantially fewer coverage options and less provider choice. In addition, the bill would expand access to the lowest-premium plans available for all individuals purchasing coverage in the individual market and allows the premium tax credit to be used to offset the cost of such plans.
Along with these reforms, the Committee also voted to pass a host of bills that would expand the availability and usability of HSAs including:
- H.R. 6301, the “Promoting High-Value Health Care Through Flexibility for High Deductible Health Plans Act of 2018,” co-sponsored by Health Subcommittee Chairman Peter Roskam (R-IL) and Rep. Mike Thompson (D-CA), which seeks to expand access and enhance the utility of Health Savings Accounts (HSAs) by offering patients greater flexibility in designing their plan design while still being able to maintain their eligibility for HSA contributions.
- H.R. 6305, the “Bipartisan HSA Improvement Act of 2018,” sponsored by Rep. Mike Kelly (R-PA) and Rep. Earl Blumenauer (D-OR), which also would expand HSA access and utility by allowing spouses to also make contributions to HSAs is their spouse has an FSA and lets employers offer certain services to employees through on-site or retail clinics.
- H.R. 6317, the “Primary Care Enhancement Act of 2018,” co-sponsored by Rep. Erik Paulsen (R-MN) and Rep. Earl Blumenauer (D-OR), which seeks to protect HSA-eligible individuals who participate in a direct primary care (DPC) arrangement from losing their HSA-eligibility merely because of their participation in a DPC. In addition, it allows DPC provider fees to be covered with HSAs.
- H.R. 6312, the “Personal Health Investment Today (PHIT) Act,” sponsored by Rep. Jason Smith (R-MO) and Rep. Ron Kind (D-WI), which seeks to fight obesity and promote wellness by allowing taxpayers to use tax-preferred accounts to pay costs of gym membership or exercise classes, children’s school sports programs and certain other wellness programs and activities.
- H.R. 6309, the “Allowing Working Seniors to Keep Their Health Savings Accounts Act of 2018,” sponsored by Rep. Erik Paulsen (R-MN), which would expand HSA eligibility to include Medicare eligible seniors who are still in the workforce.
- H.R.6199, the “Restoring Access to Medication Act of 2018,” sponsored by Rep. Lynn Jenkins (R-KS) and Rep. Grace Meng (D-NY), which would reverse Obamacare’s prohibition on using tax-favored health accounts to purchase over-the-counter medical products and would add feminine products to the list of qualified medical expenses for the purposes of these tax-favored health accounts.
- H.R. 6306, the “Improve the Rules with Respect to Health Savings Accounts,” sponsored by Rep. Erik Paulsen (R-MN), which would increase the contribution limits for HSAs and further enhances flexibility in plans by allowing both spouses to contribute to make catch-up contributions to the same account and creating a new grace period for medical expenses incurred before the HSA was established.
- H.R. 6314, the “Health Savings Act of 2018,” sponsored by Rep. Burgess (R-TX) and Rep. Roskam (R-IL), would expand eligibility and access to HSAs by allowing plans categorized as “catastrophic” and “bronze” in the exchanges to qualify for HSA contributions.
Committee Considers Health Care Fraud Next Week
The Committee next week will turn its attention to health care fraud by holding two hearings on Tuesday.
Both hearings are scheduled to take place in Room 1100 Longworth and their proceedings will be live streamed on YouTube.
The Committee’s health care reform focus this week and next are reflective of the continued emphasis of members of Congress in both parties on health care reform legislation as they prepare for the impending mid-term elections in November. As a part of these efforts, the House and Senate already over the past several months have held a wide range of hearings in various committees and key votes on a multitude of reform proposals. Numerous other hearings and votes are planned over the next several months as Congressional leaders from both parties work to advance their health care agendas in anticipation of the upcoming elections.
Key health care and health benefit reform proposals that the Republican Majority has designated for priority consideration include:
- Prescription drug costs by checking perceived negative effects of health industry and health plan consolidations involving large health insurers, pharmacy benefit management companies (PBMs), pharmacy companies and other health industry and health insurance organizations on health care costs and patient, plan sponsor and plan sponsor choice and health care quality;
- Oversight and reform of existing STARK, anti-kickback and other federal health care rules and exemptions relied upon by PBMs and other health industry organizations;
- Efforts to understand and address health care treatment, health care and coverage costs and related social concerns associated with mental health and opioid and other substance abuse conditions and their treatment;
- Efforts promote health benefit and health care choice, affordability and coverage; improve patient and employer choice; promote broader health care access and quality; reduce counterproductive regulation; and other health insurance and care improvements through expanded availability of health savings accounts, direct primary care and other consumer directed health care options, association health plan and other program options, streamlining quality reporting and regulation, billing and coding, physician and other health care provider electronic billing and recordkeeping, and other provider, payer, employer, individual and other health insurance mandates and other federal health care and health plan rules; and
- More.
Evolving Legislative & Regulatory Warrant Vigilance & Change Readiness
While the recurrent stalling of past reform efforts over the past few years calls into question whether any or all of these proposals can make it through the highly politicized and divided Congress, bi-partisian sponsorship of most of the bills reported out this week at least raises the possibility that some of these proposals enjoy sufficient bi-partisan support to potentially pass before the elections. With both parties viewing health care reform as a key issue in the upcoming elections, voter feedback on these proposals could play a big role in determining the prospects for passage this Summer.
Along with the ongoing Congressional reform efforts, the Trump Administration also continues to move forward on a series of regulatory reforms that also could impact health care and health benefit decisions and responsibilities later this year. Beyond the Administration’s implementation of its long promised and recently finalized and released association health plan, short term coverage and other health benefit rules, the Administration’s continued consideration of changes to essential health benefits and other Obamacare regulations, ongoing mental health, substance abuse, and prescription drug reform projects, and other proposed regulatory and enforcement changes are likely to require health plans, their sponsors, insurers, administrators, members and even providers to adapt to changes in federal health plan rules between now and year end.
Amid this shifting legal landscape, employer and other health plan sponsors, their insurers, vendors, providers and participants will want to remain vigilant and work to preserve the flexibility to respond to new rules or guidance likely to rollout over the next several months.
Staying on top of proposed reforms as the Summer progresses is important:
- To provide timely input to Congress on proposed reforms of particular benefit or concern;
- To help plan for and deal with rules changes that could impact their options and choices during the upcoming health plan renewal and enrollment season this Fall and going forward; and
- To be prepared to make informed choices when voting in the upcoming mid-term Congressional elections in November.
Keeping informed about potential changes is only part of the challenge, however. Employer and other health plan sponsors, fiduciaries and service providers also generally should seek to negotiate vendor contracts that allow them the greatest possible flexibility to respond to changing rules, opportunities and requirements with minimum penalties and disruption when designing, negotiating and implementing vendor contracts, plan designs and plan enrollment and other processes and communications.
About the Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for 30+ years of health industry, health and other benefit and insurance, workforce and other management work, public policy leadership and advocacy, coaching, teachings, and publications.
Highly valued for her rare ability to find pragmatic client-centric solutions by combining her detailed legal and operational knowledge and experience with her talent for creative problem-solving, Ms. Stamer’s clients include employers and other workforce management organizations; employer, union, association, government and other insured and self-insured health and other employee benefit plan sponsors, benefit plans, fiduciaries, administrators, and other plan vendors; managed care organizations, insurers, self-insured health plans and other payers and their management; public and private, domestic and international hospitals, health care systems, clinics, skilled nursing, long term care, rehabilitation and other health care providers and facilities; medical staff, health care accreditation, peer review and quality committees and organizations; managed care organizations, insurers, third party administrative services organizations and other payer organizations; billing, utilization management, management services organizations; group purchasing organizations; pharmaceutical, pharmacy, and prescription benefit management and organizations; claims, billing and other health care and insurance technology and data service organizations; other health, employee benefit, insurance and financial services product and solutions consultants, developers and vendors; and other health, employee benefit, insurance, technology, government and other management clients.
A former lead consultant to the Government of Bolivia on its Pension Privatization Project with extensive domestic and international public policy concerns in pensions, healthcare, workforce, immigration, tax, education and other areas, Ms. Stamer has been extensively involved in U.S. federal, state and local health care and other legislative and regulatory reform impacting these concerns throughout her career. Her public policy and regulatory affairs experience encompassess advising and representing domestic and multinational private sector health, insurance, employee benefit, employer, staffing and other outsourced service providers, and other clients in dealings with Congress, state legislatures, and federal, state and local regulators and government entities, as well as providing advice and input to U.S. and foreign government leaders on these and other policy concerns.
Beyond her public policy and regulatory affairs involvement, Ms. Stamer also has extensive experience helping these and other clients to design, implement, document, administer and defend workforce, employee benefit, insurance and risk management, health and safety, and other programs, products and solutions, and practices; establish and administer compliance and risk management policies; comply with requirements, investigate and respond to government; accreditation and quality organizations; private litigation and other federal and state health care industry investigations and enforcement actions; evaluate and influence legislative and regulatory reforms and other regulatory and public policy advocacy; training and discipline; enforcement, and a host of other related concerns. Ms. Stamer’s experience in these matters includes supporting these organizations and their leaders on both a real-time, “on demand” basis with crisis preparedness, intervention and response as well as consulting and representing clients on ongoing compliance and risk management; plan and program design; vendor and employee credentialing, selection, contracting, performance management and other dealings; strategic planning; policy, program, product and services development and innovation; mergers, acquisitions, and change management; workforce and operations management, and other opportunities and challenges arising in the course of their operations.
Past Chair of the ABA Managed Care & Insurance Interest Group and, a Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, heavily involved in health benefit, health care, health, financial and other information technology, data and related process and systems development, policy and operations throughout her career, and scribe of the ABA JCEB annual Office of Civil Rights agency meeting, Ms. Stamer also is widely recognized for her extensive work and leadership on leading edge health care and benefit policy and operational issues. She regularly helps employer and other health benefit plan sponsors and vendors, health industry, insurers, health IT, life sciences and other health and insurance industry clients design, document and enforce plans, practices, policies, systems and solutions; manage regulatory, contractual and other legal and operational compliance; vendors and suppliers; deal with Medicare, Medicaid, CHIP, Medicare/Medicaid Advantage, ERISA, state insurance law and other private payer rules and requirements; contracting; licensing; terms of participation; medical billing, reimbursement, claims administration and coordination, and other provider-payer relations; reporting and disclosure, government investigations and enforcement, privacy and data security; and other compliance and enforcement; Form 990 and other nonprofit and tax-exemption; fundraising, investors, joint venture, and other business partners; quality and other performance measurement, management, discipline and reporting; physician and other workforce recruiting, performance management, peer review and other investigations and discipline, wage and hour, payroll, gain-sharing and other pay-for performance and other compensation, training, outsourcing and other human resources and workforce matters; board, medical staff and other governance; strategic planning, process and quality improvement; HIPAA administrative simplification, meaningful use, EMR, HIPAA and other technology, data security and breach and other health IT and data; STARK, antikickback, insurance, and other fraud prevention, investigation, defense and enforcement; audits, investigations, and enforcement actions; trade secrets and other intellectual property; crisis preparedness and response; internal, government and third-party licensure, credentialing, accreditation, HCQIA, HEDIS and other peer review and quality reporting, audits, investigations, enforcement and defense; patient relations and care; internal controls and regulatory compliance; payer-provider, provider-provider, vendor, patient, governmental and community relations; facilities, practice, products and other sales, mergers, acquisitions and other business and commercial transactions; government procurement and contracting; grants; tax-exemption and not-for-profit; 1557 and other Civil Rights; privacy and data security; training; risk and change management; regulatory affairs and public policy; process, product and service improvement, development and innovation, and other legal and operational compliance and risk management, government and regulatory affairs and operations concerns.
Ms. Stamer has extensive health care reimbursement and insurance experience advising and defending plan sponsors, administrators, insurance and managed care organizations, health care providers, payers, and others about Medicare, Medicaid, Medicare and Medicaid Advantage, Tri-Care, self-insured group, association, individual and employer and association group and other health benefit programs and coverages including but not limited to advising public and private payers about coverage and program design and documentation, advising and defending providers, payers and systems and billing services entities about systems and process design, audits, and other processes; provider credentialing, and contracting; providers and payer billing, reimbursement, claims audits, denials and appeals, coverage coordination, reporting, direct contracting, False Claims Act, Medicare & Medicaid, ERISA, state Prompt Pay, out-of-network and other nonpar insured, and other health care claims, prepayment, post-payment and other coverage, claims denials, appeals, billing and fraud investigations and actions and other reimbursement and payment related investigation, enforcement, litigation and actions. Scribe for the ABA JCEB annual agency meeting with HHS OCR, she also has worked extensively on health and health benefit coding, billing and claims, meaningful use and EMR, billing and reimbursement, quality measurement and reimbursement, HIPAA, FACTA, PCI, trade secret, physician and other medical, workforce, consumer financial and other data confidentiality and privacy, federal and state data security, data breach and mitigation, and other information privacy and data security concerns.
Author of leading works on a multitude of health care, health plan and other health industry matters, the American Bar Association (ABA) International Section Life Sciences Committee Vice Chair, a Scribe for the ABA Joint Committee on Employee Benefits (JCEB) Annual OCR Agency Meeting, former Vice President of the North Texas Health Care Compliance Professionals Association, past Chair of the ABA Health Law Section Managed Care & Insurance Section, past ABA JCEB Council Representative and CLE and Marketing Committee Chair, past Board President of Richardson Development Center (now Warren Center) for Children Early Childhood Intervention Agency, past North Texas United Way Long Range Planning Committee Member, and past Board Member and Compliance Chair of the National Kidney Foundation of North Texas, Ms. Stamer’s health industry clients include public health organizations; public and private hospitals, healthcare systems, clinics and other health care facilities; physicians, physician practices, medical staff, and other provider organizations; skilled nursing, long term care, assisted living, home health, ambulatory surgery, dialysis, telemedicine, DME, Pharma, clinics, and other health care providers; billing, management and other administrative services organizations; insured, self-insured, association and other health plans; PPOs, HMOs and other managed care organizations, insurance, claims administration, utilization management, and other health care payers; public and private peer review, quality assurance, accreditation and licensing; technology and other outsourcing; healthcare clearinghouse and other data; research; public and private social and community organizations; real estate, technology, clinical pathways, and other developers; investors, banks and financial institutions; audit, accounting, law firm; consulting; document management and recordkeeping, business associates, vendors, and service providers and other professional and other health industry organizations; academic medicine; trade associations; legislative and other law making bodies and others.
A popular lecturer and widely published author on health industry concerns, Ms. Stamer continuously advises health industry clients about compliance and internal controls, workforce and medical staff performance, quality, governance, reimbursement, privacy and data security, and other risk management and operational matters. Ms. Stamer also publishes and speaks extensively on health and managed care industry regulatory, staffing and human resources, compensation and benefits, technology, public policy, reimbursement and other operations and risk management concerns.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other related concerns by her service in the leadership of the Solutions Law Press, Inc. Coalition for Responsible Health Policy, its PROJECT COPE: Coalition on Patient Empowerment, and a broad range of other professional and civic organizations including North Texas Healthcare Compliance Association, a founding Board Member and past President of the Alliance for Healthcare Excellence, past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children (now Warren Center For Children); current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee, current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Section, a current Defined Contribution Plan Committee Co-Chair, former Group Chair and Co-Chair of the ABA RPTE Section Employee Benefits Group, past Representative and chair of various committees of ABA Joint Committee on Employee Benefits; a ABA Health Law Coordinating Council representative, former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, a former member of the Board of Directors of the Southwest Benefits Association and others.
For more information about Ms. Stamer or her health industry and other experience and involvements, see here or contact Ms. Stamer via telephone at (214) 452-8297 or via e-mail here.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here.
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advise or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on Flurry of Reform Activity Sign Employers, Health Plans Should Prepare To Respond To Last Minute Health Reforms This Fall |
Comments Off on Flurry of Reform Activity Sign Employers, Health Plans Should Prepare To Respond To Last Minute Health Reforms This Fall |  105(h), 4980D, 4980H, 6039D, ACA, Affordable Care Act, Appeals, Association Health Plan, board of directors, Brokers, Cafeteria Plans, Claims, Claims Administration, COBRA, compensation, compliance, Contraception, Corporate Compliance, Electronic Medical Record, employee, Employee Benefits, Employer, Employers, Employment, Employment Tax, EMR, ERISA, Excise Tax, Excise Taxes, Fiduciary Responsibility, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, health plan, Health Plans, health reform, HR, Human Resources, Insurance, insurers, Internal Controls, Internal Revenue Code, Mental Health, Mental Health Parity, MEWA, Obamacare, Patient Empowerment, Patient Protection & Affordable Care Act, Pay, Payroll Tax, Plan Admistrator, Prescription Drugs, preventive care, Professional Liability, Risk Management, Technology, Uncategorized, Union, Wellness, Worker Classification |
105(h), 4980D, 4980H, 6039D, ACA, Affordable Care Act, Appeals, Association Health Plan, board of directors, Brokers, Cafeteria Plans, Claims, Claims Administration, COBRA, compensation, compliance, Contraception, Corporate Compliance, Electronic Medical Record, employee, Employee Benefits, Employer, Employers, Employment, Employment Tax, EMR, ERISA, Excise Tax, Excise Taxes, Fiduciary Responsibility, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, health plan, Health Plans, health reform, HR, Human Resources, Insurance, insurers, Internal Controls, Internal Revenue Code, Mental Health, Mental Health Parity, MEWA, Obamacare, Patient Empowerment, Patient Protection & Affordable Care Act, Pay, Payroll Tax, Plan Admistrator, Prescription Drugs, preventive care, Professional Liability, Risk Management, Technology, Uncategorized, Union, Wellness, Worker Classification |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
May 18, 2018
Today the U.S. Department of Labor issued a press release about the publication of a new OFCCP Directive extending the enforcement moratorium relating to the affirmative obligations of TRICARE providers for two years. This moratorium has been in effect for four years, and will now expire on May 7, 2021; it will also now apply to Veterans Affairs Health Benefits Program providers.
This extension will provide OFCCP time to receive feedback from stakeholders, relieve uncertainty, and give OFCCP an opportunity to evaluate and address legislation that may be enacted on this issue.
About The Author
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation; Former Chair of the RPTE Employee Benefits and Compensation Committee, a current Co-Chair of the Committee, and the former Chair of its Welfare Benefit and its Defined Compensation Plan Committees and former RPTE Joint Committee on Employee Benefits Council (JCEB) Representative, Cynthia Marcotte Stamer is a Martindale-Hubble “AV-Preeminent” practicing attorney and management consultant, author, public policy advocate, author and lecturer repeatedly recognized for her 30 plus years’ of work and pragmatic thought leadership, publications and training on health, pension and other employee benefit, insurance, labor and employment, and health care fiduciary responsibility, payment, investment, contracting and other design, administration and compliance concerns as among the “Top Rated Labor & Employment Lawyers in Texas,” a “Legal Leader,” a “Top Woman Lawyer” and with other awards by LexisNexis® Martindale-Hubbell®; as among the “Best Lawyers In Dallas” for her work in the field of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, in International Who’s Who of Professionals and with numerous other awards and distinctions.
Highly valued for her ability to meld her extensive legal and industry knowledge and experience with her talents as an insightful innovator and pragmatic problem solver, Ms. Stamer advises, represents and defends employer, union, multi-employer, association and other employee benefit plan sponsors, insurers and managed care organizations, fiduciaries, plan administrators, technology and other service providers, government and community leaders and others about health and other employee benefit and insurance program and policy design and innovation, funding, documentation, administration, communication, data security and use, contracting, plan, public and regulatory reforms and enforcement, and other risk management, compliance and operations matters. Her experience encompasses leading and supporting the development and defense of innovative new policies, programs, practices and solutions; advising and representing clients on routine plan establishment, plan documentation and contract drafting and review, administration, change and other compliance and operations; crisis prevention and response, compliance and risk management audits and investigations, enforcement actions and other dealings with the US Congress, Departments of Labor, Treasury, Health & Human Services, Federal Trade Commission, Justice, Securities and Exchange Commission, Education and other federal agencies, state legislatures, attorneys general, insurance, labor, worker’s compensation, and other agencies and regulators, and various other foreign and domestic governmental bodies and agencies. She also provides strategic and other supports clients in defending litigation as lead strategy counsel, special counsel and as an expert witness. Alongside her extensive legal and operational experience, Ms. Stamer also is recognized for her work as a public and regulatory policy advocate and community leader with a gift for finding pragmatic solutions and helping to forge the common ground necessary to build consensus. Best known for her domestic public policy and community leadership on health care and insurance reform, Ms. Stamer’s lifelong public policy and community service involvement includes service as a lead consultant to the Government of Bolivia on its pension privatization project, as well as extensive legislative and regulatory reform, advocacy and input workforce, worker classification, employee benefit, public health and healthcare, social security and other disability and aging in place, education, migration reforms domestically and internationally throughout her adult life. In addition to her public and regulatory policy involvement, Ms. Stamer also contributes her service and leadership to a professional and civic organizations and efforts including her involvement as the Founder and Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE; Coalition on Patient Empowerment, a founding Board Member and past President of the Alliance for Healthcare Excellence; Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; Vice Chair, Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group; current Fiduciary Responsibility Committee Co-Chair and Membership Committee member of the ABA RPTE Section; former RPTE Employee Benefits and Other Compensation Group Chair, former Chair and Co-Chair of its Welfare Plans Committee, and Defined Contribution Plans Committee; former RPTE Representative to ABA Joint Committee on Employee Benefits Council; former RPTE Representative to the ABA Health Law Coordinating Counsel; former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, former Board Member, Continuing Education Chair and Treasurer of the Southwest Benefits Association; Vice President of the North Texas Healthcare Compliance Professionals Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; past Dallas World Affairs Council Board Member, and in leadership of many other professional, civic and community organizations. Ms. Stamer also is a highly popular lecturer, symposia chair and author, who publishes and speaks extensively on health and managed care industry, human resources, employment and other privacy, data security and other technology, regulatory and operational risk management for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, the Society of Professional Benefits Administrators, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients, serves on the faculty and planning committee of many workshops, seminars, and symposia, and on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Beyond these involvements, Ms. Stamer also is active in the leadership of a broad range of other public policy advocacy and other professional and civic organizations and involvements. Through these and other involvements, she helps develop and build solutions, build consensus, garner funding and other resources, manage compliance and other operations, and take other actions to identify promote tangible improvements in health care and other policy and operational areas.
Before founding her current law firm, Cynthia Marcotte Stamer, P.C., Ms. Stamer practiced law as a partner with several prominent national and international law firms for more than 10 years before founding Cynthia Marcotte Stamer, P.C. to practice her unique brand of “Solutions law™” and to devote more time to the pragmatic policy and system reform, community education and innovation, and other health system improvement efforts of her PROJECT COPE: the Coalition on Patient Empowerment initiative.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com such as the following
▪DOL Spending Reports Required As Taxpayer Tool Need Improvement
▪Check & Protect Health & Other Electronic Systems & Data Against New Security Threat
▪April 1 New Deadline To Update Benefit Plan Disability Determination Claims & Appeals Procesures; Hear More on 1/26
▪Arizona Proposal To Ban Sexual Harassment Confidentiality Agreements Sign Of Growing Employer Risks
▪$23M Penalty Small Part of 21st Century’s Data Breach Fallout; Offers Data Breach Lessons For Other Businesses
▪Take Care of Your Good People
▪Read Tax Cuts and Jobs Act Conference Report For Tax Reform From Source
▪Check How IRS 2018 Retirement & Saving Plan Limits and Amounts Cost Of Living Adjustments Impact Your HR & Retirement Plan Administration & Planning
▪IRS Prepares To Nail Employers Under Obamacare Mandate While Giving Some Individual Mandate Relief
▪Hiring & Retaining Workers Growing Business Challenge
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on OFCCP Extends TRICARE Affirmative Action Morotorium |
Comments Off on OFCCP Extends TRICARE Affirmative Action Morotorium |  Affirmative Action, Civil Rights, compliance, Corporate Compliance, corporate governance, Disability, Disability Discrimination, Discrimination, EEOC, EEOC, Employee Benefits, Employer, Employers, OFCCP, Uncategorized, veterans, VEVRAA |
Affirmative Action, Civil Rights, compliance, Corporate Compliance, corporate governance, Disability, Disability Discrimination, Discrimination, EEOC, EEOC, Employee Benefits, Employer, Employers, OFCCP, Uncategorized, veterans, VEVRAA |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
May 11, 2018
The 2018 maximum deductible Health Savings Account (HSA) contribution for individuals with family coverage under a high deductible health plan (HDHP) is $6,900, rather than the lower $$6850 limitation that the Internal Revenue Service (IRS) and Department of Treasury originally identified as the 2018 maximum deduction amount last March.
The mid-year change in the 2018 annual limit that Internal Revenue Code § 223(b)(2)(B) sets for the maximum deductible HSA contribution for individuals with family coverage under a HDHP announced in Revenue Procedure 2018-27 on April 26 corrects a mistake in the amount of the 2018 annual limit amount that the Treasury Department and the IRS previously announced in Rev. Proc. 2018-18 on March 2, 2018. Revenue Procedure does not change any other annual limitation or any other requirement under section 223 for calendar year 2018.
Before Revenue Procedure 2018-27, the annual limitation on deductions under section 223(b)(2)(B) for an individual with family coverage under an HDHP at $6,850 for 2018 – a $50 reduction in the amount of the 2018 limit amount set in Revenue Procedure 2018-18, which reduced the originally announced 2018 limit amount of $6,900 that the Treasury Department and IRS previously had announced in May 4, 2017 in Revenue Procedure 2017-37. After publishing the original $6,900 limit in Revenue Procedure 2017-37, Congress changed the rules on inflation adjustments as part of “An Act to Provide for Reconciliation Pursuant to Titles II and V of the Concurrent Resolution on the Budget for Fiscal Year 2018” (the Act), Pub. L. 115–97, 131 Stat. 2504, enacted December 22, 2017. Consequently, on March 2, 2018, the Treasury Department and the IRS released Rev. Proc. 2018-18, announcing the reduction of the 2018 limit to $6,850 to reflect the statutory amendments to the inflation adjustments under the Act. However, IRS and Treasury say that the recently announced change in the 2018 annual limitation resulted after stakeholders informed the Treasury Department and the IRS that implementing the $50 reduction to the limitation on deductions for individuals with family coverage would impose numerous unanticipated administrative and financial burdens. Specifically, stakeholders informed the Treasury Department and the IRS that the costs of modifying the various systems to reflect the reduced maximum, as well as the costs associated with distributing a $50 excess contribution (and earnings), would be significantly greater than any tax benefit associated with an unreduced HSA contribution (and in some instances may exceed $50). Some stakeholders also pointed to section 223(g)(1), which requires annual inflation adjustments for HSAs to be published by June 1 of the preceding calendar year, as another indication that a current year change would be unduly burdensome.
In response to these concerns, the Treasury Department and the IRS have determined that it is in the best interest of sound and efficient tax administration to allow taxpayers to treat the $6,900 annual limitation originally published in Rev. Proc. 2017-37 as the 2018 inflation adjusted limitation on HSA contributions for eligible individuals with family coverage under an HDHP. Accordingly, $6,900 now is the annual limitation on deductions under section 223(b)(2)(B) for an individual with family coverage under an HDHP for calendar year 2018.
Before this announced change, some individuals may have received distributions of HSA contribution amounts that were treated as in excess of the annual contribution limit amount before publication of Revenue Procedure 2018-27. Revenue Procedure 2018-27 outlines two alternatives for dealing with these distributions.
Under the first alternative, an individual who receives a distribution from an HSA of an excess contribution (with earnings) based on the $6,850 deduction limit published in Rev. Proc. 2018-18 may repay the distribution to the HSA and treat the distribution as the result of a mistake of fact due to reasonable cause under Q&A-37 of Notice 2004-50. The portion of a distribution (including earnings) that an individual repays to an HSA by April 15, 2019, is not included in the individual’s gross income under section 223(f)(2) or subject to the 20 percent additional tax under section 223(f)(4). The repayment is not subject to the excise tax on excess contributions under section 4973(a)(5). Also, mistaken distributions that are repaid to an HSA are not required to be reported on Form 1099-SA or Form 8889 and are not required to be reported as additional HSA contributions. However, in accordance with Q&A-76 of Notice 2004-50, a trustee or custodian is not required to allow individuals to repay mistaken distributions.
Alternatively, Revenue Procedure 2018-27 states that an individual who receives a distribution from an HSA of an excess contribution (with earnings) based on the $6,850 deduction limit published in Rev. Proc. 2018-18 and does not repay the distribution to the HSA may treat the distribution in accordance with section 223(f)(3), which describes the treatment of excess contributions returned before the due date of return. Thus, the excess contribution generally would not be included in gross income under section 223(f)(2) or subject to the 20 percent additional tax under section 223(f)(4), provided the distribution is received on or before the last day prescribed by law (including extensions of time) for filing the individual’s 2018 tax return. However, Revenue Procedure 2018-27 adds that the tax treatment under this alternative does not apply to distributions from an HSA that are attributable to employer contributions (pursuant to a cafeteria plan election or otherwise) if the employer does not include any portion of the contributions in the employee’s wages because the employer treats $6,900 as the annual limitation on deductions under section 223(b)(2)(B). In that case, unless the distribution from the HSA is used to pay qualified medical expenses, the distribution is includible in the employee’s gross income under section 223(f)(2) and subject to the 20 percent additional tax under section 223(f)(4).
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
The author of the “Texas Payday Act,” and numerous other highly regarded publications on wage and hour and other human resources, employee benefits and compensation publications, Ms. Stamer is well-known for her 30 years of extensive wage and hour, compensation and other management advice and representation of restaurant and other hospitality, health, insurance, financial services, technology, energy, manufacturing, retail, governmental and other domestic and international businesses of all types and sizes.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here including:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on 2018 Family HSA Deductible Contribution Limit Restored To $6,900 |
Comments Off on 2018 Family HSA Deductible Contribution Limit Restored To $6,900 |  105(h), 401(k), 4980D, 4980H, 6039D, ACA, Cafeteria Plans, compensation, compliance, Corporate Compliance, corporate governance, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Policies, Employment Tax, Excise Tax, Excise Taxes, Executive Compensation, health benefit, Health Benefits, health Care, health insurance, health plan, Health Plans, HR, HSA, Human Resources, Income Tax, Internal Revenue Code, Labor Management Relations, Management, Pay, Payroll Tax, Tax, Tax Qualification, Uncategorized | Tagged: High Deductible Health PLan, HSA |
105(h), 401(k), 4980D, 4980H, 6039D, ACA, Cafeteria Plans, compensation, compliance, Corporate Compliance, corporate governance, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Policies, Employment Tax, Excise Tax, Excise Taxes, Executive Compensation, health benefit, Health Benefits, health Care, health insurance, health plan, Health Plans, HR, HSA, Human Resources, Income Tax, Internal Revenue Code, Labor Management Relations, Management, Pay, Payroll Tax, Tax, Tax Qualification, Uncategorized | Tagged: High Deductible Health PLan, HSA |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
April 18, 2018
Employers should consider inviting their workers to conduct a Paycheck Checkup to review their withholding elections to confirm they have the right amount of tax deducted from their paychecks in response to tax law changes enacted by the Tax Cuts and Jobs Act (Trump Tax) and other recent legislation. Helping workers properly to take into account tax relief or other changes reducing their income tax liability can help boost workers’ take home pay, helping them to see more benefit from the wages paid by the employer at payday.
The amount of withholding that an employer withholds from an employee’s pay generally depends upon two factors:
- The amount the employee can earn; and
- The accuracy of the personal information the employee uses to complete the Form W-4 to notify the employer of his withholding elections; and
- The tax rules that decide how much tax the employee ultimately will owe when their personal income tax returns become due on April 15, 2018.
Although most employees don’t think about the potential need to re-evaluate the withholding elections on their current Form W-4 unless reminded by an employer or professional advisor, it’s generally a good idea for workers to periodically review and update their withholding elections since these often change from time to time. Encouraging workers to periodically review and update their W-4 elections can help workers maximize their take home pay while minimizing the risk of being surprised with an unexpected income tax or even under withholding penalty when they file their annual income tax return.
A number of recent events make it particularly likely that employees will benefit from re-evaluating their W-4 withholding now. For one thing, the Tax Cuts and Jobs Act recently changed the way income tax is calculated for most individual taxpayers. As many of these changes were enacted to provide individual tax relief for many taxpayers, workers qualifying for this relief that do not review and update their withholding elections likely are having the employer withhold more tax than necessary from their paychecks. Beyond these tax rule changes, many workers also may need to update their withholding elections in response to changes in their income, marital or other family status or other changes in their personal situation that also can affect the income tax withholding of the individual worker.
The Internal Revenue Service recently updated the Withholding Calculator the IRS provides on its website to help individuals estimate their annual income tax for purposes of deciding the withholding they should enter on their Form W-4 in light of the Tax Cuts and Jobs Act changes. Individuals can use the Withholding Calculator to estimate their 2018 and to compare their current tax withholding to help the individual decide if the individual needs to change his withholding with an employer.
More details about the Withholding Calculator and the new 2018 withholding tables can be found using the following internet links on the IRS’ Frequently Asked Question pages:
Employers should consider sending a reminder to workers to review their Form W-4 using these tools to determine if they can increase their take home pay by changing their withholding to take into account any potential income tax and withholding reductions they qualify for, if any, as a result of the Tax Cuts and Jobs Act or other changes in factors that impact their withholding and income tax liability or if other changes are warranted. Because most employees just completed their annual tax returns and likely have not considered the potential need to change their elections for tax reform or other changes, employees are likely to be particularly receptive and responsive to these reminders now. Employers and benefit plan administrators also may wish to consider helping employees remember to review and update their Form W-4 withholding when sending benefit enrollment packages, processing benefit enrollment elections when announcing pay increases or bonuses, in employee handbooks or payroll stuffers, at annual enrollment times or in response to mid-year election or beneficiary change notifications and at other times when the employer or their benefit plans deal with life event or benefit election events that could impact an employee’s withholding.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
The author of the “Texas Payday Act,” and numerous other highly regarded publications on wage and hour and other human resources, employee benefits and compensation publications, Ms. Stamer is well-known for her 30 years of extensive wage and hour, compensation and other management advice and representation of restaurant and other hospitality, health, insurance, financial services, technology, energy, manufacturing, retail, governmental and other domestic and international businesses of all types and sizes.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here including:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on Remind Employees To Update Withholding |
Comments Off on Remind Employees To Update Withholding |  105(h), 401(k), 4980D, 4980H, 6039D, Cafeteria Plans, compensation, compliance, Corporate Compliance, corporate governance, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, Disability, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Policies, Employment Tax, Excise Tax, Excise Taxes, Executive Compensation, health benefit, Health Benefits, health plan, Health Plans, HR, Human Resources, Income Tax, Internal Revenue Code, Labor Management Relations, Management, Pay, Payroll Tax, Tax, Tax Qualification, Uncategorized |
105(h), 401(k), 4980D, 4980H, 6039D, Cafeteria Plans, compensation, compliance, Corporate Compliance, corporate governance, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, Disability, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Policies, Employment Tax, Excise Tax, Excise Taxes, Executive Compensation, health benefit, Health Benefits, health plan, Health Plans, HR, Human Resources, Income Tax, Internal Revenue Code, Labor Management Relations, Management, Pay, Payroll Tax, Tax, Tax Qualification, Uncategorized |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
April 12, 2018
With the Trump Administration U.S. Department of Labor Wage and Hour Division (WHD) continuing its aggressive investigation and enforcement of minimum wage, overtime and other Fair Labor Standards Act (FLSA) and other wage and hour laws it used to recover more than $1.2 billion in back pay for workers over the past five years, Agriculture, Amusement, Apparel Manufacturing, Auto Repair, Child Care Services, Construction, Food Services, Guard Services, Hair, Nail & Skin Care Services, Health Care, Hotels and Motels, Janitorial Services, Landscaping Services, Retail, and Temporary Help and other U.S. employers should evaluate their current and past potential liability exposures and consider using the new pilot WHD self-audit Payroll Audit Independent Determination (PAID) program announced by WHD on March 6 or other options to mitigate their liability for their own or temporary or other contract labor’s existing or past minimum wage and hour law violations.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
The author of the “Texas Payday Act,” and numerous other highly regarded publications on wage and hour and other human resources, employee benefits and compensation publications, Ms. Stamer is well-known for her 30 years of extensive wage and hour, compensation and other management advice and representation of restaurant and other hospitality, health, insurance, financial services, technology, energy, manufacturing, retail, governmental and other domestic and international businesses of all types and sizes.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here including:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on Employers Should Weigh New DOL PAID Program, Other Options To Manage Rising FLSA Minimum Wage & Overtime Risks |
Comments Off on Employers Should Weigh New DOL PAID Program, Other Options To Manage Rising FLSA Minimum Wage & Overtime Risks |  Attorney-Client Privilege, board of directors, Brokers, business travel, Child Labor, compensation, compliance, Construction, Corporate Compliance, corporate governance, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Policies, enforcement, Executive Compensation, Exempt, Fair Labor Standards Act, FLSA, HR, Human Resources, Insurance, Internal Controls, Internal Investigations, Labor Management Relations, Management, Managment, officers, Overtime, Telecommuting, Uncategorized, Union, Workforce | Tagged: Employer, FLSA, wage, Wage & Hour |
Attorney-Client Privilege, board of directors, Brokers, business travel, Child Labor, compensation, compliance, Construction, Corporate Compliance, corporate governance, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Policies, enforcement, Executive Compensation, Exempt, Fair Labor Standards Act, FLSA, HR, Human Resources, Insurance, Internal Controls, Internal Investigations, Labor Management Relations, Management, Managment, officers, Overtime, Telecommuting, Uncategorized, Union, Workforce | Tagged: Employer, FLSA, wage, Wage & Hour |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
February 15, 2018
Health plans and insurers, their service providers that act as business associates within the meaning of the Health Insurance Portability & Accountability Act (HIPAA) and employer and other health plan sponsors, fiduciaries, and other management leaders should heed the warnings contained in the new Resolution Agreement (FileFax Resolution Agreement) with former HIPAA business associate FileFax, Inc. announced by the Department of Health & Human Services (HHS) Office of Civil Rights (OCR) about their own need to ensure that they and their business associates comply with HIPAA’s business associate and other Privacy, Security, Breach Notification rules as well as the advisability of tightening up their risk management and oversight of business associates that handle protected health information (PHI).
Significant for business associates as what appears to be the first announced resolution agreement with a business associate directly charged by OCR with violating HIPAA and the second resolution agreement pursued and reached with a HIPAA-regulated entity in bankruptcy, the FileFax, Inc. Resolution Agreement OCR announced February 13, 2018 also contains critical lessons for Covered Entities about their dealings with their own business associates when read in conjunction with the April, 2017 resolution agreement the Center for Children’s Digestive Health (CCDH) agreed to resolve OCR charges CCDC, as a Covered Entity, violated HIPAA by allowing FileFax, Inc. to act as its business associate without adequately complying with HIPAA’s business associate requirements.
With widespread media coverage over large scale breaches of health care and other sensitive information placing further pressure upon OCR and other governmental agencies to act to protect Americans’ privacy and data fueling even greater demands for OCR and other agencies to take meaningful action to enforce HIPAA and other privacy and data security requirements, health plans, health care providers, health care clearinghouses (Covered Entities) and their business associates can expect OCR and other agencies to continue to turn up the heat on investigation and enforcement of HIPAA compliance.
In the face of these developments, Covered Entities, their business associates and those responsible for their leadership and operations need to recognize and take the necessary steps both effectively to manage their own HIPAA compliance and risk management as well as to anticipate and make provision to deal with the likelihood that they may face HIPAA responsibilities, exposures and other fallout from their own or another business partner’s breach of PHI or other sensitive data or other HIPAA violations, bankruptcy or other business distress, or other compliance or business event.
HIPAA Privacy, Security & Breach Notification Rule Responsibilities & Risks
The Privacy Rule requires that health plans, health care providers, health care clearinghouses (Covered Entities) and their vendors that qualify as “business associates” under HIPAA comply with detailed requirements concerning the protection, use, access, destruction and disclosure of protected health information. As part of these requirements, Covered Entities and their business associates must adopt, administer and enforce detailed policies and practices, assess, monitor and maintain the security of electronic protected health information (ePHI) and other protected health information, provide notices of privacy practices and breaches of “unsecured” ePHI, afford individuals that are the subject of protected health information certain rights and comply with other requirements as specified by the Privacy, Security and Breach Notification Rules. In addition, Covered Entities and business associates also must enter into a written and signed business associate agreement that contains the elements specified in Privacy Rule § 164.504(e) before the business associate creates, uses, accesses or discloses PHI of the Covered Entity. Furthermore, the Privacy Rule includes extensive documentation and keeping requirements require that Covered Entities and BAs maintain copies of these BAAs for a minimum of six years and to provide that documentation to OCR upon demand.
Violations of the Privacy Rule can carry stiff civil monetary penalties or even criminal penalties. Pursuant to amendments to HIPAA enacted as part of the HITECH Act, civil penalties typically do not apply to violations punished under the criminal penalty rules of HIPAA set forth in Social Security Act , 42 U.S.C § 1320d-6 (Section 1177).
Resolution Agreements the just announced FileFax Resolution Agreement allow Covered Entities and business associates to resolve potentially substantially larger civil monetary penalty liabilities that OCR can impose under the civil enforcement provisions of HIPAA for HIPAA violations through a negotiated settlement process. As amended by the HITECH Act, the civil enforcement provisions of HIPAA empower OCR to impose Civil Monetary Penalties on both Covered Entities and BAs for violations of any of the requirements of the Privacy or Security Rules. The penalty ranges for civil violations depends upon the circumstances associated with the violations and are subject to upward adjustment for inflation. As most recently adjusted here effective September 6, 2016, the following currently are the progressively increasing Civil Monetary Penalty tiers:
- A minimum penalty of $100 and a maximum penalty of $50,000 per violation, for violations which the CE or BA “did not know, and by exercising reasonable diligence would not have known” about using “the business care and prudence expected from a person seeking to satisfy a legal requirement under similar circumstances;”
- A minimum penalty of $1,000 and a maximum penalty of $50,000 per violation, for violations for “reasonable cause” which do not rise to the level of “willful neglect” where “reasonable cause” means the “circumstances that would make it unreasonable for the Covered Entity, despite the exercise of ordinary business care and prudence, to comply with the violated Privacy Rule requirement;”
- A minimum penalty of $10,000 and a maximum penalty of $50,000 per violation, for violations attributed to “willful neglect,” defined as “the conscious, intentional failure or reckless indifference to the obligation to comply” with the requirement or prohibition; and
- A minimum penalty of $50,000 and a maximum penalty of $1.5 million per violation, for violations attributed to “willful neglect” not remedied within 30 days of the date that the Covered Entity or BA knew or should have known of the violation.
For continuing violations such as failing to implement a required BAA, OCR can treat each day of noncompliance as a separate violation. However, sanctions under each of these tiers generally are subject to a maximum penalty of $1,500,000 for violations of identical requirements or prohibitions during a calendar year. For violations such as the failure to implement and maintain a required BAA where more than one Covered Entity bears responsibility for the violation, OCR an impose Civil Monetary Penalties against each culpable party. OCR considers a variety of mitigating and aggravating facts and circumstances when arriving at the amount of the penalty within each of these applicable tiers to impose.
In addition to these potential civil liability exposures, Covered Entities, their business associates and other individuals or organizations that wrongfully use, access or disclose electronic or other protected health information also can face civil liability under various circumstances. The criminal enforcement provisions of HIPAA authorize the Justice Department to prosecute a person who knowingly in violation of the Privacy Rule (1) uses or causes to be used a unique health identifier; (2) obtains individually identifiable health information relating to an individual; or (3) discloses individually identifiable health information to another person, punishable by the following criminal sanctions and penalties:
- A fine of up to $50,000, imprisoned not more than 1 year, or both;
- If the offense is committed under false pretenses, a fine of up to $100,000, imprisonment of not more than 5 years, or both; and
- If the offense is committed with intent to sell, transfer, or use individually identifiable health information for commercial advantage, personal gain, or malicious harm, a fine of up to $250,000, imprisoned not more than 10 years, or both.
Because HIPAA Privacy Rule criminal violations are Class A Misdemeanors or felonies, Covered Entities and business associates should include HIPAA compliance in their Federal Sentencing Guideline Compliance Programs and practices and need to be concerned both about criminal exposure for their own direct violations, as well as imputed organizational liability for violations committed by their employees or agents under the Federal Sentencing Guidelines, particularly where their failure to implement or administer these required compliance policies and practices or failure to properly investigate or redress potential violations enables, perpetuates or covers up the criminal breach.
FileFax, Inc. Breach & Resolution Agreement
While Congress amended the Civil Monetary Penalty provisions of HIPAA enforced by OCR to make many of the requirements and Civil Monetary Penalty sanctions of HIPAA directly enforceable by OCR against business associates as part of the Health Information Technology for Economic and Clinical Health (HITECH) Act, enacted as part of the American Recovery and Reinvestment Act of 2009, the FileFax Resolution Agreement appears to be the first HIPAA resolution agreement with a business associate announced by OCR.
Indeed, OCR’s enforcement action that resulted in the FileFax Resolution Agreement would never have occurred had FileFax, Inc. not become involved in handling medical records containing PHI in the capacity of a business associate for Covered Entities.
Before filing for bankruptcy in 2016, FileFax, Inc. advertised it provided HIPAA-compliant storage, maintenance, and delivery of medical records for HIPAA Covered Entities including Illinois based health care provider CCDC, which entered into a resolution agreement with OCR in April, 2017 to resolve OCR charges that it violated HIPAA by allowing FileFax, Inc. to handle PHI without fulfilling HIPAA’s business associate agreement requirements.
Like the CCDC Resolution Agreement, the FileFax, Inc. Resolution Agreement resulted from an investigation of FileFax, Inc. that OCR began in response to a February 10, 2015 anonymous complaint filed with OCR about FileFax, Inc. about deficiencies in its delivery of these HIPAA services in its capacity as a business associate to Covered Entities. The complaint to OCR alleged that FileFax, Inc. violated these requirements because an individual transported medical records obtained from FileFax, Inc. to a shredding and recycling facility to sell on February 6 and 9, 2015.
OCR’s investigation of the complaint against FileFax, Inc. confirmed that an individual had left medical records of approximately 2,150 patients at the shredding and recycling facility, and that these medical records contained patients’ PHI. OCR’s investigation additionally found that between January 28, 2015, and February 14, 2015, FileFax, Inc. impermissibly disclosed the PHI of 2,150 individuals by leaving the PHI in an unlocked truck in the FileFax, Inc. parking lot, or by granting permission to an unauthorized person to remove the PHI from FileFax, Inc. and leaving the PHI unsecured outside the FileFax, Inc. facility.
After OCR commenced its investigation of the complaint, FileFax, Inc. was placed into bankruptcy and a receiver was appointed to liquidate FileFax, Inc.’s assets for distribution to creditors and others in 2016. Despite the bankruptcy, OCR continued to pursue enforcement against FileFax, Inc. for the HIPAA violations it found through its investigation. On February 13, 2018, OCR announced that that the receiver on behalf of FileFax, Inc. had agreed in the FileFax Resolution Agreement to pay a $100,000 monetary settlement out of the bankruptcy estate and to arrange to properly store and dispose of remaining medical records found at FileFax, Inc.’s facility in compliance with HIPAA to resolve OCR’s HIPAA charges against FileFax, Inc.
OCR Previously Sanctioned Covered Entity For Involvement With FileFax, Inc.
Beyond affirming the exposure business associates to OCR civil monetary penalties or other enforcement for violating HIPAA, the FileFax Resolution Agreement in conjunction with OCR’s previously announced April 20, 2017 resolution agreement (CCDC Resolution Agreement) with CCDC also demonstrates the need for Covered Entities to recognize that their organizations are likely to face HIPAA investigations or enforcement from HIPAA violations by or OCR audits or investigations of the conduct of their business associates.
In fact, this is exactly what happened to CCDC. A small, Illinois based Covered Entity, CCDC used FileFax, Inc. to store and dispose of medical records. As a consequence of the FileFax, Inc. investigation, OCR conducted a compliance review of CCDC. OCR reports that its compliance review revealed that while CCDC had disclosed to and allowed FileFax, Inc. to store records containing PHI for CCDC since in 2003, neither party could produce a signed business associate agreement (BAA) prior to October 12, 2015. As a consequence, OCR charged CCDC with violating HIPAA by disclosing PHI to FileFax, Inc. in violation of HIPAA’s business associate requirements.
To resolve its exposure to potentially much greater civil monetary penalties associated with this charge, CCDC agreed under the CCDC Resolution Agreement to pay OCR a $31,000 resolution payment and take a variety of corrective actions. Beyond requiring CCDC to implement and maintain written business associate agreements before allowing business associates to possess or access PHI, the corrective action plan imposed as part of the CCDC Resolution Agreement also expressly requires CCDC to promptly investigate information of a possible violation of its HIPAA policies and procedures by a “workforce member,” which the Privacy Rule defines to include a business associate, and if the investigation reveals a violation, to report the violation and corrective action taken to OCR.
OCR Enforces HIPAA Against Covered Entities & Business Associates In Bankruptcy
OCR’s announcement of the FileFax Resolution Agreement also is significant in its reaffirmation of OCR to its commitment to HIPAA enforcement, even if the HIPAA-violating Covered Entity or business associate goes bankruptcy.
OCR’s enforcement action against FileFax, Inc. despite its bankruptcy and its successful negotiation of the FileFax Resolution Agreement within the bankruptcy should alert Covered Entities and business associates that OCR does not consider the bankruptcy of a Covered Entity or business associate as an obstacle to OCR enforcement against Covered Entities or business associates that violate HIPAA. The seriousness of OCR’s commitment to enforcement, even in the face of bankruptcy is driven home by its announcement of the FileFax Resolution Agreement on the heels of its December, 2017 announcement of its first OCR HIPAA resolution agreement secured with the formal approval of a bankruptcy court, a resolution agreement (21CO Resolution Agreement) against bankrupt health care provider, 21CO.
Secured with bankruptcy court approval, the 21CO Resolution Agreement resolved potentially much larger civil monetary penalties that the Fort Myers, Florida based provider of cancer care services and radiation oncology could have faced for alleged HIPAA breaches OCR charged it committed in connection with its failure to adequately act to prevent and respond to hacking and misappropriation of records containing sensitive electronic protected health information (ePHI) of up to 2,213597 individuals.
The OCR charges against 21CO arose from an OCR investigation commenced after the Federal Bureau of Investigation (FBI) notified 21CO on November 13, 2015 and a second time on December 13, 2015 than unauthorized third party illegally obtained 21CO sensitive patient information and produced 21CO patient files purchased by a FBI informant. As part of its internal investigation, 21CO hired a third party forensic auditing firm in November 2015. 21CO determined that the attacker may have accessed 21CO’s network SQL database as early as October 3, 2015, through Remote Desktop Protocol from an Exchange Server within 21CO’s network. 21CO determined that it is possible that 2,213,597 individuals may have been affected by the impermissible access to their names, social security numbers, physicians’ names, diagnoses, treatment and insurance information.
Although it knew of the breaches in November and December, 2015, 21CO waited more than three months after the FBI notified it of the breaches before it sent HIPAA or other breach notifications about the data breach to patients or notified investors in March, 2016. Its March 4, 2016 Securities and Exchange Commission 8-K on Data Security Incident (Breach 8-K) states 21CO delayed notification at the request of the FBI to avoid interfering in the criminal investigation of the breach.
When announcing the breach, 21CO provided all individuals affected by the breach with a free one-year subscription to the Experian ProtectMyID fraud protection service. At that time, 21CO said it had no evidence that any patient information actually had been misused. However some victims of the breach subsequently have claimed being victimized by a variety of scams since the breach in news reports and lawsuits about the breach.
At the time of the breach and its March 4, 2016 announcement of the breach, 21CO already was working to resolve other compliance issues. On December 16, 2015, 21CO announced that a 21CO subsidiary had agreed to pay $19.75 million to the United States and $528,000 in attorneys’ fees and costs and comply with a corporate integrity agreement related to a qui tam action in which it was accused of making false claims to Medicare and other federal health programs. See 21CO 8-K Re: Entry into a Material Definitive Agreement (December 22, 2015). Among other things, the corporate integrity agreement required by that settlement required 21CO to appoint a compliance officer and take other steps to maintain compliance with federal health care laws. In addition, five days after releasing the March 4, 2017 Breach 8-K, 21CO notified investors that its subsidiary, 21st Century Oncology, Inc. (“21C”), had agreed to pay $37.4 million to settle health care fraud law charges relating to billing and other protocols of certain staff in the utilization of state-of-the-art radiation dose calculation system used by radiation oncologists called GAMMA. See 21CO 8-K Re: GAMMA Settlement March 9, 2016 ; See also United States Settles False Claims Act Allegations Against 21st Century Oncology for $34.7 Million.
Based on OCR’s subsequent investigation into these breaches, OCR found:
- 21CO impermissibly disclosed certain PHI of 2,213,597 of its patients in violation of 45 C.F.R. § 164.502(a);
- 21CO failed to conduct an accurate and thorough assessment of the potential risks and vulnerabilities to the confidentiality, integrity, and availability of the electronic protected health information (ePHI) held by 21CO in violation of 45 C.F.R. § 164.308(a)(1)(ii)(A);
- 21CO failed to implement certain security measures sufficient to reduce risks and vulnerabilities to a reasonable and appropriate level to comply with 45 C.F.R. § 164.306(A) in violation of 45 C.F.R. § 164.308(a)(1)(ii)(B);
- 21CO failed to implement procedures to regularly review records of information system activity, such as audit logs, access reports, and security incident tracking reports as required by 45 C.F.R. §164.308(a)(1)(ii)(D);
- 21CO disclosed protected health information to a third party vendors, acting as its business associates, without obtaining satisfactory assurances in the form of a written business associate agreement in violation of HIPAA’s business associate rule requirements under 45 C.F.R. §§ 164.502(e) and 164.308(b)(3).
In return for OCR’s agreement not to further pursue charges or penalties relating to the breach investigation, the Resolution Agreement entered into with the approval of the Bankruptcy Court requires that 21CO pay OCR a $2.3 million Resolution Amount and implement to OCR’s satisfaction a corrective action plan that among other things requires that 21CO complete a detailed series of corrective actions to the satisfaction of OCR.
In addition to the OCR investigation that lead to the 21CO Resolution Agreement announced by OCR on December 28, 2017, 21CO experienced other fallout following its March 4, 2016 public disclosure of the breach. Not surprisingly, the breach notification led to a multitude of class-action civil lawsuits by breach victims and shareholders. See, e.g., 16 Data Breach Class Action Lawsuits Filed Against 21st Century Oncology Consolidated; 21st Century Oncology data breach prompts multiple lawsuits. Reports of spoofing and other misleading contacts made to 21CO patients following the breach prompted the Federal Trade Commission (FTC) to issue a specific notice alerting victims about potential false breach notifications and other misleading contacts. See April 4, 2016 FTC Announcement Re: 21st Century Oncology breach exposes patients’ info.
These and other developments also had significant consequences on 21CO’s financial status and leadership. By March 31, 2015, 21CO notified the SEC and investors that it needed added time to complete its financial statements. Subsequent SEC filings document its restatement of financial statements, the departure of board members and other leaders, default on credit terms, and ultimately its filing for Chapter 11 bankruptcy protection in the United States Bankruptcy Court for the Southern District of New York on May 25, 2017.
Because 21CO sought bankruptcy court protection from the fallout of its HIPAA breaches and other compliance and business issues, the 21CO Resolution Agreement required bankruptcy court approval. Funds for payment of the required $2.3 million resolution payment and other charges associated with the investigation apparently are being provided in part from breach liability insurance coverage provided under a policy issued by Beazley Insurance, as the Bankruptcy Court order directs Beazley Breach Response Policy No. W140E2150301 to make immediate payment to the OCR of the resolution amount and the payment of fees incurred by 21CO in connection with regulatory defense issues.
HIPAA & Data Breach Enforcement A Growing Health Plan Risk
Health plans and other Covered Entities, plan sponsors and plan fiduciaries, their business associates and other consultants and service providers and members of their workforce need to recognize that the FileFax, CCDC, 21CO and other resolution agreements are part of a growing trend, rather than isolated incidents of enforcement and that their exposure to investigation and enforcement is likely to continue to rise in the face of growing public and Congressional concern about privacy and data security.
While civil monetary penalty enforcement remains much more common than criminal prosecution, Covered Entities, their business associates and members of their workforce must understand that HIPAA enforcement and resulting liability is growing and that this trend is likely to continue if not increase.
While Department of Justice federal criminal prosecutions and convictions under HIPAA remain relatively rare, they occur and are growing. See e.g., Former Hospital Employee Sentenced for HIPAA Violations (Texas man sentenced to 18 months in federal prison for obtaining protected health information with the intent to use it for personal gain); Three Life Sentences Imposed On Man Following Convictions For Drug Trafficking, Kidnapping, Using Firearms and HIPAA Violations (drug king pin gets multiple 10 year consecutive prison terms for unauthorized access to private health information in violation of HIPAA; his health care worker friend sentenced for accessing electronic medical files and reporting information to him); Former Therapist Charged In HIPAA Case; Hefty Prison Sentence in ID Theft Case (former assisted living facility worker gets 37 months in prison after pleading guilty to wrongful disclosure of HIPAA protected information and other charges); Hefty Prison Sentence in ID Theft Case (former medical supply company owner sentenced to 12 years for HIPAA violations and fraud). While the harshest sentences tend to be associated with health care fraud or other criminal conduct, lighter criminal sentences are imposed against defendants in other cases as well. See e.g., Sentencing In S.C. Medicaid Breach Case (former South Carolina state employee sentenced to three years’ probation, plus community service, for sending personal information about more than 228,000 Medicaid recipients to his personal e-mail account.); HIPAA Violation Leads To Prison Term (former UCLA Healthcare System surgeon gets four months in prison after admitting he illegally read private electronic medical records of celebrities and others.)
While criminal enforcement of HIPAA remains relatively rare and OCR to date only actually has assessed HIPAA civil monetary penalties against certain Covered Entities for violating HIPAA in a couple isolated instances, the growing list of multi-million dollar resolution payments against Covered Entities and with the FileFax Resolution Agreement announcement, now also business associates for violating HIPAA make clear that HIPAA enforcement is both meaningful and growing. See e.g., Learn From Children’s New $3.2M+ HIPAA CMP For “Knowing” Violation of HIPAA Security Rules ($3.2 million Children’s Medical Center HIPAA Civil Monetary Penalty); 1st HIPAA Privacy Civil Penalty of $4.3 Million Signals CMS Serious About HIPAA Enforcement; $400K HIPAA Settlement Shows Need To Conduct Timely & Appropriate Risk Assessments; $5.5M Memorial HIPAA Resolution Agreement Shows Need To Audit. For more examples, also see here.
The experiences of FileFax, Inc., CCDC, 21CO and these other OCR HIPAA Resolution Agreements provide strong evidence that that health plans and other Covered Entities and their business associates can anticipate that OCR will continue to zealously investigate HIPAA breaches and other HIPAA violations. Aside from OCR’s recurrent affirmations of its commitment to HIPAA enforcement, Covered Entities, their business associates and their leaders must recognize that public and Congressional privacy and data security concerns fueled by the ever growing stream of massive data breaches at Alteryx, eBay, Paypal owner TIO Networks, Uber, Equifax and a long list of other previously trusted prominent businesses are creating additional pressure upon OCR and other agencies to pursue even stronger and more aggressive HIPAA oversight and enforcement. Amid this growing concern, OCR, the FTC and other federal and state agencies with regulatory or enforcement authority over HIPAA or other data security and privacy concerns face increasing scrutiny and pressure to take meaningful action to regulate and enforce HIPAA and other laws intended to protect sensitive data even as private litigants enjoy increasing success in obtaining civil judgments from damages resulting from breaches of their PHI or other sensitive personal information using an expanding arsenal of legal theories of recovery. In the face of these growing concerns about privacy and data security, OCR can be expected to continue, if not increase its HIPAA compliance enforcement and oversight by OCR.
Furthermore, the experiences of FileFax, Inc., 21CO, CCDC and other Covered Entities and business associates that already have become the subject of OCR investigation or enforcement also reflect that HIPAA resolution payments or penalties paid to OCR and other costs and expenses associated with the defense and resolution of OCR’s investigations and enforcement actions typically only a portion of the financial and other business consequences that Covered Entities or business associates might expect to incur as a consequence of a breach of PHI or other substantial HIPAA violation or charge.
Beyond their potential HIPAA enforcement exposures following a HIPAA covered data breach or other violation, health care or other Covered Entities and members of their workforce experiencing breaches of ePHI or other PHI often also face FTC or other government investigations and enforcement relating their data breaches under the Fair and Accurate Credit Transactions Act (FACTA) and other federal or state identity theft, data privacy and security, electronic crimes and other laws. They or members of their workforce may face licensing board, credentialing, accreditation, contractual or other investigations or sanctions. Victims, business partners, investors and others often bring civil litigation to address losses or other injures associated with the breach or other misconduct. In addition, losses and disruptions in patients, plan member, vendor, investor, employee, management and other business relationships, and other business disruptions also are common.
Where the breach of other HIPAA violation involves a health plan, health plans, their fiduciaries and sponsors also need to give due consideration to the implications and exposures that might arise under the fiduciary responsibility rules of the Employee Retirement Income Security Act (ERISA). Beyond the direct exposure of their health plan to HIPAA and other compliance liabilities, health plan fiduciaries generally will want to consider whether their fiduciary responsibility under ERISA requires that prudent or other steps be taken to safeguard health plan information and maintain and administer their health plan in accordance with HIPAA and other laws. As a consequence, fiduciaries generally will want to ensure that they take and document prudent steps to evaluate, monitor and address HIPAA and other privacy and data security safeguards to minimize not only the liability exposures of their health plans, but also to help mitigate their own potential personal liability exposures that could arise or be asserted in response to a HIPAA breach or other HIPAA violation involving their health plans.
In the face of these growing risks and liabilities, Covered Entities and their business leaders face a strong imperative to clean up and maintain their HIPAA compliance and other data security to minimize their exposure to similar consequences. In addition to reaffirming the need for Covered Entities and their business associates to take the necessary steps to maintain and effectively demonstrate the adequacy of their own HIPAA compliance, the CCDC and FileFax Resolution Agreements alert Covered Entities and business associates of the advisability of greater oversight and risk management of their dealings and relationships with the other Covered Entities and business associates with access to or involvement with their PHI or other critical functions.
In light of these rises, leaders, investors, insurers, lenders and others involved with Covered Entities and their business associates should take steps to verify that the Covered Entities and their business associates not only maintain compliance with HIPAA and its business associate and other privacy, data security and breach notification and response requirements, but also maintain appropriate practices, insurance and other safeguards to prevent, respond to and mitigate exposures in the event of a breach of protected health information or other sensitive data. The bankruptcies and other financial and business fallout of HIPAA or other data breaches experienced by FileFax, Inc. 21CO and other HIPAA-covered and non-HIPAA regulated entities also makes clear that Covered Entities and business associates should anticipate that their own fallout from a breach or other HIPAA event and resulting responsibilities and consequences could be impacted by their own or a business associate’s financial distress or bankruptcy. Beyond the risk that their own or another entity’s breach, compliance issues, or other financial or business issues could trigger breach investigation, notice or other responsibilities for their own organizations, Covered Entities, business associates and their leaders also should evaluate and revise their HIPAA risk assessments and security plans to address foreseeable threats to the availability, access, retention and security of PHI and associated records and systems.
The Bankruptcy Court’s order to 21CO’s cyber liability insurer to pay the resolution payment required under the 21CO Resolution Agreement and other costs of investigation and defense also strongly suggests that the purchase of insurance and other arrangements for funding costs of defense or settlement should be included in these evaluations.
In light of these rises, leaders, investors, insurers, lenders and others involved with Covered Entities and their business associates should take steps to verify that the Covered Entities and their business associates not only maintain compliance with HIPAA, but also comply with data security, privacy and other information protection requirements arising under other laws, regulations, and contracts, as well as the practical business risks that typically follow the announcement of a breach. Considering these risks, Covered Entities and their business associates should recognize the advisability of taking meaningful, documented action to verify their existing compliance and ongoing oversight to ensure their organizations can demonstrate appropriate action to maintain appropriate practices, insurance and other safeguards to prevent, respond to and mitigate exposures in the event of a breach of protected health information or other sensitive data.
As part of these efforts, Covered Entities and their business associates should ensure that they have conducted, and maintain and are ready to produce appropriate policies and procedures backed up by a well-documented, up-to-date industry wide risk assessment of their organization’s susceptibility to breaches or other misuse of electronic or other protected health information. The starting point of these efforts should be to adopt and enforce updated written policies, procedures, technical and physical safeguards, processes and training to prevent the improper use, access, destruction or disclosure of patient PHI. Processes also should create, retain and be designed to cost effectively track, capture, and retain both all protected health information, its use, access, protection, destruction and disclosure, and the requisite supportive documentation supporting the appropriateness of those action to position the organization cost-effectively and quickly to fulfill required accounting, reporting and other needs in the event of a data breach, audit, participant inquiry or other event.
As part of this process, Covered Entities and business associates should maintain strong and ongoing processes for assessing and monitoring the adequacy of their policies and practices. In addition to ensuring that their organization has a comprehensive risk management and compliance assessment, Covered Entities and business associates need to conduct documented periodic audits and spot HIPAA audits and assessments. In doing so, they must use care to look outside the four corners of their Privacy Policies and core operating systems to ensure that their policies, practices, oversight and training address all protected health information within their operations on an entity wide basis. This entity-wide assessment should include communications and requests for information normally addressed to the Privacy Officer as well as requests and communications that could arise in the course of media or other public relations, practice transition, workforce communication and other operations not typically under the direct oversight and management of the Privacy Officer.
In connection with these efforts, the enforcement actions make clear that Covered Entities and business associates should adopt, implement and monitor PHI privacy, and security on an entity wide basis. These efforts should include general policies, practices and procedures as well as specifically tailored policies, processes and training to protect PHI and preserve HIPAA compliance throughout their organization. Testing and analysis should be conducted on a regular basis. Documented reassessments and testing should be performed in response to software, hardware or other changes or events that could impact security or other operations. Beyond security, attention also should cover business or system interruption including losses that might occur from the bankruptcy, termination of business or other disruptions of business associates or other parties. Attention should be paid both to protecting access and use of PHI and ePHI in the course of business as well as the transmission, transport, storage and destruction of records or systems containing such information.
Careful attention should be devoted to ensuring that business associate agreements as well and other processes provide for HIPAA compliance with respect to all PHI created, used, accessed or disclosed to business associates or others not part of their direct workforce or operating outside the core boundaries of their facilities.
Covered entities and their business associates also must recognize and design their compliance efforts and documentation recognizing that HIPAA compliance is a living process, which require both constant diligence about changes in systems or other events that may require reevaluation or adjustments, whether from changes in software, systems or processes or external threats.
Because the cost of responding to and investigating breaches or other compliance concern can be quite burdensome, Covered Entities and their business associates also generally will want to pursue options to plan for and minimize potential expenses in the design and administration of their programs as well as to minimize and cover the potentially extraordinary costs of breach or other compliance investigation and results that commonly arise following a breach or other compliance event. As a part of this planning, Covered Entities and their business associates also generally will want to add consideration of changes to federal tax rules on the deductibility of compliance penalty and other related compliance expenditures.
While the Internal Revenue Code traditionally has prohibited businesses and individuals from deducting penalties, fines and other expenditures arising from violations of federal or state laws under Section 162(f) of the Internal Revenue Code, Section 13306 of the Tax Cuts and Jobs Creation Act creates a new exception for amounts (other than amounts paid or incurred any amount paid or incurred as reimbursement to the government or entity for the costs of any investigation or litigation) that a taxpayer establishes meet the following requirements:
- Constitute restitution (including remediation of property) for damage or harm which was or may be caused by the violation of any law or the potential violation of any law, or
- Are paid to come into compliance with any law which was violated or otherwise involved in the investigation or inquiry into a violation or potential violation of any law;
- Are identified as restitution or as an amount paid to come into compliance with such law, as the case may be, in the court order or settlement agreement, and
- In the case of any amount of restitution for failure to pay any tax imposed under this title in the same manner as if such amount were such tax, would have been allowed as a deduction under this chapter if it had been timely paid.
Because the true effect of these modifications will be impacted by implementing regulations and a number of other special conditions and rules may impact the deductibility of these payments and the reporting obligations attached to their payment, Covered Entities will want to consult with legal counsel about these rules and monitor their implementation to understand their potential implications on compliance expenditures and penalties.
About The Author
Repeatedly recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, a Fellow in the American College of Employee Benefit Council, the American Bar Foundation and the Texas Bar Foundation and board certified in labor and employment law by the Texas Board of Legal Specialization, Cynthia Marcotte Stamer is a practicing attorney, management consultant, author, public policy advocate and lecturer widely known for health and managed care, employee benefits, insurance and financial services, data and technology and other management work, public policy leadership and advocacy, coaching, teachings, and publications. Nationally recognized for her work, experience, leadership and publications on HIPAA and other medical privacy and data use and security, FACTA, GLB, trade secrets and other privacy and data security concerns, Ms. Stamer has worked extensively with clients and the government on cybersecurity, technology and processes and other issues involved in the use and management of medical, insurance and other financial, workforce, trade secrets and other sensitive data and information throughout her career. Scribe or co-scribe of the ABA Joint Committee on Employee Benefits Agency meeting with OCR since 2011 and author of a multitude of highly regarded publications on HIPAA and other health care, insurance, financial and other privacy and data security, Ms. Stamer is widely known for her extensive and leading edge experience, advising, representing, training and coaching health care providers, health plans, healthcare clearinghouses, business associates, their information technology and other solutions providers and vendors, and others on HIPAA and other privacy, data security and cybersecurity design, documentation, administration, audit and oversight, business associate and other data and technology contracting, breach investigation and response, and other related concerns including extensive involvement representing clients in dealings with OCR and other Health & Human Services, Federal Trade Commission, Department of Labor, Department of Treasury, state health, insurance and attorneys’ general, Congress and state legislators and other federal officials.
Ms. Stamer also has an extensive contributes her leadership and insights with other professionals, industry leaders and lawmakers. Her insights on HIPAA risk management and compliance often appear in medical privacy related publications of a broad range of health care, health plan and other industry publications Among others, she has conducted privacy training for the Association of State & Territorial Health Plans (ASTHO), the Los Angeles Health Department, SHRM, HIMMS, the American Bar Association, the Health Care Compliance Association, a multitude of health plan, insurance and financial services, education, employer employee benefit and other clients, trade and professional associations and others. You can get more information about her HIPAA and other experience here. For additional information about Ms. Stamer, see here, e-mail her here or telephone Ms. Stamer at (214) 452-8297.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here including:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on OCR HIPAA Resolution Agreement Against Bankrupt Business Associate Signals Growing Exposures, Need for Tighter HIPAA Compliance By Health Plans & Business Associates |
Comments Off on OCR HIPAA Resolution Agreement Against Bankrupt Business Associate Signals Growing Exposures, Need for Tighter HIPAA Compliance By Health Plans & Business Associates |  Association Health Plan, board of directors, Brokers, church plan, Civil Monetary Penalties, Civil Rights, Claims Administration, Corporate Compliance, corporate governance, Cybercrime, Data Breach, Data Security, EBSA, employee, Employee Benefits, Employer, Employers, Employment, ERISA, FACTA, Fair Credit Reporting Act, fiduciary duty, Fiduciary Responsibility, GINA, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, health plan, Health Plans, HIPAA, HR, Human Resources, Identity Theft, Insurance, insurers, Internal Controls, Internal Investigations, Technology, third party administrators, Trade secret, Uncategorized | Tagged: Health Plans, HIPAA, Technology |
Association Health Plan, board of directors, Brokers, church plan, Civil Monetary Penalties, Civil Rights, Claims Administration, Corporate Compliance, corporate governance, Cybercrime, Data Breach, Data Security, EBSA, employee, Employee Benefits, Employer, Employers, Employment, ERISA, FACTA, Fair Credit Reporting Act, fiduciary duty, Fiduciary Responsibility, GINA, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, health plan, Health Plans, HIPAA, HR, Human Resources, Identity Theft, Insurance, insurers, Internal Controls, Internal Investigations, Technology, third party administrators, Trade secret, Uncategorized | Tagged: Health Plans, HIPAA, Technology |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
February 2, 2018
The $3.5 million payment that Fresenius Medical Care North America (FMCNA) is paying to the U.S. Department of Health and Human Services (HHS) Office for Civil Rights (OCR) to settle potential liability for potentially much higher Civil Monetary Penalties (CMPs) to OCR for Health Insurance Portability and Accountability Act (HIPAA) Privacy and Security Rules violation charges under a voluntary resolution agreement illustrates the need for group health plans and their employer and other sponsors, fiduciaries, and vendors to make HIPAA compliance a key priority for 2018.
Widespread publicity and fallout from data breaches involving Equifax, Blue Cross, the Internal Revenue Service and many other giant organizations have ramped up public awareness and government concern about health care and other data security. The resulting pressure is adding additional fuel to the already substantial concern of OCR and other agencies about compliance with HIPAA and other data security and breach laws. Like the $2.3 million HIPAA resolution agreement OCR announced with now bankrupt radiation oncology and cancer care provider 21st Century Oncology, Inc. (21CO) earlier this year, see, e.g., $23M Penalty Small Part of 21st Century’s Data Breach Fallout; Offers Data Breach Lessons For Other Businesses, the growing list of OCR resolution agreements and other enforcement actions against FMCNA, 21CO and other covered entities and other legal and market fallout that covered entities and other organizations experience following the announcement of breaches or other security deficiencies make the case for why HIPAA-covered health care providers, health plans, health care clearinghouses and their business associates (covered entities) must prioritize HIPAA compliance and other medical and other data security protection, privacy and risk management a top priority in 2018.
When weighing the importance of HIPAA compliance and risk management for their health plans, health plans, their employer or other sponsors, fiduciaries, insurers, administrators and their business associates should resist the temptation to underestimate the exposure because providers, rather than health plans, have been the most common target of the majority of the announced OCR enforcement actions resulting in substantial civil monetary penalties or resolution payments.
HIPAA Privacy, Security & Breach Notification Rule Responsibilities & Risks
The Privacy Rule requires that health plans, health care providers, health care clearinghouses (covered entities) and their vendors that qualify as “business associates” under HIPAA comply with detailed requirements concerning the protection, use, access, destruction and disclosure of protected health information. As part of these requirements, covered entities and their business associates must adopt, administer and enforce detailed policies and practices, assess, monitor and maintain the security of electronic protected health information (ePHI) and other protected health information, provide notices of privacy practices and breaches of “unsecured” ePHI, afford individuals that are the subject of protected health information certain rights and comply with other requirements as specified by the Privacy, Security and Breach Notification Rules. In addition, covered entities and business associates also must enter into a written and signed business associate agreement that contains the elements specified in Privacy Rule § 164.504(e) before the business associate creates, uses, accesses or discloses PHI of the covered entity. Furthermore, the Privacy Rule includes extensive documentation and keeping requirements require that covered entities and BAs maintain copies of these BAAs for a minimum of six years and to provide that documentation to OCR upon demand.
Violations of the Privacy Rule can carry stiff civil monetary penalties or even criminal penalties. Pursuant to amendments to HIPAA enacted as part of the HITECH Act, civil penalties typically do not apply to violations punished under the criminal penalty rules of HIPAA set forth in Social Security Act , 42 U.S.C § 1320d-6 (Section 1177).
Resolution Agreements like the $3.2 million FMCNA resolution agreement allow covered entities and business associates to resolve potentially substantially larger civil monetary penalty liabilities that OCR can impose under the civil enforcement provisions of HIPAA. As amended by the HITECH Act, the civil enforcement provisions of HIPAA empower OCR to impose Civil Monetary Penalties on both covered entities and BAs for violations of any of the requirements of the Privacy or Security Rules. The penalty ranges for civil violations depends upon the circumstances associated with the violations and are subject to upward adjustment for inflation. As most recently adjusted here effective September 6, 2016, the following currently are the progressively increasing Civil Monetary Penalty tiers:
- A minimum penalty of $100 and a maximum penalty of $50,000 per violation, for violations which the CE or BA “did not know, and by exercising reasonable diligence would not have known” about using “the business care and prudence expected from a person seeking to satisfy a legal requirement under similar circumstances;”
- A minimum penalty of $1,000 and a maximum penalty of $50,000 per violation, for violations for “reasonable cause” which do not rise to the level of “willful neglect” where “reasonable cause” means the “circumstances that would make it unreasonable for the covered entity, despite the exercise of ordinary business care and prudence, to comply with the violated Privacy Rule requirement;”
- A minimum penalty of $10,000 and a maximum penalty of $50,000 per violation, for violations attributed to “willful neglect,” defined as “the conscious, intentional failure or reckless indifference to the obligation to comply” with the requirement or prohibition; and
- A minimum penalty of $50,000 and a maximum penalty of $1.5 million per violation, for violations attributed to “willful neglect” not remedied within 30 days of the date that the covered entity or BA knew or should have known of the violation.
For continuing violations such as failing to implement a required BAA, OCR can treat each day of noncompliance as a separate violation. However, sanctions under each of these tiers generally are subject to a maximum penalty of $1,500,000 for violations of identical requirements or prohibitions during a calendar year. For violations such as the failure to implement and maintain a required BAA where more than one covered entity bears responsibility for the violation, OCR an impose Civil Monetary Penalties against each culpable party. OCR considers a variety of mitigating and aggravating facts and circumstances when arriving at the amount of the penalty within each of these applicable tiers to impose.
In addition to these potential civil liability exposures, covered entities, their business associates and other individuals or organizations that wrongfully use, access or disclose electronic or other protected health information also can face civil liability under various circumstances. The criminal enforcement provisions of HIPAA authorize the Justice Department to prosecute a person who knowingly in violation of the Privacy Rule (1) uses or causes to be used a unique health identifier; (2) obtains individually identifiable health information relating to an individual; or (3) discloses individually identifiable health information to another person, punishable by the following criminal sanctions and penalties:
- A fine of up to $50,000, imprisoned not more than 1 year, or both;
- If the offense is committed under false pretenses, a fine of up to $100,000, imprisonment of not more than 5 years, or both; and
- If the offense is committed with intent to sell, transfer, or use individually identifiable health information for commercial advantage, personal gain, or malicious harm, a fine of up to $250,000, imprisoned not more than 10 years, or both.
Because HIPAA Privacy Rule criminal violations are Class A Misdemeanors or felonies, Covered Entities and business associates should include HIPAA compliance in their Federal Sentencing Guideline Compliance Programs and practices and need to be concerned both about criminal exposure for their own direct violations, as well as imputed organizational liability for violations committed by their employees or agents under the Federal Sentencing Guidelines, particularly where their failure to implement or administer these required compliance policies and practices or failure to properly investigate or redress potential violations enables, perpetuates or covers up the criminal breach.
Fresenius Breach, Charges & Settlement Agreement Illustrate Civil Exposures
The FMCNA resolution agreement is another example of a growing list of resolution agreements various HIPAA covered entities have entered into to resolve their exposure to potentially greater liability should OCR assess civil monetary penalties under HIPAA’s civil sanction scheme.
The breach reports filed on January 21, 2017 reported five separate breach incidents occurring between February 23, 2012 and July 18, 2012 implicating the electronic protected health information (ePHI) of five separate FMCNA owned covered entities (FMCNA covered entities): Bio-Medical Applications of Florida, Inc. d/b/a Fresenius Medical Care Duval Facility in Jacksonville, Florida (FMC Duval Facility); Bio-Medical Applications of Alabama, Inc. d/b/a Fresenius Medical Care Magnolia Grove in Semmes, Alabama (FMC Magnolia Grove Facility); Renal Dimensions, LLC d/b/a Fresenius Medical Care Ak-Chin in Maricopa, Arizona (FMC Ak-Chin Facility); Fresenius Vascular Care Augusta, LLC (FVC Augusta); and WSKC Dialysis Services, Inc. d/b/a Fresenius Medical Care Blue Island Dialysis (FMC Blue Island Facility).
OCR concluded its investigation showed the breaches resulted because FMCNA failed to conduct an accurate and thorough risk analysis of potential risks and vulnerabilities to the confidentiality, integrity, and availability of all of its ePHI. OCR also concluded:
- The FMCNA covered entities impermissibly disclosed the ePHI of patients by providing unauthorized access for a purpose not permitted by the Privacy Rule.
- FMC Ak-Chin failed to implement policies and procedures to address security incidents.
- FMC Magnolia Grove failed to implement policies and procedures that govern the receipt and removal of hardware and electronic media that contain ePHI into and out of a facility; and the movement of these items within the facility.
- FMC Duval and FMC Blue Island failed to implement policies and procedures to safeguard their facilities and equipment therein from unauthorized access, tampering, and theft, when it was reasonable and appropriate to do so under the circumstances.
- FMC Magnolia Grove and FVC Augusta failed to implement a mechanism to encrypt and decrypt ePHI, when it was reasonable and appropriate to do so under the circumstances.
In addition to a $3.5 million monetary settlement, a corrective action plan requires the FMCNA covered entities to complete a risk analysis and risk management plan, revise policies and procedures on device and media controls as well as facility access controls, develop an encryption report, and educate its workforce on policies and procedures.
HIPAA & Data Breach Enforcement A Growing Health Plan Risk
Health plans and other covered entities, plan sponsors and plan fiduciaries, their business associates and other consultants and service providers and members of their workforce need to recognize that the FMCNA and other resolution agreements are part of a growing trend, rather than isolated incidents of enforcement.
While civil monetary penalty enforcement remains much more common than criminal prosecution, covered entities, their business associates and members of their workforce must understand that HIPAA enforcement and resulting liability is growing.
While Department of Justice federal criminal prosecutions and convictions under HIPAA remain relatively rare, they occur and are growing. See e.g., Former Hospital Employee Sentenced for HIPAA Violations (Texas man sentenced to 18 months in federal prison for obtaining protected health information with the intent to use it for personal gain); Three Life Sentences Imposed On Man Following Convictions For Drug Trafficking, Kidnapping, Using Firearms and HIPAA Violations (drug king pin gets multiple 10 year consecutive prison terms for unauthorized access to private health information in violation of HIPAA; his health care worker friend sentenced for accessing electronic medical files and reporting information to him); Former Therapist Charged In HIPAA Case; Hefty Prison Sentence in ID Theft Case (former assisted living facility worker gets 37 months in prison after pleading guilty to wrongful disclosure of HIPAA protected information and other charges); Hefty Prison Sentence in ID Theft Case (former medical supply company owner sentenced to 12 years for HIPAA violations and fraud). While the harshest sentences tend to be associated with health care fraud or other criminal conduct, lighter criminal sentences are imposed against defendants in other cases as well. See e.g., Sentencing In S.C. Medicaid Breach Case (former South Carolina state employee sentenced to three years’ probation, plus community service, for sending personal information about more than 228,000 Medicaid recipients to his personal e-mail account.); HIPAA Violation Leads To Prison Term (former UCLA Healthcare System surgeon gets four months in prison after admitting he illegally read private electronic medical records of celebrities and others.)
While criminal enforcement of HIPAA remains relatively rare and OCR to date only actually has assessed HIPAA civil monetary penalties against certain Covered Entities for violating HIPAA in a couple isolated instances, the growing list of multi-million dollar resolution payments that FMCNA and other covered entities caught violating HIPAA make clear that HIPAA enforcement is both meaningful and growing. See e.g., Learn From Children’s New $3.2M+ HIPAA CMP For “Knowing” Violation of HIPAA Security Rules ($3.2 million Children’s Medical Center HIPAA Civil Monetary Penalty); 1st HIPAA Privacy Civil Penalty of $4.3 Million Signals CMS Serious About HIPAA Enforcement; $400K HIPAA Settlement Shows Need To Conduct Timely & Appropriate Risk Assessments; $5.5M Memorial HIPAA Resolution Agreement Shows Need To Audit. For more examples, also see here.
Beyond the direct exposure of their health plan to HIPAA and other compliance liabilities, health plan fiduciaries also should note that their fiduciary responsibility under the Employee Retirement Income Security Act (ERISA) likely includes taking prudent steps to safeguard health plan information and maintain and administer their health plan in accordance with HIPAA. As a consequence, fiduciaries generally will want to ensure that they take and document prudent steps to evaluate, monitor and address HIPAA and other privacy and data security safeguards to minimize not only the liability exposures of their health plans, but also to help mitigate their own potential personal liability exposures that could arise or be asserted in response to a HIPAA breach or other HIPAA violation involving their health plans.
Coming on the heels of an already lengthy and growing list of OCR high dollar HIPAA enforcement actions, the FMCNA and other resolution agreements and civil monetary penalties these and other announced enforcement actions clearly reflect that OCR takes HIPAA compliance seriously and stands ready to impose substantial penalties when it finds violations in connection with breach notice investigations. Viewed in the context of these and other enforcement actions, the FMCNA Resolution Agreement and others clearly reflect the time for complacency in HIPAA compliance and leniency in HIPAA HIPAA enforcement are passed. Rather, these and other enforcement actions make clear why health care providers, health plans, healthcare clearinghouses and their business associates must make HIPAA compliance a priority now.
Covered entities and business associates also should recognize their potential responsibilities and risks for breaches or other improper conduct concerning patient or other sensitive personal financial information, trade secrets or other data under a wide range of laws beyond HIPAA and its state law equivalents. As documented by the media coverage of the legal and business woes of Alteryx, eBay, Paypal owner TIO Networks, Uber, Equifax and a long list of other previously trusted prominent businesses have and continue to incur from data breaches within their organizations, health care or other covered entities experiencing breaches often also face FTC or other government investigations and enforcement under the Fair and Accurate Credit Transactions Act (FACTA) and other federal or state identity theft, data privacy and security, electronic crimes and other rules as well as business losses and disruptions; civil litigation from breach victims, shareholders and investors, and business partners as well as OCR, FTC, and state data security regulation enforcement. Amid this growing concern, OCR has indicated that it intends to continue to diligently both seek to support and encourage voluntary compliance by covered entities and their business associates and investigate and enforce HIPAA against HIPAA covered entities and their business associates that fail to adequately safeguard PHI and ePHI in accordance with HIPAA. In the face of these growing risks and liabilities, covered entities and their business leaders face a strong imperative to clean up and maintain their HIPAA compliance and other data security to minimize their exposure to similar consequences.
In light of these rises, leaders, investors, insurers, lenders and others involved with covered entities and their business associates should take steps to verify that the covered entities and their business associates not only maintain compliance with HIPAA, but also comply with data security, privacy and other information protection requirements arising under other laws, regulations, and contracts, as well as the practical business risks that typically follow the announcement of a breach. Considering these risks, covered entities and their business associates must recognize and take meaningful, documented action to verify their existing compliance and ongoing oversight to ensure their organizations can demonstrate appropriate action to maintain appropriate practices, insurance and other safeguards to prevent, respond to and mitigate exposures in the event of a breach of protected health information or other sensitive data.
In response to these growing risks and concerns, covered entities and their business associates should ensure that they have conducted, and maintain and are ready to produce appropriate policies and procedures backed up by a well documented, up-to-date industry wide risk assessment of their organization’s susceptibility to breaches or other misuse of electronic or other protected health information. The starting point of these efforts should be to adopt and enforce updated written policies, procedures, technical and physical safeguards, processes and training to prevent the improper use, access, destruction or disclosure of patient PHI. Processes also should create, retain and be designed to cost effectively track, capture, and retain both all protected health information, its use, access, protection, destruction and disclosure, and the requisite supportive documentation supporting the appropriateness of those action to position the organization cost-effectively and quickly to fulfill required accounting, reporting and other needs in the event of a data breach, audit, participant inquiry or other event.
As part of this process, covered entities and business associates should start by reviewing and updating their policies, HIPAA audits and assessments and other documentation and processes. In doing so, they must use care to look outside the four corners of their Privacy Policies and core operating systems to ensure that their policies, practices, oversight and training address all protected health information within their operations on an entity wide basis. This entity-wide assessment should include both communications and requests for information normally addressed to the Privacy Officer as well as requests and communications that could arise in the course of media or other public relations, practice transition, workforce communication and other operations not typically under the direct oversight and management of the Privacy Officer.
In connection with these efforts, the enforcement actions make clear that Covered Entities and business associates should adopt, implement and monitor PHI privacy, and security on an entity wide basis. These efforts should include both general policies, practices and procedures as well as specifically tailored policies, processes and training to protect PHI and preserve HIPAA compliance throughout their organization as well as the business associate agreements and other processes to provide for HIPAA compliance with respect to protected health information created, used, accessed or disclosed to business associates or others not part of their direct workforce or operating outside the core boundaries of their facilities.
Covered entities and their business associates also must recognize and design their compliance efforts and documentation recognizing that HIPAA compliance is a living process, which require both constant diligence about changes in systems or other events that may require reevaluation or adjustments, whether from changes in software, systems or processes or external threats.
Because the cost of responding to and investigating breaches or other compliance concern can be quite burdensome, covered entities and their business associates also generally will want to pursue options to plan for and minimize potential expenses in the design and administration of their programs as well as to minimize and cover the potentially extraordinary costs of breach or other compliance investigation and results that commonly arise following a breach or other compliance event. As a part of this planning, covered entities and their business associates also generally will want to add consideration of changes to federal tax rules on the deductibility of compliance penalty and other related compliance expenditures.
While the Internal Revenue Code traditionally has prohibited businesses and individuals from deducting penalties, fines and other expenditures arising from violations of federal or state laws under Section 162(f) of the Internal Revenue Code, Section 13306 of the Tax Cuts and Jobs Creation Act creates a new exception for amounts (other than amounts paid or incurred any amount paid or incurred as reimbursement to the government or entity for the costs of any investigation or litigation) that a taxpayer establishes meet the following requirements:
- Constitute restitution (including remediation of property) for damage or harm which was or may be caused by the violation of any law or the potential violation of any law, or
- Are paid to come into compliance with any law which was violated or otherwise involved in the investigation or inquiry into a violation or potential violation of any law;
- Are identified as restitution or as an amount paid to come into compliance with such law, as the case may be, in the court order or settlement agreement, and
- In the case of any amount of restitution for failure to pay any tax imposed under this title in the same manner as if such amount were such tax, would have been allowed as a deduction under this chapter if it had been timely paid.
Because the true effect of these modifications will be impacted by implementing regulations and a number of other special conditions and rules may impact the deductibility of these payments and the reporting obligations attached to their payment, covered entities will want to consult with legal counsel about these rules and monitor their implementation to understand their potential implications on compliance expenditures and penalties.
About The Author
Repeatedly recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, a Fellow in the American College of Employee Benefit Council, the American Bar Foundation and the Texas Bar Foundation and board certified in labor and employment law by the Texas Board of Legal Specialization, Cynthia Marcotte Stamer is a practicing attorney, management consultant, author, public policy advocate and lecturer widely known for health and managed care, employee benefits, insurance and financial services, data and technology and other management work, public policy leadership and advocacy, coaching, teachings, and publications. Nationally recognized for her work, experience, leadership and publications on HIPAA and other medical privacy and data use and security, FACTA, GLB, trade secrets and other privacy and data security concerns, Ms. Stamer has worked extensively with clients and the government on cybersecurity, technology and processes and other issues involved in the use and management of medical, insurance and other financial, workforce, trade secrets and other sensitive data and information throughout her career. Scribe or co-scribe of the ABA Joint Committee on Employee Benefits Agency meeting with OCR since 2011 and author of a multitude of highly regarded publications on HIPAA and other health care, insurance, financial and other privacy and data security, Ms. Stamer is widely known for her extensive and leading edge experience, advising, representing, training and coaching health care providers, health plans, healthcare clearinghouses, business associates, their information technology and other solutions providers and vendors, and others on HIPAA and other privacy, data security and cybersecurity design, documentation, administration, audit and oversight, business associate and other data and technology contracting, breach investigation and response, and other related concerns including extensive involvement representing clients in dealings with OCR and other Health & Human Services, Federal Trade Commission, Department of Labor, Department of Treasury, state health, insurance and attorneys’ general, Congress and state legislators and other federal officials.
Ms. Stamer also has an extensive contributes her leadership and insights with other professionals, industry leaders and lawmakers. Her insights on HIPAA risk management and compliance often appear in medical privacy related publications of a broad range of health care, health plan and other industry publications Among others, she has conducted privacy training for the Association of State & Territorial Health Plans (ASTHO), the Los Angeles Health Department, SHRM, HIMMS, the American Bar Association, the Health Care Compliance Association, a multitude of health plan, insurance and financial services, education, employer employee benefit and other clients, trade and professional associations and others. You can get more information about her HIPAA and other experience here. For additional information about Ms. Stamer, see here, e-mail her here or telephone Ms. Stamer at (214) 452-8297.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources here including:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please be sure that we have your current contact information including your preferred e-mail by creating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice or an offer or commitment to provide legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as legal advice or an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on $3.5M HIPAA Settlement Highlights Need To Prioritize Health Plan HIPAA Compliance in 2018 |
Comments Off on $3.5M HIPAA Settlement Highlights Need To Prioritize Health Plan HIPAA Compliance in 2018 |  Association Health Plan, board of directors, Brokers, church plan, Civil Monetary Penalties, Civil Rights, Claims Administration, Corporate Compliance, corporate governance, Cybercrime, Data Breach, Data Security, EBSA, employee, Employee Benefits, Employer, Employers, Employment, ERISA, FACTA, Fair Credit Reporting Act, fiduciary duty, Fiduciary Responsibility, GINA, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, health plan, Health Plans, HIPAA, HR, Human Resources, Identity Theft, Insurance, insurers, Internal Controls, Internal Investigations, Technology, third party administrators, Trade secret, Uncategorized | Tagged: Health Plans, HIPAA, Technology |
Association Health Plan, board of directors, Brokers, church plan, Civil Monetary Penalties, Civil Rights, Claims Administration, Corporate Compliance, corporate governance, Cybercrime, Data Breach, Data Security, EBSA, employee, Employee Benefits, Employer, Employers, Employment, ERISA, FACTA, Fair Credit Reporting Act, fiduciary duty, Fiduciary Responsibility, GINA, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, health plan, Health Plans, HIPAA, HR, Human Resources, Identity Theft, Insurance, insurers, Internal Controls, Internal Investigations, Technology, third party administrators, Trade secret, Uncategorized | Tagged: Health Plans, HIPAA, Technology |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
January 30, 2018
Businesses with employees that travel regularly or for the occasional training or other isolated business trip should review and update their travel related policies, practices, and procedures for evolving laws, risks and management needs.
To start with, 2017 tax reforms impact the tax treatment of various employee relocation and travel related expense. Businesses should review these changes and make appropriate updates now to avoid headaches for the business and its employees later.
While many employers mostly focus upon travel expense management, reporting and reimbursement, smart employers also understand there’s much more to consider.
First and foremost, since employees often forget that the purpose of business travel is carrying out the business of the company and not a boondoggle, business travel policies and communications should make clear to employees that their trip is about work. Policies should make clear to employees their tesponsibility for attending meetings and performing other business-related responsibilities as well as for conducting themselves at all times consistent with company policy and to promote a positive impression of the employer and the company.
Naturally all travel policies also should require compliance with all applicable laws and customs. For international travel, this includes compliance with the Foreign Corrupt Practices Act, the Patriot Act, U.S. and foreign immigration and customs, and other relevant laws, rules and customs. However, domestic travelers also should be reminded if their duty to comply with local laws as well.
Amid the current “Me Too” frenzy, however, companies also should consider addressing other potentially risky behavior that tends to arise when employees travel on business. Unfortunately history proves that many employees actually do need to be told and reminded to abstain from inappropriate alcohol, sexual harassment or other behavior that could create liability or embarrassment for the company when traveling for business or engaging in other activities. Because business travel tends to blur distinctions between business and personal time, most businesses will want to establish and communicate high expectations concerning on and off-duty conduct when traveling on business to head off potential problems. Updated direction about hosting or participating in entertainment and other social activities with co-workers, customers, vendors, prospects and others also often are warranted.
Beyond communicating expectations of employees while on business travel, businesses also should confirm their company’s compensation, expense reimbursement, timekeeping and reporting, hours of work, and other policies comply with current laws and capture and retain appropriate documentation.
Businesses must recognize, for instance, that training and other work related travel typically is considered hours of work for wage an hour, safety and various other purposes. Employers should confirm their policies and practices properly capture and count all required hours of compensable work and pay hourly workers for time on the road properly in accordance with Labor Department requirements. Many employers unfortunately get nailed for overtime violations because of assumptions or misunderstandings of rules. For instance, many employers improperly fail to count air travel and certain other travel time as compensable when required to do so under Labor Department Fair Labor Standards Act (FLSA) rules. Likewise, improperly structured expense reimbursement policies or practices can bump up overtime pay liability by requiring the employer to include otherwise excludable expense reimbursements payments in the hourly rate of pay when calculating regular and overtime pay. Employers must ensure they understand these rules and take appropriate steps to capture, track, report and pay for time and expenses upfront to defend an audit or other challenge effectively and efficiently.
Reviewing and tightening workforce travel related policies, practices and procedures to meet current laws, business and social expectations and management needs can boost the bang businesses realize for their business travel buck while mitigating a host of legal and business risks.
About The Author
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation; Former Chair of the RPTE Employee Benefits and Compensation Committee, a current Co-Chair of the Committee, and the former Chair of its Welfare Benefit and its Defined Compensation Plan Committees and former RPTE Joint Committee on Employee Benefits Council (JCEB) Representative, Cynthia Marcotte Stamer is a Martindale-Hubble “AV-Preeminent” practicing attorney and management consultant, author, public policy advocate, author and lecturer repeatedly recognized for her 30 plus years’ of work and pragmatic thought leadership, publications and training on health, pension and other employee benefit, insurance, labor and employment, and health care fiduciary responsibility, payment, investment, contracting and other design, administration and compliance concerns as among the “Top Rated Labor & Employment Lawyers in Texas,” a “Legal Leader,” a “Top Woman Lawyer” and with other awards by LexisNexis® Martindale-Hubbell®; as among the “Best Lawyers In Dallas” for her work in the field of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, in International Who’s Who of Professionals and with numerous other awards and distinctions.
Highly valued for her ability to meld her extensive legal and industry knowledge and experience with her talents as an insightful innovator and pragmatic problem solver, Ms. Stamer advises, represents and defends employer, union, multi-employer, association and other employee benefit plan sponsors, insurers and managed care organizations, fiduciaries, plan administrators, technology and other service providers, government and community leaders and others about health and other employee benefit and insurance program and policy design and innovation, funding, documentation, administration, communication, data security and use, contracting, plan, public and regulatory reforms and enforcement, and other risk management, compliance and operations matters. Her experience encompasses leading and supporting the development and defense of innovative new policies, programs, practices and solutions; advising and representing clients on routine plan establishment, plan documentation and contract drafting and review, administration, change and other compliance and operations; crisis prevention and response, compliance and risk management audits and investigations, enforcement actions and other dealings with the US Congress, Departments of Labor, Treasury, Health & Human Services, Federal Trade Commission, Justice, Securities and Exchange Commission, Education and other federal agencies, state legislatures, attorneys general, insurance, labor, worker’s compensation, and other agencies and regulators, and various other foreign and domestic governmental bodies and agencies. She also provides strategic and other supports clients in defending litigation as lead strategy counsel, special counsel and as an expert witness. Alongside her extensive legal and operational experience, Ms. Stamer also is recognized for her work as a public and regulatory policy advocate and community leader with a gift for finding pragmatic solutions and helping to forge the common ground necessary to build consensus. Best known for her domestic public policy and community leadership on health care and insurance reform, Ms. Stamer’s lifelong public policy and community service involvement includes service as a lead consultant to the Government of Bolivia on its pension privatization project, as well as extensive legislative and regulatory reform, advocacy and input workforce, worker classification, employee benefit, public health and healthcare, social security and other disability and aging in place, education, migration reforms domestically and internationally throughout her adult life. In addition to her public and regulatory policy involvement, Ms. Stamer also contributes her service and leadership to a professional and civic organizations and efforts including her involvement as the Founder and Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE; Coalition on Patient Empowerment, a founding Board Member and past President of the Alliance for Healthcare Excellence; Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; Vice Chair, Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group; current Fiduciary Responsibility Committee Co-Chair and Membership Committee member of the ABA RPTE Section; former RPTE Employee Benefits and Other Compensation Group Chair, former Chair and Co-Chair of its Welfare Plans Committee, and Defined Contribution Plans Committee; former RPTE Representative to ABA Joint Committee on Employee Benefits Council; former RPTE Representative to the ABA Health Law Coordinating Counsel; former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, former Board Member, Continuing Education Chair and Treasurer of the Southwest Benefits Association; Vice President of the North Texas Healthcare Compliance Professionals Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; past Dallas World Affairs Council Board Member, and in leadership of many other professional, civic and community organizations. Ms. Stamer also is a highly popular lecturer, symposia chair and author, who publishes and speaks extensively on health and managed care industry, human resources, employment and other privacy, data security and other technology, regulatory and operational risk management for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, the Society of Professional Benefits Administrators, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients, serves on the faculty and planning committee of many workshops, seminars, and symposia, and on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Beyond these involvements, Ms. Stamer also is active in the leadership of a broad range of other public policy advocacy and other professional and civic organizations and involvements. Through these and other involvements, she helps develop and build solutions, build consensus, garner funding and other resources, manage compliance and other operations, and take other actions to identify promote tangible improvements in health care and other policy and operational areas.
Before founding her current law firm, Cynthia Marcotte Stamer, P.C., Ms. Stamer practiced law as a partner with several prominent national and international law firms for more than 10 years before founding Cynthia Marcotte Stamer, P.C. to practice her unique brand of “Solutions law™” and to devote more time to the pragmatic policy and system reform, community education and innovation, and other health system improvement efforts of her PROJECT COPE: the Coalition on Patient Empowerment initiative.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com such as the following
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved
 Comments Off on Time To Tighten Business Travel Policies |
Comments Off on Time To Tighten Business Travel Policies |  Absenteeism, Affirmative Action, board of directors, Brokers, business travel, Civil Rights, compensation, compliance, conflict of interest, Corporate Compliance, corporate governance, directors, Discrimination, Drug & Alcohol, E-Verify, Education, EEOC, EEOC, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Agreement, Employment Discrimination, Employment Policies, enforcement, Executive Compensation, Fair Labor Standards Act, FICA, FLSA, Fringe Benefit, Government Contractors, Hiring, HR, Human Resources, I-9, Immigration, Insurance, Internal Controls, Internal Investigations, Internal Revenue Code, IRC, Labor Management Relations, Leadership, Management, Nonresident aliens, occupational safety, OSHA, Overtime, Pay, Payroll Tax, Risk Management, Sexual Harassment, Telecommuting, Uncategorized, visas, Wage & Hour, Whistleblower, Worker Classification, Workforce |
Absenteeism, Affirmative Action, board of directors, Brokers, business travel, Civil Rights, compensation, compliance, conflict of interest, Corporate Compliance, corporate governance, directors, Discrimination, Drug & Alcohol, E-Verify, Education, EEOC, EEOC, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Agreement, Employment Discrimination, Employment Policies, enforcement, Executive Compensation, Fair Labor Standards Act, FICA, FLSA, Fringe Benefit, Government Contractors, Hiring, HR, Human Resources, I-9, Immigration, Insurance, Internal Controls, Internal Investigations, Internal Revenue Code, IRC, Labor Management Relations, Leadership, Management, Nonresident aliens, occupational safety, OSHA, Overtime, Pay, Payroll Tax, Risk Management, Sexual Harassment, Telecommuting, Uncategorized, visas, Wage & Hour, Whistleblower, Worker Classification, Workforce |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
January 24, 2018
Department of Labor (DOL) and other agencies’ spending reports posted at USASpending.gov to comply withthe Digital Accountability and Transparency Act of 2014 (DATA Act) are intended to help taxpayers, government leaders and others monitor and evaluate agency spending. However a new report from the DOL Office of Inspector General (OIG) found data reporting and other issues have compromised the reliability of the data reported in DOL reports posed on USASpending.gov.
The Data Act requires federal agencies to report spending data in accordance with new government-wide data standards developed by the Office of Management and Budget (OMB) and the Department of Treasury (Treasury). The data reports are posted on so taxpayers and policy makers understand how the Department is spending its funds. The Act requires federal agencies to report spending data in accordance with new government-wide data standards developed by the Office of Management and Budget (OMB) and the Department of Treasury (Treasury). The Act also requires the Inspectors General of each federal agency to conduct a review of the agency’s DATA Act compliance every two years and report on the completeness, timeliness, accuracy, and quality of the agency’s data.
The new report reports OIG’s findings from a performance audit OIG performed to assess: (1) the completeness, timeliness, accuracy, and quality of data submitted by the Department; and (2) the Department’s implementation and use of the Government-wide data standards established by OMB and Treasury for the Fiscal Year 2017 second quarter. While OIG found DOL effectively implemented and used the Government-wide data standards established by OMB and Treasury to prepare the reports and timely submitted the DATA Act required reports, it found numerous issues with the overall quality of the spending data it submitted for publication on USAspending.gov. Among other things, OIG reports that DOL:
- Did not report all the required data elements for 19 percent of the transactions sampled. OIG found 77% of these errors occurred because the Department did not include Unique Record Identifiers for transactions when it was required to. This could cause issues when linking financial data with grant data on USAspending.gov.
- 74% of the transactions sampled contained an error in one or more data elements. OIG reports many of these errors resulted from issues in the Treasury’s DATA Act broker data extraction process.
- Excluding those errors, 52% of the transactions sampled contained inaccurate information.
- In addition to errors uncovered from OIG’s sampling audit, DOL also reported inaccurate program activity and object class codes for 5 and 7 percent of transactions, respectively, in its File B submission.
OIG attributes these errors in accuracy and completeness occurred because of data entry mistakes, data extraction issues, and weak data validation processes and concluded that these control deficiencies will have a negative impact on the quality of the data DOL reports until corrected.
Based on these findings, OIG has made eight recommendations to DOL’s Principal Deputy Chief Financial Officer to improve the quality of the data the DOL reports to USAspending.gov in the future and to strengthen internal controls over its data management processes.
While OIG reports DOL has concurred with these recommendations and has stated it has implemented additional controls, resulting in fewer errors with each submission, taxpayers and others using past reports need to consider the reported deficiencies in their evaluation and use of the data as well as assess the validity of future reported data for possible issues for future assessments. Even considering these issues, however, taxpayers and government leaders should consider consulting the data when investigating or evaluating DOL or other program activities or expenditures for policy, enforcement priority or other purposes.
About The Author
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation; Former Chair of the RPTE Employee Benefits and Compensation Committee, a current Co-Chair of the Committee, and the former Chair of its Welfare Benefit and its Defined Compensation Plan Committees and former RPTE Joint Committee on Employee Benefits Council (JCEB) Representative, Cynthia Marcotte Stamer is a Martindale-Hubble “AV-Preeminent” practicing attorney and management consultant, author, public policy advocate, author and lecturer repeatedly recognized for her 30 plus years’ of work and pragmatic thought leadership, publications and training on health, pension and other employee benefit, insurance, labor and employment, and health care fiduciary responsibility, payment, investment, contracting and other design, administration and compliance concerns as among the “Top Rated Labor & Employment Lawyers in Texas,” a “Legal Leader,” a “Top Woman Lawyer” and with other awards by LexisNexis® Martindale-Hubbell®; as among the “Best Lawyers In Dallas” for her work in the field of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, in International Who’s Who of Professionals and with numerous other awards and distinctions.
Highly valued for her ability to meld her extensive legal and industry knowledge and experience with her talents as an insightful innovator and pragmatic problem solver, Ms. Stamer advises, represents and defends employer, union, multi-employer, association and other employee benefit plan sponsors, insurers and managed care organizations, fiduciaries, plan administrators, technology and other service providers, government and community leaders and others about health and other employee benefit and insurance program and policy design and innovation, funding, documentation, administration, communication, data security and use, contracting, plan, public and regulatory reforms and enforcement, and other risk management, compliance and operations matters. Her experience encompasses leading and supporting the development and defense of innovative new policies, programs, practices and solutions; advising and representing clients on routine plan establishment, plan documentation and contract drafting and review, administration, change and other compliance and operations; crisis prevention and response, compliance and risk management audits and investigations, enforcement actions and other dealings with the US Congress, Departments of Labor, Treasury, Health & Human Services, Federal Trade Commission, Justice, Securities and Exchange Commission, Education and other federal agencies, state legislatures, attorneys general, insurance, labor, worker’s compensation, and other agencies and regulators, and various other foreign and domestic governmental bodies and agencies. She also provides strategic and other supports clients in defending litigation as lead strategy counsel, special counsel and as an expert witness. Alongside her extensive legal and operational experience, Ms. Stamer also is recognized for her work as a public and regulatory policy advocate and community leader with a gift for finding pragmatic solutions and helping to forge the common ground necessary to build consensus. Best known for her domestic public policy and community leadership on health care and insurance reform, Ms. Stamer’s lifelong public policy and community service involvement includes service as a lead consultant to the Government of Bolivia on its pension privatization project, as well as extensive legislative and regulatory reform, advocacy and input workforce, worker classification, employee benefit, public health and healthcare, social security and other disability and aging in place, education, migration reforms domestically and internationally throughout her adult life. In addition to her public and regulatory policy involvement, Ms. Stamer also contributes her service and leadership to a professional and civic organizations and efforts including her involvement as the Founder and Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE; Coalition on Patient Empowerment, a founding Board Member and past President of the Alliance for Healthcare Excellence; Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; Vice Chair, Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group; current Fiduciary Responsibility Committee Co-Chair and Membership Committee member of the ABA RPTE Section; former RPTE Employee Benefits and Other Compensation Group Chair, former Chair and Co-Chair of its Welfare Plans Committee, and Defined Contribution Plans Committee; former RPTE Representative to ABA Joint Committee on Employee Benefits Council; former RPTE Representative to the ABA Health Law Coordinating Counsel; former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, former Board Member, Continuing Education Chair and Treasurer of the Southwest Benefits Association; Vice President of the North Texas Healthcare Compliance Professionals Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; past Dallas World Affairs Council Board Member, and in leadership of many other professional, civic and community organizations. Ms. Stamer also is a highly popular lecturer, symposia chair and author, who publishes and speaks extensively on health and managed care industry, human resources, employment and other privacy, data security and other technology, regulatory and operational risk management for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, the Society of Professional Benefits Administrators, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients, serves on the faculty and planning committee of many workshops, seminars, and symposia, and on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Beyond these involvements, Ms. Stamer also is active in the leadership of a broad range of other public policy advocacy and other professional and civic organizations and involvements. Through these and other involvements, she helps develop and build solutions, build consensus, garner funding and other resources, manage compliance and other operations, and take other actions to identify promote tangible improvements in health care and other policy and operational areas.
Before founding her current law firm, Cynthia Marcotte Stamer, P.C., Ms. Stamer practiced law as a partner with several prominent national and international law firms for more than 10 years before founding Cynthia Marcotte Stamer, P.C. to practice her unique brand of “Solutions law™” and to devote more time to the pragmatic policy and system reform, community education and innovation, and other health system improvement efforts of her PROJECT COPE: the Coalition on Patient Empowerment initiative.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com such as the following:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on DOL Spending Reports Required As Taxpayer Tool Need Improvement |
Comments Off on DOL Spending Reports Required As Taxpayer Tool Need Improvement |  401(k), Civil Rights, Claims Administration, COBRA, compensation, compliance, Corporate Compliance, corporate governance, Defined Benefit Plans, Defined Contribution Plans, Discrimination, Disease Management, Drug & Alcohol, EBSA, EEOC, employee, Employee Benefits, Employer, Employers, Employment, Employment Discrimination, Employment Policies, enforcement, ERISA, Executive Compensation, Fair Labor Standards Act, family leave, fiduciary duty, Fiduciary Responsibility, FLSA, Government Accountability, Government Contractors, h-2A Visa, Health Benefits, health insurance, health insurance marketplace, health plan, Health Plans, HR, Human Resources, Insurance, insurers, Internal Controls, Labor Management Relations, LEP, LGBT, Management, medical leave, Mental Health, MEWA, Military Leave, mine safety, MSHA, NLRA, Obamacare, occupational safety, officers, OSHA, Overtime, Patient Empowerment, Pay, pension plan, Plan Admistrator, Prescription Drugs, Public Policy, Reporting & Disclosure, Retirement Plans, Retirements, Sexual Harassment, Unfair Labor Practice, Union, VEVRAA, Wellness Programs |
401(k), Civil Rights, Claims Administration, COBRA, compensation, compliance, Corporate Compliance, corporate governance, Defined Benefit Plans, Defined Contribution Plans, Discrimination, Disease Management, Drug & Alcohol, EBSA, EEOC, employee, Employee Benefits, Employer, Employers, Employment, Employment Discrimination, Employment Policies, enforcement, ERISA, Executive Compensation, Fair Labor Standards Act, family leave, fiduciary duty, Fiduciary Responsibility, FLSA, Government Accountability, Government Contractors, h-2A Visa, Health Benefits, health insurance, health insurance marketplace, health plan, Health Plans, HR, Human Resources, Insurance, insurers, Internal Controls, Labor Management Relations, LEP, LGBT, Management, medical leave, Mental Health, MEWA, Military Leave, mine safety, MSHA, NLRA, Obamacare, occupational safety, officers, OSHA, Overtime, Patient Empowerment, Pay, pension plan, Plan Admistrator, Prescription Drugs, Public Policy, Reporting & Disclosure, Retirement Plans, Retirements, Sexual Harassment, Unfair Labor Practice, Union, VEVRAA, Wellness Programs |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
January 17, 2018
Health plans, their employer, union, insurer or other sponsors, fiduciaries, administrative or other service providers and their vendors and advisors should act immediately to investigate if any action is needed to protect electronic protected health information or other sensitive data and systems in response to the following cyber risk alert from the Department Of Health and Human Services Office of Civil Rights.

TLP: WHITE: ASPR/CIP HPH Cyber Notice: Meltdown and Spectre Vulnerability Guidance UPDATE #1
January 17, 2018
DISCLAIMER: This product is provided “as is” for informational purposes only. The Department of Health and Human Services (HHS) does not provide warranties of any kind regarding any information contained within. HHS does not endorse any commercial product or service referenced in this product or otherwise. Further dissemination of this product is governed by the Traffic Light Protocol (TLP) marking in the header.
TLP: WHITE information may be distributed without restriction (subject to standard copyright rules).
Healthcare and Public Health Sector partners-
The attached report is a technical update to the previously distributed HPH Cyber Notice covering chip vulnerabilities named Meltdown and Spectre. Both Meltdown and Spectre are vulnerabilities in how computer chips handle data that have the potential to expose sensitive information, such as protected health information (PHI), being processed on the chip. As this information is protected from disclosure under HIPAA, Healthcare and Public Health (HPH) entities should employ risk management processes to address these vulnerabilities and ensure the security of medical records and other PHI.
Major concerns for the HPH sector include but are not limited to:
• Challenges identifying vulnerable medical devices and accessory medical equipment and ensuring patches are validated to prevent impacts to the intended use.
• Cloud Computing: Potential PHI or Personally Identifiable Information (PII) data leakage in shared computing environments
• Web browsers: Possible PHI/PII data leakage
• Patches: Potential for service degradation and/or interruption from patches
The detailed report can be found here: Technical Report on Widespread Processor Vulnerabilities
 Comments Off on Check & Protect Health & Other Electronic Systems & Data Against New Security Threat |
Comments Off on Check & Protect Health & Other Electronic Systems & Data Against New Security Threat |  4980D, ADA, Association Health Plan, board of directors, Brokers, Civil Rights, compliance, Corporate Compliance, Cybercrime, Data Breach, Data Security, directors, Disease Management, Electronic Medical Record, Employee Benefits, Employer, Employers, ERISA, exchange, Fiduciary Responsibility, GINA, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, health plan, Health Plans, HIPAA, Uncategorized |
4980D, ADA, Association Health Plan, board of directors, Brokers, Civil Rights, compliance, Corporate Compliance, Cybercrime, Data Breach, Data Security, directors, Disease Management, Electronic Medical Record, Employee Benefits, Employer, Employers, ERISA, exchange, Fiduciary Responsibility, GINA, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, health plan, Health Plans, HIPAA, Uncategorized |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
January 10, 2018
Employer and sponsors, fiduciaries, administrators and insurers of employee benefitplansof any type covered by the Employee Retirement Income Security Act (ERISA) making any disability based determinations now have until April 1, 2018 to bring their plans’ claims and appeals procedures for disability-based decisions and related notices and communications into compliance with substantially more complicated requirements in new Department of Labor Employee Benefit Security Administration (EBSA) regulations.
The EBSA announced on January 5, 2018 the extension of the effective date of new requirements for benefit plan processing and providing notification about claims or appeals involving disability determinations from their originally scheduled effective date of January 1, 2018 to April 1, 2018.
While the extension gives employer and other sponsors, fiduciaries, administrators and insurers of employee benefit plans making disability-based benefit determinations a few extra months to review and update their plan documents, summary plan descriptions, procedures, processes and claims and appeals notices to meet tightened new federal rules on disability-based benefit determinations applicable to all post December 31, 2017 claims under the restated Final Rule on Claims Procedure for Plans Providing Disability Benefits (“Disability Claims Rule”), the nature and scope of these new requirements will require updates to virtually all ERISA-covered benefit plans with any disability dependent provisions. These updates are likely to include changes to plan documents, summary plan descriptions, notices, contracts, processes and procedures for a broad range of plans. Consequently, employer and other plan sponsors, fiduciaries, administrators, insurers and others responsible for any benefit plan not already reviewed and updated to comply should get moving to complete the necessary review and update to meet the April 1, 2018 deadline.
Cynthia Marcotte Stamer and others will lead a free telephone study group discussion of “Claims Regulations and Other Developments Affecting Plan Fiduciaries” on January 26, 2018 beginning at 1 PM (Eastern), Noon (Central), 11 AM (Mountain), and 10 AM (Pacific). For more details about the Study Group, see here.
New Disability Claims Rule Overview
Originally published in final form by the EBSA on December 16, 2016, the Disability Claims Rule generally require all ERISA-covered employee benefit plans making any disability benefit or other determination conditioned upon a finding of disability to comply with the new Disability Claims Rule for any claim received after March 31, 2018.
Based on EBSA’s previously adopted Patient Protection and Affordable Care Act (“ACA”) group health plan claims and appeals rules, the new Final Disability Claims Rule will apply to all disability determinations made under any ERISA-covered plan after March 31, 2018, regardless of how the plan characterizes the benefit or whether the plan is a health or other welfare, pension, 401(k) plan or other savings plan.
The new Disability Claims Rule will apply to a broad range of plans, most of which historically have not followed the detailed claims and appeals notification, independent and impartial decision-making, rescission, deemed exhaustion, “culturally and linguistically appropriate” and other procedural protections and safeguards that the Disability Claims Rule extends from the current group health plan rules to all ERISA-covered plans making benefit determinations based on disability. Consequently covered plans making disability-based benefit or other covered determinations are likely to require updates to plan documents, insurance or administrative services contracts, summary plan descriptions and other plan communications, claims and appeals notices, and other related processes, procedures and documentation to meet these new requirements. Since certain requirements of the Disability Claims Rules like the summary plan description advance disclosure requirements are required to be provided before the claim is received, plans and their sponsors, fiduciaries, insurers and administrators risk being accused of violating these requirements by waiting to update plans, their processes and materials until after claim involving a disability based determination arises.
Ensuring that impacted plans are updated before the April 1, 2018 deadline is important because the Disability Claims Rule, like the group health plan claims and appeals rules upon which it is based, also states that noncompliance with any of its requirements empowers a participant to immediately sue the plan for enforcement if his rights without further complying the the plan’s administrative procedures. Moreover, failing to comply with summary plan disclosure or claims or appeal adverse benefit determination notification requirements also may subject the plan administrator to administrative penalties under ERISA section 514(c); fiduciaries to ERISA fiduciary liability, and compromise the ability to defend otherwise defensible decisions. Consequently, employers and other plan sponsors, fiduciaries, administrators and insurers will want to act quickly to ensure that their plans, their summary plan descriptions and other communications, notices, processes, contracts and procedures are updated appropriately before April 1, 218.
About The Author
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation; Former Chair of the RPTE Employee Benefits and Compensation Committee, a current Co-Chair of the Committee, and the former Chair of its Welfare Benefit and its Defined Compensation Plan Committees and former RPTE Joint Committee on Employee Benefits Council (JCEB) Representative, Cynthia Marcotte Stamer is a Martindale-Hubble “AV-Preeminent” practicing attorney and management consultant, author, public policy advocate, author and lecturer repeatedly recognized for her 30 plus years’ of work and pragmatic thought leadership, publications and training on health, pension and other employee benefit, insurance, labor and employment, and health care fiduciary responsibility, payment, investment, contracting and other design, administration and compliance concerns as among the “Top Rated Labor & Employment Lawyers in Texas,” a “Legal Leader,” a “Top Woman Lawyer” and with other awards by LexisNexis® Martindale-Hubbell®; as among the “Best Lawyers In Dallas” for her work in the field of “Labor & Employment,” “Tax: ERISA & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, in International Who’s Who of Professionals and with numerous other awards and distinctions.
Highly valued for her ability to meld her extensive legal and industry knowledge and experience with her talents as an insightful innovator and pragmatic problem solver, Ms. Stamer advises, represents and defends employer, union, multi-employer, association and other employee benefit plan sponsors, insurers and managed care organizations, fiduciaries, plan administrators, technology and other service providers, government and community leaders and others about health and other employee benefit and insurance program and policy design and innovation, funding, documentation, administration, communication, data security and use, contracting, plan, public and regulatory reforms and enforcement, and other risk management, compliance and operations matters. Her experience encompasses leading and supporting the development and defense of innovative new policies, programs, practices and solutions; advising and representing clients on routine plan establishment, plan documentation and contract drafting and review, administration, change and other compliance and operations; crisis prevention and response, compliance and risk management audits and investigations, enforcement actions and other dealings with the US Congress, Departments of Labor, Treasury, Health & Human Services, Federal Trade Commission, Justice, Securities and Exchange Commission, Education and other federal agencies, state legislatures, attorneys general, insurance, labor, worker’s compensation, and other agencies and regulators, and various other foreign and domestic governmental bodies and agencies. She also provides strategic and other supports clients in defending litigation as lead strategy counsel, special counsel and as an expert witness. Alongside her extensive legal and operational experience, Ms. Stamer also is recognized for her work as a public and regulatory policy advocate and community leader with a gift for finding pragmatic solutions and helping to forge the common ground necessary to build consensus. Best known for her domestic public policy and community leadership on health care and insurance reform, Ms. Stamer’s lifelong public policy and community service involvement includes service as a lead consultant to the Government of Bolivia on its pension privatization project, as well as extensive legislative and regulatory reform, advocacy and input workforce, worker classification, employee benefit, public health and healthcare, social security and other disability and aging in place, education, migration reforms domestically and internationally throughout her adult life. In addition to her public and regulatory policy involvement, Ms. Stamer also contributes her service and leadership to a professional and civic organizations and efforts including her involvement as the Founder and Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE; Coalition on Patient Empowerment, a founding Board Member and past President of the Alliance for Healthcare Excellence; Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; Vice Chair, Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Interest Group; current Fiduciary Responsibility Committee Co-Chair and Membership Committee member of the ABA RPTE Section; former RPTE Employee Benefits and Other Compensation Group Chair, former Chair and Co-Chair of its Welfare Plans Committee, and Defined Contribution Plans Committee; former RPTE Representative to ABA Joint Committee on Employee Benefits Council; former RPTE Representative to the ABA Health Law Coordinating Counsel; former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, former Board Member, Continuing Education Chair and Treasurer of the Southwest Benefits Association; Vice President of the North Texas Healthcare Compliance Professionals Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; past Dallas World Affairs Council Board Member, and in leadership of many other professional, civic and community organizations. Ms. Stamer also is a highly popular lecturer, symposia chair and author, who publishes and speaks extensively on health and managed care industry, human resources, employment and other privacy, data security and other technology, regulatory and operational risk management for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, the Society of Professional Benefits Administrators, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients, serves on the faculty and planning committee of many workshops, seminars, and symposia, and on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Beyond these involvements, Ms. Stamer also is active in the leadership of a broad range of other public policy advocacy and other professional and civic organizations and involvements. Through these and other involvements, she helps develop and build solutions, build consensus, garner funding and other resources, manage compliance and other operations, and take other actions to identify promote tangible improvements in health care and other policy and operational areas.
Before founding her current law firm, Cynthia Marcotte Stamer, P.C., Ms. Stamer practiced law as a partner with several prominent national and international law firms for more than 10 years before founding Cynthia Marcotte Stamer, P.C. to practice her unique brand of “Solutions law™” and to devote more time to the pragmatic policy and system reform, community education and innovation, and other health system improvement efforts of her PROJECT COPE: the Coalition on Patient Empowerment initiative.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com such as the following:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2018 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on April 1 New Deadline To Update Benefit Plan Disability Determination Claims & Appeals Procesures; Hear More on 1/26 |
Comments Off on April 1 New Deadline To Update Benefit Plan Disability Determination Claims & Appeals Procesures; Hear More on 1/26 |  401(k), ACA, Accommodation, Civil Rights, Claims Administration, COBRA, compensation, compliance, Corporate Compliance, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, Disability, Disability Plans, Disease Management, Drug & Alcohol, EBSA, Employee Benefits, Employer, Employers, Employment, Employment Policies, ERISA, Executive Compensation, family leave, fiduciary duty, Fiduciary Responsibility, Health Benefits, health insurance, health plan, Health Plans, HR, Human Resources, Insurance, insurers, Internal Controls, Labor Management Relations, medical leave, Mental Health, Patient Empowerment, pension plan, Prescription Drugs, Reporting & Disclosure, Retirement Plans, Retirements, Uncategorized, Union, Wellness Programs |
401(k), ACA, Accommodation, Civil Rights, Claims Administration, COBRA, compensation, compliance, Corporate Compliance, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, Disability, Disability Plans, Disease Management, Drug & Alcohol, EBSA, Employee Benefits, Employer, Employers, Employment, Employment Policies, ERISA, Executive Compensation, family leave, fiduciary duty, Fiduciary Responsibility, Health Benefits, health insurance, health plan, Health Plans, HR, Human Resources, Insurance, insurers, Internal Controls, Labor Management Relations, medical leave, Mental Health, Patient Empowerment, pension plan, Prescription Drugs, Reporting & Disclosure, Retirement Plans, Retirements, Uncategorized, Union, Wellness Programs |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
January 5, 2018
Continuing Fallout of 2015 Data Breach Provides Many Lessons For Other Businesses & Their Health Plans
Read the rest of this entry »
 Comments Off on $23M Penalty Small Part of 21st Century’s Data Breach Fallout; Offers Data Breach Lessons For Other Businesses |
Comments Off on $23M Penalty Small Part of 21st Century’s Data Breach Fallout; Offers Data Breach Lessons For Other Businesses |  ADA, Association Health Plan, Banking, Bankruptcy, board of directors, Brokers, Cafeteria Plans, Civil Monetary Penalties, Claims Administration, compensation, compliance, Consumer Protection, Corporate Compliance, corporate governance, Cybercrime, Data Breach, Data Security, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, Disability, EBSA, employee, Employee Benefits, Employer, Employers, Employment, Employment Policies, ERISA, Excise Taxes, FACTA, Fiduciary Responsibility, Form 5500, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, health plan, Health Plans, HIPAA, HR, Human Resources, Identity Theft, Internal Revenue Code, IRC, Labor Management Relations, Management, Mental Health, Pay, pension plan, Reporting & Disclosure, retirement plan, Retirement Plans, Retirements, Salaried, Tax, Uncategorized | Tagged: Cyber Security, Cybercrime, Data Breach, HIPAA, Identity Theft, Privacy, Technology |
ADA, Association Health Plan, Banking, Bankruptcy, board of directors, Brokers, Cafeteria Plans, Civil Monetary Penalties, Claims Administration, compensation, compliance, Consumer Protection, Corporate Compliance, corporate governance, Cybercrime, Data Breach, Data Security, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, Disability, EBSA, employee, Employee Benefits, Employer, Employers, Employment, Employment Policies, ERISA, Excise Taxes, FACTA, Fiduciary Responsibility, Form 5500, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, health plan, Health Plans, HIPAA, HR, Human Resources, Identity Theft, Internal Revenue Code, IRC, Labor Management Relations, Management, Mental Health, Pay, pension plan, Reporting & Disclosure, retirement plan, Retirement Plans, Retirements, Salaried, Tax, Uncategorized | Tagged: Cyber Security, Cybercrime, Data Breach, HIPAA, Identity Theft, Privacy, Technology |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
December 18, 2017
Want to know what tax changes are included in the Tax Cuts and Jobs Act (H.R. 1) (Act”) and expected to pass Congress tomorrow (December 20, 2017)? Check out the House Conference Committee Report, H. Rept. 115-466 (the “Conference Report”) released on Friday, December 15, 2017.
The House Conference Committee Report details the negotiated reconciliation of House Bill (H.R. 1) as passed by the House of Representatives on November 16, 2017 and the provisions of H.R. 1 with amendments passed by the Senate on December 2, 2017. Over the past few weeks, a joint committee made up of key representatives from the House and Senate have engaged in highly publicized negotiations to reconcile differences in the House and Senate versions of the Act. The House Conference Committee Report signed off by the Conference Committee and filed in the House of Representatives of December 15, 2017 documents the agreements reached by House and Senate Conferees reconciling the House and Senate versions of H.R. 1, which Congress will vote upon this week. Solutions Law Press, Inc. will publish analysis of various provisions of these reforms over the next few days. In the meantime, taxpayers interested in learning about the Act may use the links in this article to begin familiarizing themselves with its provisions.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
Well-known for her extensive work with health, insurance, financial services, technology, energy, manufacturing, retail, hospitality, governmental and other highly regulated employers, her nearly 30 years’ of experience encompasses work with domestic and international businesses of all types and sizes as well as extensive work with Congress and U.S. federal and state regulatory agencies on workforce, compensation and benefits, and performance and operational compliance challenges. A primary drafter of the Bolivian Pension Privitization law who also has worked on workforce, tax, employee benefits, health care, insurance, safety, immigration, privacy and data security and other federal and state legal reforms domestically and internationally throughout her adult life, Ms. Stamer also has been extensively involved in various aspects of Congressional considerations of the current Act and other legislation considered by the current Congress.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations, for clients and others.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com such as the following:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2017 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved
 Comments Off on Read Tax Cuts and Jobs Act Conference Report For Tax Reform From Source |
Comments Off on Read Tax Cuts and Jobs Act Conference Report For Tax Reform From Source |  105(h), 401(k), 5000, Cafeteria Plans, church plan, compensation, compliance, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, EBSA, employee, Employee Benefits, Employer, Employers, Employment, Employment Agreement, Employment Tax, ESOP, Excise Tax, Excise Taxes, Executive Compensation, Exempt, Form 5500, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, health plan, Health Plans, HR, Human Resources, Income Tax, Insurance, insurers, IRC, Management, Obamacare, Patient Protection & Affordable Care Act, Patient Protection and Affordabel Care Act, Patient Protection and Affordable Care Act, Pay, Payroll Tax, pension plan, Premium Subsidies, retirement plan, Retirement Plans, Risk Management, Social Security, Tax, Tax Credit, Tax Qualification, Uncategorized | Tagged: tax reform, Taxes |
105(h), 401(k), 5000, Cafeteria Plans, church plan, compensation, compliance, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, EBSA, employee, Employee Benefits, Employer, Employers, Employment, Employment Agreement, Employment Tax, ESOP, Excise Tax, Excise Taxes, Executive Compensation, Exempt, Form 5500, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, health plan, Health Plans, HR, Human Resources, Income Tax, Insurance, insurers, IRC, Management, Obamacare, Patient Protection & Affordable Care Act, Patient Protection and Affordabel Care Act, Patient Protection and Affordable Care Act, Pay, Payroll Tax, pension plan, Premium Subsidies, retirement plan, Retirement Plans, Risk Management, Social Security, Tax, Tax Credit, Tax Qualification, Uncategorized | Tagged: tax reform, Taxes |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
December 18, 2017
Employers, employee benefit plan sponsors and administrators, vendors and their advisors and service providers should re-evaluate their existing payroll and other settings and elections, planning, testing and related strategies and assumptions in light of the 2018 annual cost-of-living adjustments (COLAs) to the dollar limitations applicable to the Internal Revenue Code Section 415 qualified retirement plans benefit and contribution limits announced by the Internal Revenue Service (IRS) in Notice 2017-64, IRB 2017-45 on November 6, 2017.
H.R. 1, Tax Cuts and Jobs Act (Tax Refirm Bill) reported out of the Conference Committee last week and scheduled for a vote before Congress tomorrow leaves these limits substantially unchanged.
Notice 2017-64 adjusts the dollar limitations applicable to the Internal Revenue Code Section 415 qualified retirement plans benefit and contribution limits. The Section 415 limitations COLAs are made and published annually to comply with Section 415(d)’s requirement that the Treasury Security annually adjust these limits for cost-of-living increases. Other limitations applicable to deferred compensation plans are also affected by these adjustments under § 415. Under § 415(d), the adjustments are to be made under adjustment procedures similar to those used to adjust benefit amounts under § 215(i)(2)(A) of the Social Security Act.
In addition to impacting contribution limits permitted to defined benefit, 401(k) and other defined contribution and other plans, the changes can impact the definition of highly compensated employees, discrimination testing, plan funding and a broad range of employee benefit, compensation, tax, payroll, union or other contracting and other concerns for employers, employee benefit plan sponsors, fiduciaries, administrators, payroll, plan and other vendors, participants and beneficiaries and others.
The following is a chart of the adjusted limits compared to the currently applicable 2017 limitations. (Download chart)
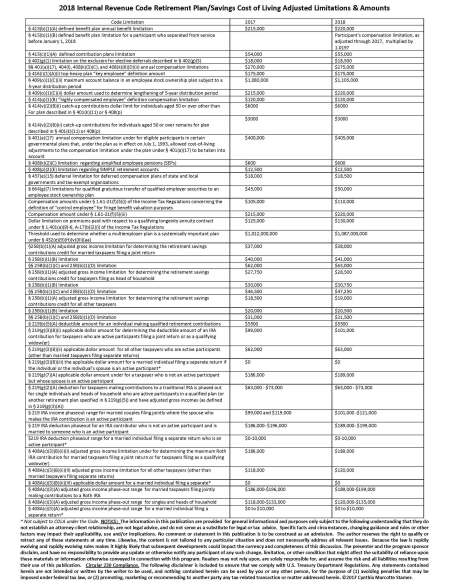
Employers, employee benefit plan sponsors, fiduciaries, administrators and other vendors, participants and beneficiaries and others working with employee benefit plans or compensation contributed to these arrangements should review these new 2018 COLA limitations to assess their potential impact and make appropriate adjustments to avoid compliance challenges or other unfortunate surprises in 2018. If they already have not already done so, reviewing the 2018 Social Security Act COLAs also would be wise. See 2018 Social Security COLAs Set.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
Well-known for her extensive work with health, insurance, financial services, technology, energy, manufacturing, retail, hospitality, governmental and other highly regulated employers, her nearly 30 years’ of experience encompasses domestic and international businesses of all types and sizes.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com such as the following:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2017 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved
 Comments Off on Check How IRS 2018 Retirement & Saving Plan Limits and Amounts Cost Of Living Adjustments Impact Your HR & Retirement Plan Administration & Planning |
Comments Off on Check How IRS 2018 Retirement & Saving Plan Limits and Amounts Cost Of Living Adjustments Impact Your HR & Retirement Plan Administration & Planning |  401(k), Association Health Plan, Brokers, compensation, compliance, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, Disability, Disability Plans, employee, Employee Benefits, Employer, Employers, Employment, Employment Policies, Employment Tax, ERISA, ESOP, Excise Taxes, Form 5500, Health Plans, HR, Human Resources, Internal Revenue Code, IRC, Labor Management Relations, Management, Pay, pension plan, Reporting & Disclosure, retirement plan, Retirement Plans, Retirements, Salaried, Tax, Uncategorized |
401(k), Association Health Plan, Brokers, compensation, compliance, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, Disability, Disability Plans, employee, Employee Benefits, Employer, Employers, Employment, Employment Policies, Employment Tax, ERISA, ESOP, Excise Taxes, Form 5500, Health Plans, HR, Human Resources, Internal Revenue Code, IRC, Labor Management Relations, Management, Pay, pension plan, Reporting & Disclosure, retirement plan, Retirement Plans, Retirements, Salaried, Tax, Uncategorized |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
December 14, 2017
Employer and other sponsors, fiduciaries, administrators and insurers of the Employee Retirement Income Security Act (ERISA)-covered employee benefit plans making disability-based benefit determinations should confirm that their plan documents, summary plan descriptions, procedures and claims and appeals notices are updated and ready to meet tightened new federal rules on disability-based benefit determinations applicable to all post December 31, 2017 claims under the restated Final Rule on Claims Procedure for Plans Providing Disability Benefits (“Disability Claims Rule”). Given the nature and scope of these new requirements, most covered plans will require specific action be taken before the new rules take effect to update plan documents, summary plan descriptions, notices, contracts, processes and procedures to meet the January 1, 2018 deadline.
The Disability Claims Rule published by the Department of Labor Employee Benefit Security Administration (“EBSA”) on December 19, 2016 generally require all ERISA-covered employee benefit plans making any disability benefit or other determination conditioned upon a finding of disability to comply with the new Disability Claims Rule for any claim received after December 31, 2017.
The new Final Disability Claims Rule will apply to all disability determinations made under any ERISA-covered plan after December 31, 2017, regardless of how the plan characterizes the benefit or whether the plan is a health or other welfare, pension, 401(k) plan or other savings plan.
Significant affirmative action is likely required to prepare covered plans to meet these requirements since most plans historically have not followed the detailed claims and appeals notification, independent and impartial decision-making, rescission, deemed exhaustion, “culturally and linguistically appropriate” and other procedural protections and safeguards based on EBSA’s previously adopted Patient Protection and Affordable Care Act (“ACA”) group health plan claims and appeals rules, which the Disability Claims Rules extend and make applicable to all ERISA-covered plans making benefit determinations based on disability. Covered plans making disability-based benefit or other covered determinations are likely to require updates to plan documents, insurance or administrative services contracts, summary plan descriptions and other plan communications, claims and appeals notices, and other related processes, procedures and documentation to meet these new requirements. Since certain requirements of the Disability Claims Rules like the summary plan description advance disclosure requirements are required to be provided before the claim is received, plans and their sponsors risk being accused of violating these requirements by waiting to update plans, their processes and materials until after claim involving a disability based determination arises.
Ensuring that impacted plans are updated before the January 1, 2018 deadline is important because the Disability Claims Rule, like the group health plan claims and appeals rules upon which it is based, also states that noncompliance with any of its requirements empowers a participant to immediately sue the plan for enforcement if his rights without further complying the the plan’s administrative procedures. Moreover, failing to comply with summary plan disclosure or claims or appeal adverse benefit determination notification requirements also may subject the plan administrator to administrative penalties under ERISA section 514(c). Consequently, employers and other plan sponsors, fiduciaries, administrators and insurers will want to act quickly to ensure that their plans, their summary plan descriptions and other communications, notices, processes, contracts and procedures are updated appropriately before January 1, 2018.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
Well-known for her extensive work with health, insurance, financial services, technology, energy, manufacturing, retail, hospitality, governmental and other highly regulated employers, her nearly 30 years’ of experience encompasses domestic and international businesses of all types and sizes.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediatepast RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, BenefitsMagazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com such as the following:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2017 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on Confirm Your Benefit Plans Ready For New Disability Determination Rules on 1/1/18 |
Comments Off on Confirm Your Benefit Plans Ready For New Disability Determination Rules on 1/1/18 |  401(k), ACA, ADA, Affordable Care Act, Appeals, board of directors, Brokers, Cafeteria Plans, Claims, Claims Administration, compensation, compliance, Construction, Corporate Compliance, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, directors, Disability, Disability, Disability Plans, Drug & Alcohol, EBSA, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Policies, ERISA, Executive Compensation, family leave, Fiduciary Responsibility, health benefit, Health Benefits, health insurance, Leave, Management, medical leave, Mental Health, Mental Health Parity, Obamacare, Patient Protection & Affordable Care Act, Pay, pension plan, Plan Admistrator, Professional Liability, third party administrators, Uncategorized, Union, Worker | Tagged: Appeals, Claims, defined benefit plan, Disability, Disability Insurance, Disability Plan, EBSA, Employee Retirement Income Security act, ERISA, Fiduciary Responsibility, pension plan |
401(k), ACA, ADA, Affordable Care Act, Appeals, board of directors, Brokers, Cafeteria Plans, Claims, Claims Administration, compensation, compliance, Construction, Corporate Compliance, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, directors, Disability, Disability, Disability Plans, Drug & Alcohol, EBSA, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Policies, ERISA, Executive Compensation, family leave, Fiduciary Responsibility, health benefit, Health Benefits, health insurance, Leave, Management, medical leave, Mental Health, Mental Health Parity, Obamacare, Patient Protection & Affordable Care Act, Pay, pension plan, Plan Admistrator, Professional Liability, third party administrators, Uncategorized, Union, Worker | Tagged: Appeals, Claims, defined benefit plan, Disability, Disability Insurance, Disability Plan, EBSA, Employee Retirement Income Security act, ERISA, Fiduciary Responsibility, pension plan |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
December 13, 2017
 Teamwork is a valuable and necessary to organizational performance in most workplaces. However management undermines team performance and effectiveness by giving participation trophies to team members that don’t give their best when working on teams.
Teamwork is a valuable and necessary to organizational performance in most workplaces. However management undermines team performance and effectiveness by giving participation trophies to team members that don’t give their best when working on teams.
Managements goal at all-time should be to maximize the effectiveness of the team by encouraging and require each individual team member to contribute their best on the team.
Overemphasizing team work at the expense of individual performance accountability, however, undermines team performance by disincentivizing optimal performance by every team member. Optimal management and performance rewards ensure that each individual member of the team remains accountable for optimizing his or her individual performance while encouraging effective participation on the team. To maintain individual performance within the team, ensure your expectations and performance measures track not only team performance but also individual performance on the team. Measure and award teamwork by individual members of the team as one of the performance measures rather than making teamwork itself at the expense of the performance goals the basis of the reward.
Check out this coach’s perspective for more food for thought.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
Well-known for her extensive work with health, insurance, financial services, technology, energy, manufacturing, retail, hospitality, governmental and other highly regulated employers, her nearly 30 years’ of experience encompasses domestic and international businesses of all types and sizes.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com such as the following:
▪DOL Proposes Changing FLSA Tipped Employee Pay Rules
▪Consider Internal Investigation & Defense Costs When Administering Compliance Programs
▪Recruiting Qualified Workers Biggest Challenge US Manufacturers See In Otherwise Optimistic 3rd Quarter 2017
▪Government Retirees Get New Thrift Plan Distributing Choices
▪Jennifer A. Abruzzo Named NLRB Acting General Counsel
▪Bill Mandating E-Verify, Raising Employer I-9 Penalties Approved By House Judiciary Committee
▪Address Workplace Harassment During October Stop Bullying Month
▪NIOSH Proposed Updated Occupational Safety Chemical Monitoring Rules
▪2018 Social Security COLAs Set
▪IRS Updates Defined Benefit Plan Guidance
▪Read Trump Health Care Executive Order
▪Dealing With HR, Benefits & Other Headaches From Equifax and Other Data Breach
▪Employers Should Manage Potential Unfair Labor Practice Risks From Recording, Acceptable Use, Fighting, Integrity & Other Employment Policies
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2017 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved
 Comments Off on Individual Accountability For Performance Matters |
Comments Off on Individual Accountability For Performance Matters |  compensation, compliance, Corporate Compliance, corporate governance, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Policies, Executive Compensation, Hiring, HR, Human Resources, Internal Controls, Management, Pay, Uncategorized |
compensation, compliance, Corporate Compliance, corporate governance, employee, Employee Benefits, Employee Handbook, Employer, Employers, Employment, Employment Policies, Executive Compensation, Hiring, HR, Human Resources, Internal Controls, Management, Pay, Uncategorized |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
December 12, 2017
The Internal Revenue Service (“IRS”) is acting to help Patient Protection and Affordable Care Act (“Obamacare”) health subsidy-eligible individuals living in regions where exchange insurers do not offer bronze (lowest cost) coverage even as it moves ahead to nail employers failing to comply with Obamacare’s employer shared responsibility rules (commonly referred to as the “employer mandate”). The move comes as House and Senate Conferees are preparing to conference to work out differences in the tax bill which could repeal the Obamacare individual mandate penalty for failing to maintain coverage while leaving intact penalties against employers violating the employer mandate by failing to offer affordable minimum essential coverage as well as other Obamacare penalties on plans and their employers.
IRS New Individual Obamacare Relief
Notice 2017-74 will provide that Individuals who are not eligible for coverage under an eligible employer-sponsored plan and who lack access to affordable coverage should not be denied the use of the affordability exemption under § 5000A(e)(1) of the Code and § 1.5000A-3(e) of the Regulations merely because they reside in an area served by a Marketplace that does not offer a bronze-level plan. Consequently, for purposes of the affordability exemption under § 5000A(e)(1) and § 1.5000A-3(e), if an individual resides in a rating area served by a Marketplace that does not offer a bronze plan, the individual generally should use as his or her applicable plan the lowest cost metal-level plan available in the Marketplace serving the rating area in which the individual resides.
Notice 2017-74 will be in IRB 2017-51, dated December 18, 2017.
Employer’s Still Face Obamacare Penalties
While the IRS has issued limited relief for individuals from the ACA’s individual mandate penalties, so far it has remained steadfast in its refusal to grant employers corresponding relief from the ACA employer shared responsibility penalties or other ACA penalties. Instead, IRS officials continue to make clear that the IRS intends to enforce the ACA employer shared responsibility rules against employers with 50 or more full-time employees (including full-time equivalent employees) (“covered employers”).
Under the Obamacare employer mandate rules, covered employers face significant Federal tax penalties for (1) failing to offer minimal essential coverage to substantially all full-time employees and their dependents (the “A Penalty”), or (2) offering coverage that is either “unaffordable” or does not provide “minimum value” (the “B Penalty”) (referred to collectively as the “ACA Penalties”) if a full-time employee enrolls in the Health Insurance Marketplace (the “Exchange”) and receives a Premium Tax Credit.
While many employers assumed President Trump’s January 20, 2017 Executive Order Executive Order Minimizing the Economic Burden of the Patient Protection and Affordable Care Act Pending Repeal would insulate them against enforcement of the employer mandate and other Obamacare penalties, the IRS doesn’t see the Executive Order as barring its enforcement of Obamacare against sponsoring employers or their group health plans. An April 14, 2017 IRS Chief Counsel letter, for instance, the IRS announced it does not interpret its discretionary authority under Obamacare to allow waiver of the employer mandate tax imposed under Internal Revenue Code Section 4980H against covered employers that fail to provide the affordable minimum essential coverage required by the employer mandate. In keeping with this interpretation, the IRS has announced that it will begin enforcement of the employer mandate tax liability for plan years after 2015 against covered employers that failed to meet the employer mandate.
Of course, the employer mandate is not the only Obama care provision that employers and their health plans need to worry about. In addition to the employer mandate, Obamacare imposed a host of patient protection and other federal mandates upon employer-sponsored plans, most of which apply to plans covering two or more employees. In addition to any benefit and other administrative penalties that otherwise arise under the Employee Retirement Income Security Act and/or the Social Security Act for violating these mandates, employers sponsoring plans that violate any of 40 listed mandates imposed by Obamacare or certain other federal laws also become liable under Internal Revenue Code Section 6039D to self-identify, self-assess, report on Form 8928 and pay an excise tax equal to $100 per person per uncorrected violation. The IRS, Department Of Labor and Department Of Health and Human Services have taken the position the January 20 Executive Order also does not bar enforcement of those Obamacare penalties. Accordingly, employers and their group health plans continue to face potentially substantial liability if their group health plan does not comply with Obamacare.
In the face of these exposures, employers and their group health plan administrators, fiduciaries and advisors should carefully review their plans and their administration for compliance before the end of the plan year so as to be able to take appropriate and timely corrective action before penalties attach and while stop loss or other insurance is available to help mitigate the cost of these corrections. Employers preparing for upcoming health plan renewals also should review their group contracts and conduct due diligence to verify their group health plan terms and operations meet the mandates as they initiate new plan years. Employers also generally will want to review their compliance and take action to address any deficiencies against any vendors or advisers who may have culpability in the defective health plan design or administration. Prompt action against vendors who may be culpable for the design or administration defects is necessary to preserve potential claims for contractual, deceptive trade practices or other causes of action that an employer might have under state contract, tort or other law. Employers and health plan fiduciaries should consider engaging experienced legal counsel to conduct this review on behalf of the employer other plan sponsor within the scope of attorney-client privilege so as to assess and address these potential risks on a timely basis and explore options within the scope of privilege. Brokers, advisors, consultants and insurers whose employer clients also may want to assess compliance risks and/or urge their clients to do so to help minimize their exposure to malfeasance or other claims from clients angry about penalties and other unexpected costs of noncompliance.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
Well-known for her extensive work with health, insurance, financial services, technology, energy, manufacturing, retail, hospitality, governmental and other highly regulated employers, her nearly 30 years’ of experience encompasses domestic and international businesses of all types and sizes.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediatepast RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, BenefitsMagazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com such as the following:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2017 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on IRS Prepares To Nail Employers Under Obamacare Mandate While Giving Some Individual Mandate Relief |
Comments Off on IRS Prepares To Nail Employers Under Obamacare Mandate While Giving Some Individual Mandate Relief |  105(h), 5000, ACA, compliance, Employee Benefits, Employer, Employers, Employment, Employment Policies, Employment Tax, ERISA, Excise Taxes, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, health plan, Health Plans, health reform, Human Resources, Premium Subsidies, Uncategorized |
105(h), 5000, ACA, compliance, Employee Benefits, Employer, Employers, Employment, Employment Policies, Employment Tax, ERISA, Excise Taxes, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, health plan, Health Plans, health reform, Human Resources, Premium Subsidies, Uncategorized |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
October 14, 2017
Monthly Social Security and Supplemental Security Income (SSI) benefits for more than 66 million Americans will increase 2.0 percent in 2018.
The Social Security Administration announced the 2.0 cost of living adjustment (COLA) Friday announced a 2% increase in benefits for 2018.
The largest COLA increase since 2012 will increase the benefits payable to more than 61 million Social Security beneficiaries in January 2018. Increased payments to more than 8 million SSI beneficiaries will begin on December 29, 2017. The Social Security Administration deducts $1 from benefits for each $3 earned over $45,360 until the month the worker turns age 66.)
There is no limit on earnings for workers who are “full” retirement age or older for the entire year.
The slight increase in benefits also may result in a corresponding decrease in disability benefits under plans that integrate or otherwise offset plan benefits with Social Security.
Information about Medicare COLAs for 2018, when announced, will be available at www.Medicare.gov.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
Well-known for her extensive work with health, insurance, financial services, technology, energy, manufacturing, retail, hospitality, governmental and other highly regulated employers, her nearly 30 years’ of experience encompasses domestic and international businesses of all types and sizes.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com such as the following:
▪ RAISE Act Immigration Reforms Touted As “Giving Americans A Raise”
▪ Health Clinic At Houston Convention Center, Other HHS Help For Hurricane Harvey Victims
▪ IRS Updates Amounts Used To Calculate 2017 Obamacare Individual Individual Shares Responsibility Tax Penalties
▪ DB Plan Sponsors Check Out New Bifurcated Distribution Model Amendmentsy
▪ U.S. News Names 2017-2018 “Best” Hospitals; Patient Usefulness Starts With Metholodogy Understanding
▪ Use Lessons Of Past Mistakes or Injustice To Build Better Future
▪ Prepare For Turnover, Other Challenges From Rising Workforce Competition
▪ Employers, Health Plans Should Brace For Tightened Federal Mental Health Coverage Mandate Disclosure And Enforcement
▪ Withholding Calculator Tool Helps Workers Figure Withholding
▪ Better Preparing U.S. Workers To Fill Your Jobs
▪ SCOTUS Ruling Bars Many State Arbitration Agreement Restrictions
▪ $2.4M HIPAA Settlement Message Warns Health Plans & Providers Against Sharing Medical Info With Media, Others
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2017 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on 2018 Social Security COLAs Set |
Comments Off on 2018 Social Security COLAs Set |  Claims Administration, defined benefit plan, Defined Benefit Plans, Disability, Disability Plans, Employee Benefits, Employer, Employers, Employment, ERISA, HR, Human Resources, pension plan, retirement plan, Retirement Plans, Retirements, Social Security, Uncategorized | Tagged: Social Security, SSI |
Claims Administration, defined benefit plan, Defined Benefit Plans, Disability, Disability Plans, Employee Benefits, Employer, Employers, Employment, ERISA, HR, Human Resources, pension plan, retirement plan, Retirement Plans, Retirements, Social Security, Uncategorized | Tagged: Social Security, SSI |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
October 13, 2017
Qualified profit-sharing and pension plan sponsors, fiduciaries, administrators and service providers should check of this recent guidance on various qualified pension and profit sharing plan qualification:
Organizations and service providers involved in defined benefit plans should review their programs and make adjustments as warranted.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
Well-known for her extensive work with health, insurance, financial services, technology, energy, manufacturing, retail, hospitality, governmental and other highly regulated employers, her nearly 30 years’ of experience encompasses domestic and international businesses of all types and sizes.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment;a member and policy technical adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, Insurance Thought Leaders, and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com.
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here including:
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and uhave no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2017 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on IRS Updates Defined Benefit Plan Guidance |
Comments Off on IRS Updates Defined Benefit Plan Guidance |  Bankruptcy, board of directors, Brokers, Corporate Compliance, corporate governance, defined benefit plan, Defined Benefit Plans, directors, employee, Employee Benefits, Employer, Employers, Employment Policies, Employment Tax, ERISA, Excise Tax, Form 5500, Government Contractors, government plan, HR, Human Resources, Insurance, Internal Revenue Code, IRC, Labor Management Relations, Management, retirement plan, Retirement Plans, Retirements, Tax, Tax Qualification, Uncategorized, Worker Classification | Tagged: defined benefit plan, Retirement Plans, tax qualification |
Bankruptcy, board of directors, Brokers, Corporate Compliance, corporate governance, defined benefit plan, Defined Benefit Plans, directors, employee, Employee Benefits, Employer, Employers, Employment Policies, Employment Tax, ERISA, Excise Tax, Form 5500, Government Contractors, government plan, HR, Human Resources, Insurance, Internal Revenue Code, IRC, Labor Management Relations, Management, retirement plan, Retirement Plans, Retirements, Tax, Tax Qualification, Uncategorized, Worker Classification | Tagged: defined benefit plan, Retirement Plans, tax qualification |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
October 12, 2017
President Trump today (October 12, 2017) issued the following that he promised to be the first in a series of executive orders and other administrative actions that his administration will roll out to provide Obamacare relief for consumers, employers and others by promoting healthcare choice and competition given the continued difficulty by the Republican-led Congress to pass legislation repealing or replacing the health care law.
What actually will result remains to be seen. Like the January 20, 2017 Executive Order Minimizing the Economic Burden of the Patient Protection and Affordable Care Act Pending Repeal that President Trump signed as his first executive order, the new Executive Order doesn’t actually change anything; it merely directs the agencies to review and propose for implementation changes to regulations and other guidance allowed by law.
On the heels of his announcement of the Executive Order, President Trump moved forward on his promise to take other action on Obamacare by announcing that the Administration will not continue funding for individual subsidies that currently are continued under an Obama Administration action in the absence of Congressional action funding those subsidies.
Concerned parties should monitor and inform themselves about proposed changes in the Executive Order and other actions as they are proposed and develop, and provide timely comments and other input to help influence the shape and content of any changes proposed or adopted in response to the Executive Order. Solutions Law Press, Inc. will be monitoring developments. Stay tuned for updates.
Language of Executive Order
By the authority vested in me as President by the Constitution and the laws of the United States of America, it is hereby ordered as follows:
Section 1. Policy.
(a) It shall be the policy of the executive branch, to the extent consistent with law, to facilitate the purchase of insurance across State lines and the development and operation of a healthcare system that provides high-quality care at affordable prices for the American people. The Patient Protection and Affordable Care Act (PPACA), however, has severely limited the choice of healthcare options available to many Americans and has produced large premium increases in many State individual markets for health insurance. The average exchange premium in the 39 States that are using http://www.healthcare.gov in 2017 is more than double the average overall individual market premium recorded in 2013. The PPACA has also largely failed to provide meaningful choice or competition between insurers, resulting in one-third of America’s counties having only one insurer offering coverage on their applicable government-run exchange in 2017.
(b) Among the myriad areas where current regulations limit choice and competition, my Administration will prioritize three areas for improvement in the near term: association health plans (AHPs), short-term, limited-duration insurance (STLDI), and health reimbursement arrangements (HRAs).
(i) Large employers often are able to obtain better terms on health insurance for their employees than small employers because of their larger pools of insurable individuals across which they can spread risk and administrative costs. Expanding access to AHPs can help small businesses overcome this competitive disadvantage by allowing them to group together to self-insure or purchase large group health insurance. Expanding access to AHPs will also allow more small businesses to avoid many of the PPACA’s costly requirements. Expanding access to AHPs would provide more affordable health insurance options to many Americans, including hourly wage earners, farmers, and the employees of small businesses and entrepreneurs that fuel economic growth.
(ii) STLDI is exempt from the onerous and expensive insurance mandates and regulations included in title I of the PPACA. This can make it an appealing and affordable alternative to government-run exchanges for many people without coverage available to them through their workplaces. The previous administration took steps to restrict access to this market by reducing the allowable coverage period from less than 12 months to less than 3 months and by preventing any extensions selected by the policyholder beyond 3 months of total coverage.
(iii) HRAs are tax-advantaged, account-based arrangements that employers can establish for employees to give employees more flexibility and choices regarding their healthcare. Expanding the flexibility and use of HRAs would provide many Americans, including employees who work at small businesses, with more options for financing their healthcare.
(c) My Administration will also continue to focus on promoting competition in healthcare markets and limiting excessive consolidation throughout the healthcare system. To the extent consistent with law, government rules and guidelines affecting the United States healthcare system should:
(i) expand the availability of and access to alternatives to expensive, mandate-laden PPACA insurance, including AHPs, STLDI, and HRAs;
(ii) re-inject competition into healthcare markets by lowering barriers to entry, limiting excessive consolidation, and preventing abuses of market power; and
(iii) improve access to and the quality of information that Americans need to make informed healthcare decisions, including data about healthcare prices and outcomes, while minimizing reporting burdens on affected plans, providers, or payers.
Sec. 2. Expanded Access to Association Health Plans.
Within 60 days of the date of this order, the Secretary of Labor shall consider proposing regulations or revising guidance, consistent with law, to expand access to health coverage by allowing more employers to form AHPs. To the extent permitted by law and supported by sound policy, the Secretary should consider expanding the conditions that satisfy the commonality‑of-interest requirements under current Department of Labor advisory opinions interpreting the definition of an “employer” under section 3(5) of the Employee Retirement Income Security Act of 1974. The Secretary of Labor should also consider ways to promote AHP formation on the basis of common geography or industry.
Sec. 3. Expanded Availability of Short-Term, Limited‑Duration Insurance.
Within 60 days of the date of this order, the Secretaries of the Treasury, Labor, and Health and Human Services shall consider proposing regulations or revising guidance, consistent with law, to expand the availability of STLDI. To the extent permitted by law and supported by sound policy, the Secretaries should consider allowing such insurance to cover longer periods and be renewed by the consumer.
Sec. 4. Expanded Availability and Permitted Use of Health Reimbursement Arrangements.
Within 120 days of the date of this order, the Secretaries of the Treasury, Labor, and Health and Human Services shall consider proposing regulations or revising guidance, to the extent permitted by law and supported by sound policy, to increase the usability of HRAs, to expand employers’ ability to offer HRAs to their employees, and to allow HRAs to be used in conjunction with nongroup coverage.
Sec. 5. Public Comment.
The Secretaries shall consider and evaluate public comments on any regulations proposed under sections 2 through 4 of this order.
Within 180 days of the date of this order, and every 2 years thereafter, the Secretary of Health and Human Services, in consultation with the Secretaries of the Treasury and Labor and the Federal Trade Commission, shall provide a report to the President that:
(a) details the extent to which existing State and Federal laws, regulations, guidance, requirements, and policies fail to conform to the policies set forth in section 1 of this order; and
(b) identifies actions that States or the Federal Government could take in furtherance of the policies set forth in section 1 of this order.
Sec. 7. General Provisions.
(a) Nothing in this order shall be construed to impair or otherwise affect:
(i) the authority granted by law to an executive department or agency, or the head thereof; or
(ii) the functions of the Director of the Office of Management and Budget relating to budgetary, administrative, or legislative proposals.
(b) This order shall be implemented consistent with applicable law and subject to the availability of appropriations.
(c) This order is not intended to, and does not, create any right or benefit, substantive or procedural, enforceable at law or in equity by any party against the United States, its departments, agencies, or entities, its officers, employees, or agents, or any other person.
DONALD J. TRUMP
THE WHITE HOUSE,
October 12, 2017
Implications & Actions
The impact of this and other Executive Orders and other Presidential actions depend upon what actions, if any, the agencies determine they are allowed by law to take and how those changes are implemented. Concerned persons and organizations should begin preparing input to the agencies and monitoring and commenting on proposals and other guidance to help shape the outcome.
Solutions Law Press, Inc. is preparing initial analysis of this Executive Order and will be closely monitoring and updating this analysis. Follow up to learn more and stay abreast of new developments.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
Well-known for her extensive work with health, insurance, financial services, technology, energy, manufacturing, retail, hospitality, governmental and other highly regulated employers, her nearly 30 years’ of experience encompasses domestic and international businesses of all types and sizes. Author of numerous works on privacy and data security, Ms. Stamer‘s experience includes involvement in cyber security and other data privacy and security matters for more than 20 years.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com such as the following:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2017 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on Read Trump Health Care Executive Order |
Comments Off on Read Trump Health Care Executive Order |  105(h), ACA, Affordable Care Act, Association Health Plan, Brokers, Civil Rights, Claims Administration, Corporate Compliance, EBSA, employee, Employee Benefits, Employer, Employers, ERISA, Excise Tax, Excise Taxes, Fiduciary Responsibility, FLSA, Form 5500, health benefit, Health Benefits, health Care, Health Care Reform, health insurance, health insurance marketplace, health plan, Health Plans, health reform, HR, Human Resources, Insurance, insurers, Internal Controls, Internal Revenue Code, IRC, MEWA, Payroll Tax, Premium Subsidies, Reporting & Disclosure, Tax Credit, Uncategorized, Union, Wellness, Wellness Programs, Worker Classification, Workforce, zane benefits | Tagged: ACA, Affordable Care Act, Corporate Compliance, Employee Benefits, Employer, Employers, Employment, employment law, ERISA, executive, Health Care, Health Care Reform, Health Insurance, Health Plan, Health Plans, Human Resources, Insurance, Labor, Labor Department, Managed Care, Medical Coverage, Overtime, Tax, wage and hour, Worker Classification |
105(h), ACA, Affordable Care Act, Association Health Plan, Brokers, Civil Rights, Claims Administration, Corporate Compliance, EBSA, employee, Employee Benefits, Employer, Employers, ERISA, Excise Tax, Excise Taxes, Fiduciary Responsibility, FLSA, Form 5500, health benefit, Health Benefits, health Care, Health Care Reform, health insurance, health insurance marketplace, health plan, Health Plans, health reform, HR, Human Resources, Insurance, insurers, Internal Controls, Internal Revenue Code, IRC, MEWA, Payroll Tax, Premium Subsidies, Reporting & Disclosure, Tax Credit, Uncategorized, Union, Wellness, Wellness Programs, Worker Classification, Workforce, zane benefits | Tagged: ACA, Affordable Care Act, Corporate Compliance, Employee Benefits, Employer, Employers, Employment, employment law, ERISA, executive, Health Care, Health Care Reform, Health Insurance, Health Plan, Health Plans, Human Resources, Insurance, Labor, Labor Department, Managed Care, Medical Coverage, Overtime, Tax, wage and hour, Worker Classification |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
October 6, 2017
As businesses continue to struggle to comply with the growing plethora of federal and state laws mandating data security, the identity theft and cyber security epidemic keeps growing.
As human resources and other business leaders work to guard their own data and respond to employee demands for assistance in responding to breaches of their personal financial and other data, this weeks’ announcement that embattled credit monitoring giant Equifax has been awarded the exclusive contract to provide taxpayer identification and fraud prevention services to the Internal Revenue Service has many questioning whether these investments are futile.
The IRS’ announcement comes despite the September 7, 2017 announcement by Equifax of a data breach of its records impacting sensitive personal information of millions of consumers including:
- The names, Social Security numbers, birth dates, addresses and, in some instances, driver’s license numbers of an estimated 143 million U.S. consumers;
- Credit card numbers for approximately 209,000 U.S. consumers,
- Certain dispute documents with personal identifying information for approximately 182,000 U.S. consumers,and
- Personal information for certain U.K. and Canadian consumers.
The huge breach already was creating many headaches for many businesses and their human resources departments before the IRS announced the award of the contract to Equifax. Due to the massive size of the breach, mist companies have been required to respond to concerns of workers impacted directly by the breach as well as requests of employees and identity theft protection companies that the business consider offering cybersecurity protection for employees or customers.
Beyond helping their workforce understand and cope with the news, many businesses and employee benefit plans also face the added headache of needing to investigate and respond to concerns about their own potential responsibilities to provide breach notification or take other actions. This added headache arises due to their or their plans’ use of Equifax or vendors utilizing Equifax to run employee or vendor background checks or carry out internal employee or employee benefit plan, customer or other business activities. These involvements often give rise to duties to conduct investigations and potentially provide notification or other responses to employees, applicants, benefit plan members, contractors or customers whose data may have been impacted under the Fair and Accurate Credit Transactions Act (FACTA), the Health Insurance Portability and Accountability Act (HIPAA), the Employee Retirement Income Security Act (ERISA) Fiduciary Responsibility rules or various other federal and state laws and regulations, vendor contracts or their own data privacy or security policies.
When notification is recommended or required, human resources and other business leaders also have to consider if modifications should be considered to standard protocols recommended to data breach victims. Notification and registration as an identity theft victim with Equifax long has been a standard part of the federal and state government recommended protocol for recommended to consumers impacted by identity theft or other data breaches. See,e.g., IRS Taxpayer Guide To Identity Theft. Although government agencies as of yet have not changed this recommendation to remove Equifax reporting, many consumers and others view reporting to Equifax as akin to the fox watching the hen house. Consequently, employers and other parties helping consumers respond to the breach often receive push back or questions from consumers about the appropriateness and security reporting to Equifax in light of its breach.
Beyond evaluating and handling their own legal responsibilities to investigate and deal with any breach impacting their data, employers and other business leaders also likely are or should consider what claims against Equifax, other vendors and business partners involved with Equifax and their own liability insurers are available and warranted to help cover the costs and potential liabilities for the business arising from the breach and it’s fall out.
As employers and other businesses work through these issues, They should keep in mind that the fallout is likely to continue for years and be further complicated by past and subsequent breaches impacting other governmental and private organizations. Human resources, employee benefits and other businesses and their leaders can expect to experience challenges dealing with fraudulent uses of misappropriated information as well as demands that they tighten up their background check, data security and usage and other practices and documentation to mitigate risks from the compromised data.
Human resources, employee benefits and other business leaders need to secure the assistance of counsel experienced in guiding their organizations through these and other challenges.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
Well-known for her extensive work with health, insurance, financial services, technology, energy, manufacturing, retail, hospitality, governmental and other highly regulated employers, her nearly 30 years’ of experience encompasses domestic and international businesses of all types and sizes. Author of numerous works on privacy and data security, Ms. Stamer‘s experience includes involvement in cyber security and other data privacy and security matters for more than 20 years.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com such as the following:
▪RAISE Act Immigration Reforms Touted As “Giving Americans A Raise”
▪Health Clinic At Houston Convention Center, Other HHS Help For Hurricane Harvey Victims
▪IRS Updates Amounts Used To Calculate 2017 Obamacare Individual Individual Shares Responsibility Tax Penalties
▪DB Plan Sponsors Check Out New Bifurcated Distribution Model Amendmentsy
▪U.S. News Names 2017-2018 “Best” Hospitals; Patient Usefulness Starts With Metholodogy Understanding
▪Use Lessons Of Past Mistakes or Injustice To Build Better Future
▪Prepare For Turnover, Other Challenges From Rising Workforce Competition
▪Employers, Health Plans Should Brace For Tightened Federal Mental Health Coverage Mandate Disclosure And Enforcement
▪Withholding Calculator Tool Helps Workers Figure Withholding
▪Better Preparing U.S. Workers To Fill Your Jobs
▪SCOTUS Ruling Bars Many State Arbitration Agreement Restrictions
▪$2.4M HIPAA Settlement Message Warns Health Plans & Providers Against Sharing Medical Info With Media, Others
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2017 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on Dealing With HR, Benefits & Other Headaches From Equifax and Other Data Breach |
Comments Off on Dealing With HR, Benefits & Other Headaches From Equifax and Other Data Breach |  Banking, board of directors, Brokers, Civil Monetary Penalties, Claims, Claims Administration, compliance, conflict of interest, Consumer Protection, Corporate Compliance, corporate governance, Cybercrime, Data Breach, Data Security, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, directors, E-Verify, EBSA, Educational Privacy, employee, Employee Benefits, Employer, Employers, Employment, Employment Policies, Employment Tax, ERISA, ESOP, Excise Tax, FACTA, Fair Credit Reporting Act, FICA, fiduciary duty, Fiduciary Responsibility, Financial Security, Form 5500, GINA, Government Contractors, health benefit, Health Benefits, health Care, health insurance, health plan, Health Plans, HIPAA, Hiring, HR, Human Resources, I-9, Identity Theft, Income Tax, Insurance, insurers, Internal Controls, Internal Investigations, Internal Revenue Code, Internet, IRC, Labor Management Relations, Leadership, Management, Managment, Patient Empowerment, Payroll Tax, pension plan, Physician, Plan Admistrator, Privacy, Professional Liability, Protected Health Information, Provider, Reporting & Disclosure, retirement plan, Retirement Plans, Retirements, Risk Management, Security, Tax, Tax Credit, Tax Qualification, Technology, third party administrators, visas, Workforce | Tagged: ADA, Corporate Compliance, Data Breach, Employee Benefits, Employer, Employers, employment law, Equifax, ERISA, Health Care, Health Insurance, HIPAA, Human Resources, Insurance, Insurer, Labor Department, Privacy, Retirement Plans, Risk Management, Tax, Technology, wage and hour, Worker Classification |
Banking, board of directors, Brokers, Civil Monetary Penalties, Claims, Claims Administration, compliance, conflict of interest, Consumer Protection, Corporate Compliance, corporate governance, Cybercrime, Data Breach, Data Security, defined benefit plan, Defined Benefit Plans, defined contribution plan, Defined Contribution Plans, directors, E-Verify, EBSA, Educational Privacy, employee, Employee Benefits, Employer, Employers, Employment, Employment Policies, Employment Tax, ERISA, ESOP, Excise Tax, FACTA, Fair Credit Reporting Act, FICA, fiduciary duty, Fiduciary Responsibility, Financial Security, Form 5500, GINA, Government Contractors, health benefit, Health Benefits, health Care, health insurance, health plan, Health Plans, HIPAA, Hiring, HR, Human Resources, I-9, Identity Theft, Income Tax, Insurance, insurers, Internal Controls, Internal Investigations, Internal Revenue Code, Internet, IRC, Labor Management Relations, Leadership, Management, Managment, Patient Empowerment, Payroll Tax, pension plan, Physician, Plan Admistrator, Privacy, Professional Liability, Protected Health Information, Provider, Reporting & Disclosure, retirement plan, Retirement Plans, Retirements, Risk Management, Security, Tax, Tax Credit, Tax Qualification, Technology, third party administrators, visas, Workforce | Tagged: ADA, Corporate Compliance, Data Breach, Employee Benefits, Employer, Employers, employment law, Equifax, ERISA, Health Care, Health Insurance, HIPAA, Human Resources, Insurance, Insurer, Labor Department, Privacy, Retirement Plans, Risk Management, Tax, Technology, wage and hour, Worker Classification |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
August 21, 2017
Individual Americans that don’t maintain their and their dependents’ enrollment in at least minimum essential coverage in a health program meeting the requirements of the Patient Protection & Affordable Care Act commonly referred to as “Obama Care” still generally should expect to pay individual shared responsibility tax penalties imposed by Obamacare.
Despite campaign promises to quickly repeal or reform Obamacare, the Republican controlled Congress has been unable to pass legislation repealing the individual tax penalty or other Obamacare coverage mandate related rules. Moreover, contrary to the impression widely held by many Americans that President Trump’s January 20 Executive Order protects uncovered individuals from the tax imposed under Internal Revenue Code Section 5001A, the Internal Revenue Service still plans to enforce and collect the tax. See here. Consequently, Internal Revenue Code Section 5001A still generally requires uncovered taxpayers to pay the individual shared responsibility payment.
This means that taxpayers not enrolled in minimum essential coverage or otherwise exempt from the individual responsibility payment need to be prepared to pay the tax.
In anticipation of enforcement of the individual shared responsibility tax, the Internal Revenue Service just set the monthly national average premium for qualified health plans that have a bronze level of coverage offered through Exchanges at $272 per individual and the maximum monthly national average premium for qualified health plans with a bronze level of coverage offered through Exchanges at $1,360 for a shared responsibility family with five or more members. The Internal Revenue Service intends that these amounts will be used to calculate individual shared responsibility tax penalties for 2017. The updated amounts are published in Rev. Proc. 2017-48
In general, the individual responsibility tax equals the lesser of (1) the sum of the monthly penalty amounts, or (2) the sum of the monthly national average bronze plan premiums for the shared responsibility family. See § 1.5000A-4(a). The monthly national average bronze plan premium means, for a month for which a shared responsibility payment is imposed, 1/12 of the annual national average premium for qualified health plans that (1) have a bronze level of coverage, (2) would provide coverage for the taxpayer’s shared responsibility family members, and (3) are offered through Exchanges for plan years beginning in a calendar year with or within which the taxable year ends. §§ 5000A(c)(1)(B) and 1.5000A-4(c). For this purpose, “shared responsibility family” means, for a month in a taxable year, all nonexempt individuals for whom the taxpayer and the taxpayer’s spouse, if the taxpayer is married and files a joint return with the spouse, are liable for the shared responsibility payment under § 5000A for that taxable year. See § 1.5000A-1(d)(17).
Taxpayers who are not enrolled in the necessary health coverage to meet the Obamacare health coverage mandate should evaluate their shared responsibility tax penalty exposure and weigh whether it makes more sense to enroll in qualifying health coverage or prepare to pay the tax.
About The Author
Recognized as “Legal Leader™ Texas Top Rated Lawyer” in both Health Care Law and Labor and Employment Law, a “Texas Top Lawyer,” and an “AV-Preeminent” and “Top Rated Lawyer” by Martindale-Hubble, singled out as among the “Best Lawyers In Dallas” in employee benefits by D Magazine; Cynthia Marcotte Stamer is a practicing attorney and management consultant, author, public policy advocate and lecturer widely recognized for her nearly 30 years’ of work and pragmatic thought leadership, publications and training on health coverage and health care, health plan and employee benefits, workforce and related regulatory and other compliance, performance management, risk management, product and process development, public policy, operations and other concerns.
Throughout her legal and consulting career, Ms. Stamer has drawn recognition for combining extensive knowledge and experience with her talents as an insightful innovator and problem solver when advising, representing and defending employer and other plan sponsors, insurers, fiduciaries, insurers, electronic and other technology, plan administrators and other service providers, governments and others about health coverage, benefit program design, funding, documentation, administration, data security and use, contracting, plan, public and regulatory reforms and enforcement, and other risk management and operations matters as well as for her work and thought leadership on a broad range of other health, employee benefits, human resources and other workforce, insurance, tax, compliance and other matters. Her experience encompasses leading and supporting the development and defense of innovative new programs, practices and solutions; advising and representing clients on routine plan establishment, plan documentation and contract drafting and review, administration, change and other compliance and operations crisis prevention and response, compliance and risk management audits and investigations, enforcement actions and other dealings with the US Congress, Departments of Labor, Treasury, Health & Human Services, Federal Trade Commission, Justice, state legislatures, attorneys general, insurance, labor, worker’s compensation, and other agencies and regulators, She also provides strategic and other supports clients in defending litigation as lead strategy counsel, special counsel and as an expert witness.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares shared her thought leadership, experience and advocacy on these and other concerns by her service in the leadership of a broad range of other professional and civic organization including her involvement as Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE; Coalition on Patient Empowerment, a founding Board Member and past President of the Alliance for Healthcare Excellence, past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee, current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Section, Past Group Chair, current Defined Contribution Plan Committee Co-Chair, former Welfare Committee Chair and Co-Chair of the ABA RPTE Section Employee Benefits Group, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative and current RPTE Representative to the ABA Health Law Coordinating Counsel, former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, former member of the Board of Directors of the Southwest Benefits Association and others.
Ms. Stamer also is a highly popular lecturer, symposia chair and author, who publishes and speaks extensively on health and managed care industry, human resources, employment and other privacy, data security and other technology, regulatory and operational risk management for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, the Society of Professional Benefits Administrators, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients, serves on the faculty and planning committee of many workshops, seminars, and symposia, and on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications. For additional information about Ms. Stamer, see CynthiaStamer.com or contact Ms. Stamer via email to here or via telephone to (469) 767-8872.
About Solutions Law Press
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at www.SolutionsLawPress.com.
If you or someone else you know would like to receive future updates and notices about other upcoming Solutions Law Press™ events, please be sure that we have your current contact information – including your preferred e-mail by creating or updating your profile here. For important information concerning this communication, see here.
NOTICE: Any party accessing or using any content obtained from or through Solutions Law Press, Inc.™ acknowledges and agrees that any and all programs, publications, statements and materials presented or published by Solutions Law Press, Inc.™ and any statements or other contents made or contained therein are for general informational and educational purposes only. They are generic in nature and not tailored or intended to be relied upon by any person, business, entity or other party for purposes for determining the legal, financial or other appropriateness, defensibility, suitability, outcome or consequences of any strategy, action, course of action, or any other facts, circumstances, event or conduct. Users of these resources are responsible at all times for independently evluating the suitability of any content, materials, tools or other materials or information accessed from or through Solutions Law Press, Inc. directly or indirectly.
Solutions Law Press, Inc.™ and its authors and contributors do not represent or warrant in any form or manner, and expressly disclaim and deny the appropriateness of the use or reliance of any person or entity on any content, tools or resources accessed or obtained from or through Solutions Law Press, Inc.™ for any general or particular use or purpose by any party under any circumstances.
Likewise, they do not establish an attorney-client relationship or other fiduciary, contractual or other relationship between Solutions Law Press, Inc. and/or any of its authors or contributors and any other party. They are not, and do not serve as a substitute for legal, accounting, tax or other advice. They don’t create or otherwise give rise to any duty, obligation, responsibility on behalf of Solutions Law Press, Inc™ or any provider or offeree of content, tools or services to any party.
Parties accessing or using any of Solutions Law Press, Inc.™ competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The publisher and the author expressly disclaim all liability for this content and any responsibility to provide any update or otherwise notify anyone of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
©2017 Cynthia Marcotte Stamer. Non-Exclusive License To Republish Granted To Solutions Law Press.
 Comments Off on IRS Updates Amounts Used To Calculate 2017 Obamacare Individual Individual Shares Responsibility Tax Penalties |
Comments Off on IRS Updates Amounts Used To Calculate 2017 Obamacare Individual Individual Shares Responsibility Tax Penalties |  4980D, 4980H, 6039D, ACA, Affordable Care Act, Employee Benefits, Employer, Employers, Excise Tax, health benefit, Health Benefits, health Care, Health Care Reform, health insurance, health insurance marketplace, health plan, Health Plans, health reform, HR, Human Resources, Insurance, insurers, Internal Revenue Code, IRC, Patient Protection & Affordable Care Act, Premium Subsidies, Tax, Uncategorized | Tagged: ACA, Health Insurance, Health Plans, individual shared responsibility tax, Obamacare |
4980D, 4980H, 6039D, ACA, Affordable Care Act, Employee Benefits, Employer, Employers, Excise Tax, health benefit, Health Benefits, health Care, Health Care Reform, health insurance, health insurance marketplace, health plan, Health Plans, health reform, HR, Human Resources, Insurance, insurers, Internal Revenue Code, IRC, Patient Protection & Affordable Care Act, Premium Subsidies, Tax, Uncategorized | Tagged: ACA, Health Insurance, Health Plans, individual shared responsibility tax, Obamacare |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
August 8, 2017
U.S. employers recruiting or employing workers with high demand skills or experience in the U.S. labor market should reevaluate existing employee retention and recruiting packages and policies and intellectual property safeguards to deal with the increasingly competitive job market reflected in June, 2017 employment data and trends reflected in U.S. Bureau of Labor Statistics (BLS) data released today (August 8, 2017). Employers relying on workers within these industries should re-evaluate and update as necessary their existing budgeting, hiring, recruitment and retention, trade secret, noncompetition and other policies and practices to proactively position their companies to effectively compete to ensure they retain and recruit the necessary workers to operate effectively.
The BLS statistics offer employers and others key insights into various workforce and employment trend, not the least of which are signs of growing competition among employers for high demand workers arising from the continued growth in job openings reported in the BLS statistics. See, e.g. Table A. Job openings, hires, and total separations by industry, seasonally adjusted and Job Openings and Labor Turnover Technical Note; Table 1. Job openings levels and rates by industry and region, seasonally adjusted; Table 2. Hires levels and rates by industry and region, seasonally adjusted; Table 3. Total separations levels and rates by industry and region, seasonally adjusted.
BLS statistics showing new hires lagging behind the continued growth in job openings signal that employers in impacted industries and regions should prepare to face growing competition for qualified workers.
According to BLS, the U.S. job openings level increased by 461,000 to 6.2 million openings as of the last day of June. Among these 461,000 new openings, the overwhelming majority – 417,000 openings were for private sector positions, with the largest increases occurring in professional and business services (+179,000), health care and social assistance (+125,000) and construction (+62,000) while job openings decreased for other services by 62,000.
Meanwhile, BLS statistics showing that hires and total separations did not keep up with the growth in job openings sends a strong message that employers employing workers from increasingly competitive talent pools should focus as much on their ability to retain existing workers as to recruit new workers to fill new positions or replace workers. Aside from the gap between job openings and hires generally, quit rate statistics reported by BLS merit special consideration. As quits are voluntary separations initiated by the employee, the quit rate can serve as a measure of workers’ willingness or ability to leave an existing position for a new opportunity. BLS statistics showing continued stability in the quit rate and number of quits during June suggests that as of the end of June, reflected that many employed workers in high growth industries had not yet decided to make the leap to a new position. See Table 4. Quits levels and rates by industry and region, seasonally adjusted. Table 10. Quits levels and rates by industry and region, not seasonally adjusted.
Amid growing competition for workers, however, it is foreseeable that employers seeking to fill open positions will turn their attention to employers already employed. Accordingly, in addition to evaluating their ability to recruit qualified workers away from other employers, employers should anticipate and prepare for the likelihood that other employers increasingly will target their workers for recruitment.
Adequate analysis and preparation now could help position their businesses both to retain valuable workers and recruit new or replacement workers to fulfill their staffing leads. Beyond considering the adequacy of current recruitment, compensation, benefits, work rules and culture to compete effectively amid the evolving labor market, business leaders also generally will want to evaluate the adequacy and enforceability of trade secret, noncompetition and solicitation, and other legal and operational controls to protect their organization’s workforce and intellectual property from turnover related threats and dilution both as they relate to new hires and potential departing employees.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
Well-known for her extensive work with health, insurance, financial services, technology, energy, manufacturing, retail, hospitality, governmental and other highly regulated employers, her nearly 30 years’ of experience encompasses domestic and international businesses of all types and sizes.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com such as the following:
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2017 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on Prepare For Turnover, Other Challenges From Rising Workforce Competition |
Comments Off on Prepare For Turnover, Other Challenges From Rising Workforce Competition |  401(k), directors, employee, Employee Benefits, Employer, Employers, Employment, Employment Agreement, ERISA, Executive Compensation, health plan, Management, Managment, Non-Compete, Non-Competition Agreement, Uncategorized | Tagged: Economy, Employer, Hiring, HR, Job Growth, Labor, Labor Management Relations, Labor Pool, Labor Statistics, Management, Recruiting, Workforce |
401(k), directors, employee, Employee Benefits, Employer, Employers, Employment, Employment Agreement, ERISA, Executive Compensation, health plan, Management, Managment, Non-Compete, Non-Competition Agreement, Uncategorized | Tagged: Economy, Employer, Hiring, HR, Job Growth, Labor, Labor Management Relations, Labor Pool, Labor Statistics, Management, Recruiting, Workforce |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
August 2, 2017
Employers operating in the United States (U.S.) should evaluate potential workforce and implications of immigration law reforms proposed in the revised The Reforming American Immigration for a Strong Economy Act (RAISE Act) reintroduced in the Senate by co-sponsors Senators Tom Cotton and David Perdue with the announced backing of President Donald Trump earlier today (August 2, 2017).
Applauding the RAISE ACT as his preferred vehicle for implementing the “merit based” Green Card system he promised would be implemented during his Presidential campaign, President Trump said the RAISE Act reforms will “give Americans a raise” by creating a “skills-based immigration system that seeks to make America more competitive, raise wages for American workers, and create jobs” while also ensuring that “newcomers to our wonderful country will be assimilated, will succeed, and will achieve the American Dream.”
In pursuit of these goals, the RAISE Act would radically restructure U.S. rules to radically change the foreign workers and others eligible to qualify for work or other visas to enter the U.S., the procedures for their selection and other visa rules.
The centerpiece of these reforms are the RAISE Act’s proposal to replace the current permanent employment visa and lottery visa programs used to determine what foreign workers receive Green Cards to work in the U.S. with a “merit based system” under which a newly created “skills-based point system” would determine the workers eligible for selection to receive a work visa to work in the U.S. based upon listed “predictors of immigrant success and economic contribution.” Under the skills-based point system created by the RAISE Act, selection for inclusion in the pool of workers eligible to work in the U.S. would rank foreign workers seeking visas based on a merit-based point system created under the legislation.
Beyond these specific reforms to the worker visa programs, other proposed reforms that tighten the eligibility rules and requirements for granting visas to noncitizen family members of U.S. citizens and foreign workers also can be expected to impact the recruitment and employment of foreign workers. For this reason, employers and workers concerned with the recruitment of foreign labor to work in the United States generally will want to carefully evaluate all of these proposed reforms.
Proposed Direct Reforms To Work Visa Programs
The RAISE Act’s strategy for reforming the worker visa program focuses on the replacement of the current permanent employment visa and lottery programs with a newly created “skills-based points system” for granting work-eligible visas similar to systems used by Canada and Australia. Concurrent with the deployment of the new skills-based point system, the RAISE Act provides for the elimination of the existing diversity visa lottery program, pursuant to which the U.S. currently grants via lottery selection 50,000 visas annually in a lottery to applicants from countries with low rates of immigration to the United States, with no regard to the applicants’ skills.
As proposed under RAISE Act §5, the U.S. would issue up to 140,000 employment-based visas annually to applicants selected by the U.S. Citizenship and Immigration Services twice a year to receive an invitation to file full applications and undergo security vetting from the pool of applicants scoring the highest points the new skills-based points system created under the RAISE Act.
Under the RAISE Act reforms, a new skills-based points system would be used to prioritize applicants for visa eligibility based on the following “predictors of immigrant success and economic contribution:”
- Education,
- English-language ability,
- High-paying job offers,
- Age,
- Record of extraordinary achievement, and
- Entrepreneurial initiative.
The RAISE Act would require that an applicant score at least 30-points to eligible to qualify for inclusion in the pool of applicants eligible to be considered for possible selection to receive an employment-based visa or “Green Card.” Subject to this floor, applicants would be selected for invitation to complete the application process and undergo a security check based on their score relative to other applicants.
Immigrant households arriving through the points system are not eligible for federal means tested benefits for a period of 5 years.
Section 5(e) of the RAISE Act requires an annual statistical report on the skills-based points system while Section 5(f) requires a quadrennial report to Congress recommending updates to the points system with the aim of improving the economy and enhancing working Americans’ wages.
Section 6 conditions naturalization on the sponsors of an immigrant fulfilling their obligation to reimburse the federal government for benefits used by the immigrant, as required under current law.
Proposed Changes To Immigration Preferences for Family Members of U.S. Citizens & Residents
Beyond the direct reforms to the worker visa systems, the RAISE Act’s proposed changes to the preferences for granting visas to family members of U.S. citizens and residents also are likely to impact the recruitment and retention of foreign workers to fill positions in the United States by both narrowing to spouses and children the list of family members eligible to qualify as “family-sponsored immigrants” and tightening the requirements for parents of citizens and residents to qualify for visitors visa.
As proposed, the RAISE Act would keep, but narrow the availability of visas for “family-sponsored immigrants.” RAISE Act §4 would continue to allow preferences for spouses and minor children of U.S. residents but eliminate visa preferences for extended family and grown adult family members of U.S. residents. Along with narrowing the individuals that can qualify for visa preferences as family-sponsored immigrants, the RAISE Act also caps the allowable number of “family-sponsored immigrants” eligible for admission per fiscal year to 88,000 reduced by the number of certain previously admitted family-sponsored immigrants not obtaining alien lawfully admitted to the United States for permanent residence status within a specified period remaining in the United States.
Along with this narrowing of the applicability of preferences for family-sponsored immigrants, the RAISE Act also proposes to create a temporary visa under which elderly parents of U.S. residents could come to the United States for a limited period of time conditional upon the fulfillment by the resident of certain conditions. This newly created nonimmigrant classification for alien parents of adult United States Citizens would be conditional upon the sponsoring nonimmigrant child being at least 21 years old, legally resident in the U.S., responsible for the nonimmigrant parent’s support and for providing satisfactory proof that the sponsoring child maintains health insurance coverage for the parent at no cost to the parent. Furthermore, the parent receiving the visitor’s visa would not be authorized to be employed in the United States or eligible for any Federal, State, or local public benefit.
Proposed Cap on Offers Of Permanent Residency To Refugees
RAISE Act § 3 would caps the number of refugees granted permanent visas to the United States at 50,000 per year, in line with a 13-year average. It also requires the President to report the annual number of refugees admitted to the United States.
President, Sponsors Say Reforms Give U.S. Citizens “A Raise”
Joined by RAISE Act co-sponsors Senator Cotton and Senator Perdue for his Rose Garden announcement of support for enactment of the RAISE Act this morning, President Trump reaffirmed his campaign commitment to create “a merit-based immigration system that protects U.S. workers and taxpayers” that “demonstrates our compassion for struggling American families who deserve an immigration system that puts their needs first and that puts America first” while helping “ensure that newcomers to our wonderful country will be assimilated, will succeed, and will achieve the American Dream.
According to President Trump, “The RAISE Act — R-A-I-S-E — the RAISE Act will reduce poverty, increase wages, and save taxpayers billions and billions of dollars … by changing the way the United States issues Green Cards to nationals from other countries” to protect low skilled U.S. workers from unfair foreign immigrant competition by replacing a “low-skilled system” with a new points-based system for receiving a Green Card “that favors applicants who can speak English, financially support themselves and their families, and demonstrate skills that will contribute to our economy.”
President Trump also touted provisions of the RAISE Act for preventing new migrants and new immigrants from collecting welfare and other benefits upon entry to the country as protecting U.S. taxpayers.
Implications For Employers
The reforms proposed by the RAISE Act, if enacted as proposed are likely to impact U.S. based employers in a multitude of ways including, but not limited to the obvious changes in the selection and availability of foreign workers for employment in the United States.
Obviously, the proposed changes to the processes for selection and qualification of non-citizens will impact both the nature of the workers eligible for employment, and the procedures and timing of their availability. The emphasis on granting visas to higher skilled workers over those with lower skills likely will raise concerns for employers reliant upon lower skilled foreign labor. While the new point system is touted as preferring the recruitment of higher skilled workers, it remains to be seen whether the system actually will meet the workforce needs already expressed by a host of hi-tech and other U.S. businesses concerned about immigration reform. Meanwhile, employers recruiting foreign workers with family members also should anticipate that foreign workers may request or require assistance from their U.S. employer to fulfill newly imposed requirements that the worker provide health care coverage as a condition to his sponsorship of a parental visa or to address new government benefit eligibility exclusions included in the RAISE Act.
Beyond impacting the actual availability of foreign workers and their skill sets, it also is likely that the English-speaking and other preferences incorporated into the skills based point system proposed by the REACH Act also inevitably will necessitate some reconsideration if not actual reform of federal or state laws or regulations concerning nondiscrimination based on national origin, race or other civil rights laws that have been the basis of challenges to English language only workforce or other business rules. It remains to be seen how Congress and the Administration contemplates the new priority system will integrate with the employment and other federal and state laws that commonly are relied upon to protect foreign and English as a Second Language individuals against employment and other discrimination.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
Well-known for her extensive work with health, insurance, financial services, technology, energy, manufacturing, retail, hospitality, governmental and other highly regulated employers, her nearly 30 years’ of experience encompasses domestic and international businesses of all types and sizes. A former lead consultant to the Government of Bolivia on its Pension Reform project, Vice Chair of Policy of the American Bar Association International Section Life Sciences Committee and an active in a host of migration reform and other cross-border workforce, pandemic and other healthcare, education, ethics, cyber crime policy reforms within and outside the United States throughout her career, Ms. Stamer also has extensive experience working with domestic and foreign businesses on a host of immigration, workforce, compensation, benefits, privacy, and other compliance and management challenges arising in connection with the management and use of ex-pat and other global workforces by U.S. and foreign businesses.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association, the US-Mexico Chamber of Commerce and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com.
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2017 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on RAISE Act Immigration Reforms Touted As “Giving Americans A Raise” |
Comments Off on RAISE Act Immigration Reforms Touted As “Giving Americans A Raise” |  Discrimination, E-Verify, EEOC, EEOC, employee, Employee Benefits, Employer, Employers, English As A Second Language, h-2A Visa, health benefit, Health Benefits, health Care, health insurance, health plan, Health Plans, Hiring, HR, I-9, Immigration, Internal Controls, RAISE Act, Uncategorized, visas, Worker | Tagged: EEOC, ESL, Immigration, International, Migration, RAISE Act |
Discrimination, E-Verify, EEOC, EEOC, employee, Employee Benefits, Employer, Employers, English As A Second Language, h-2A Visa, health benefit, Health Benefits, health Care, health insurance, health plan, Health Plans, Hiring, HR, I-9, Immigration, Internal Controls, RAISE Act, Uncategorized, visas, Worker | Tagged: EEOC, ESL, Immigration, International, Migration, RAISE Act |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
August 1, 2017
Employers and employee benefit plan fiduciaries and administrators should consider sharing the free IRS Withholding Calculator resource offered in English, Spanish, and ASL formats with workers in annual employee benefit enrollment packages, new hire paperwork, bonus announcement and other wage related materials and other employee communications to help workers better understand and manage the tax and other effects of their annual employee benefit elections on their take-home pay. Including reminders to re-evaluate withholding and if necessary, change their W-4 withholding elections also helps employees and their families ensure that withholding elections that workers complete as part of new hire documentation are updated in response to changing taxable income and other relevant events.
Communicating the availability of these free government-resource tools to workers during the annual employee benefit plan enrollment period, year-end, raise or bonus time or other strategic times throughout the year could help employees better appreciate the tax-preferred benefit offerings provided by the employer as well as provide significant financial education benefits many workers need for little or no employer cost.
While enrollment packages typically tout the potential “tax savings” that employees can enjoy from participating in tax-favored, employer-sponsored health, group term life, qualified pension or profit-sharing, and other tax-preferred employee benefit or fringe benefit programs offered by their employers, few employees truly understand how to determine properly their necessary wage withholding on taxable wages, much less the specific effects of their employee benefit elections on their income or employment tax liability or withholding.
A better understanding of the relative tax benefits and savings of enrollment in tax-preferred benefits offered by an employer and their potential implications on the income tax withholding elected by the workers can benefit both employees and their employer. Aside from illustrating in real, meaningful terms specific to the worker the tax benefits of his election of employer-offered, tax preferred benefits, proper tax withholding helps employees avoid unnecessary over withholding that can reduce employees’ take-home pay as well as helps protect employees from unexpectedly higher year-end tax bills that often surprise workers when an employee sets his withholding too low.
While few employers or plans want to incur the potential financial costs or liability of estimating savings for individual workers, sharing information about free government-provided resources like the IRS calculator or using vendor-provided solutions that incorporate tools in employee enrollment and other communications can help employees appreciate the benefits of tax-preferred employee benefits and make more informed choices about their benefits and their withholding.
Educating employees about the availability of these free resources also is a low-cost way of providing valuable information to workers whether or not the employer or plan has a vendor offered solution that includes the same or similar tool. However, educating workers about the availability of the withholding calculator and other tools can be a particularly attractive option for an employer when the employer doesn’t have a vendor-provided option that includes that information or can only access the tool for added charges.
While many vendors offer similar tools and materials sold to employers and employee benefit plans, employers or benefit plan fiduciaries generally must pay fees, share promotional materials or meet at the requirements to deliver those resources as part of a vendor-supplied package. Utilizing these vendor supplied resources without fulfilling these preconditions could expose the employer or plan to potential copyright, trademark or other contractual or intellectual property claims from the vendor. In contrast, IRS withholding calculator and many other government tools can be used or shared freely without these concerns. Moreover, employers and plans are less likely to face challenges for sharing an unfiltered government resource than a similar tool packaged within a vendor communication package promoting other options.
Of course, regardless of whether these or other tools or information are shared as a free-standing tool or as part of a broader communication package, employers, plans and others sharing these government tools and other similar resources generally will want to ensure that the materials are distributed along with and subject to general tax advice and other disclaimers of reliance as well as statements encouraging users to consult with their own qualified tax or other qualified professionals about the users’ specific circumstance.
About The Author
Recognized by her peers as a Martindale-Hubble “AV-Preeminent” (Top 1%) and “Top Rated Lawyer” with special recognition LexisNexis® Martindale-Hubbell® as “LEGAL LEADER™ Texas Top Rated Lawyer” in Health Care Law and Labor and Employment Law; as among the “Best Lawyers In Dallas” for her work in the fields of “Labor & Employment,” “Tax: Erisa & Employee Benefits,” “Health Care” and “Business and Commercial Law” by D Magazine, Cynthia Marcotte Stamer is a practicing attorney board certified in labor and employment law by the Texas Board of Legal Specialization and management consultant, author, public policy advocate and lecturer widely known for management work, coaching, teachings, and publications.
Ms. Stamer works with businesses and their management, employee benefit plans, governments and other organizations deal with all aspects of human resources and workforce, internal controls and regulatory compliance, change management and other performance and operations management and compliance. Her day-to-day work encompasses both labor and employment issues, as well as independent contractor, outsourcing, employee leasing, management services and other nontraditional service relationships. She supports her clients both on a real-time, “on demand” basis and with longer term basis to deal with all aspects for workforce and human resources management, including, recruitment, hiring, firing, compensation and benefits, promotion, discipline, compliance, trade secret and confidentiality, noncompetition, privacy and data security, safety, daily performance and operations management, emerging crises, strategic planning, process improvement and change management, investigations, defending litigation, audits, investigations or other enforcement challenges, government affairs and public policy.
Well-known for her extensive work with health, insurance, financial services, technology, energy, manufacturing, retail, hospitality, governmental and other highly regulated employers, her nearly 30 years’ of experience encompasses domestic and international businesses of all types and sizes.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares her thought leadership, experience and advocacy on these and other concerns by her service as a management consultant, business coach and consultant and policy strategist as well through her leadership participation in professional and civic organizations such her involvement as the Vice Chair of the North Texas Healthcare Compliance Association; Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE: Coalition on Patient Empowerment; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; former Gulf Coast TEGE Council Exempt Organization Coordinator; a founding Board Member and past President of the Alliance for Healthcare Excellence; former board member and Vice President of the Managed Care Association; past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; a member and policy adviser to the National Physicians’ Council for Healthcare Policy; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee; current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section; Past Chair of the ABA Health Law Section Managed Care & Insurance Section; ABA Real Property Probate and Trust (RPTE) Section former Employee Benefits Group Chair, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative, and Defined Contribution Committee Co-Chair, past Welfare Benefit Committee Chair and current Employee Benefits Group Fiduciary Responsibility Committee Co-Chair, Substantive and Group Committee member, Membership Committee member and RPTE Representative to the ABA Health Law Coordinating Council; past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee; a former member of the Board of Directors, Treasurer, Member and Continuing Education Chair of the Southwest Benefits Association and others.
Ms. Stamer also is a widely published author, highly popular lecturer, and serial symposia chair, who publishes and speaks extensively on human resources, labor and employment, employee benefits, compensation, occupational safety and health, and other leadership, performance, regulatory and operational risk management, public policy and community service concerns for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications.
Want to know more? See here for details about the author of this update, attorney Cynthia Marcotte Stamer, e-mail her here or telephone Ms. Stamer at (469) 767-8872.
About Solutions Law Press, Inc.™
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at SolutionsLawPress.com.
If you or someone else you know would like to receive future updates about developments on these and other concerns, please provide your current contact information and preferences including your preferred e-mail by creating or updating your profile here.
NOTICE: These statements and materials are for general informational and purposes only. They do not establish an attorney-client relationship, are not legal advice, and do not serve as a substitute for legal advice. Readers are urged to engage competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The presenter and the program sponsor disclaim, and have no responsibility to provide any update or otherwise notify any participant of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
Circular 230 Compliance. The following disclaimer is included to ensure that we comply with U.S. Treasury Department Regulations. Any statements contained herein are not intended or written by the writer to be used, and nothing contained herein can be used by you or any other person, for the purpose of (1) avoiding penalties that may be imposed under federal tax law, or (2) promoting, marketing or recommending to another party any tax-related transaction or matter addressed herein.
©2017 Cynthia Marcotte Stamer. Non-exclusive right to republish granted to Solutions Law Press, Inc.™ For information about republication, please contact the author directly. All other rights reserved.
 Comments Off on Withholding Calculator Tool Helps Workers Figure Withholding |
Comments Off on Withholding Calculator Tool Helps Workers Figure Withholding |  105(h), 401(k), Affordable Care Act, Brokers, Cafeteria Plans, compensation, compliance, Corporate Compliance, Default enrollment, defined benefit plan, Defined Benefit Plans, Defined Contribution Plans, Disability, Disability Plans, EBSA, employee, Employee Benefits, Employer, Employers, Employment, Employment Tax, Executive Compensation, FICA, fiduciary duty, Form 5500, HR, Human Resources, Income Tax, Insurance, Managment, Tax, Tax Qualification, Uncategorized, Worker, Workforce | Tagged: Employee Benefits, employee communications, Health Insurance, Human Resources, Income Tax, onboarding, Tax, Withholding, Workforce |
105(h), 401(k), Affordable Care Act, Brokers, Cafeteria Plans, compensation, compliance, Corporate Compliance, Default enrollment, defined benefit plan, Defined Benefit Plans, Defined Contribution Plans, Disability, Disability Plans, EBSA, employee, Employee Benefits, Employer, Employers, Employment, Employment Tax, Executive Compensation, FICA, fiduciary duty, Form 5500, HR, Human Resources, Income Tax, Insurance, Managment, Tax, Tax Qualification, Uncategorized, Worker, Workforce | Tagged: Employee Benefits, employee communications, Health Insurance, Human Resources, Income Tax, onboarding, Tax, Withholding, Workforce |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
June 22, 2017
Register Now To Participate In
“2017 Federal Group Health Plan Mental Health Rules Update”
Solutions Law Press, Inc™ Health Plan Update WebEx Briefing
Tuesday, June 27, 2017
10:30 A.M.-11:30 P.M. Eastern | 11:30 A.M.-12:30 P.M. Central
EXPANDING REGULATORY REQUIREMENTS & ENFORCEMENT SPELL TROUBLE FOR HEALTH PLANS AND THEIR SPONSORING EMPLOYERS.
Solutions Law Press, Inc.™ invites employer and other group health plan sponsors, fiduciaries, insurers, administrative service providers, plan brokers and consultants are invited learn critical information about their expanding risks and responsibilities arising from existing and proposed changes to rules and enforcement of federal group health plan mental health and substance abuse (MH/SUB) coverage and privacy rules under the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA), as supplemented by the Patient Protection and Affordable Care Act (ACA) and the 21st Century Cures Act (Cures Act) and the Privacy Rules of the Health Insurance Portability & Accountability Act (HIPAA) conducted by attorney Cynthia Marcotte Stamer, a Fellow in the American College of Employee Benefits recognized as among the “Best Lawyers” in employee benefits for her health and other benefit knowledge, experience, policy advocacy and thought leadership. Register here now!
Tightening Health Plan Mental Health & Substance Abuse Rules & Enforcement Make Group Health Plan Compliance Critical
New and proposed guidance jointly published June 16, 2017 by the Departments of Labor (DOL), Health & Human Services (HHS) and Treasury is the latest in a series of regulatory and enforcement developments over the past year alerting group health plans and their employer and other group health plan sponsors, fiduciaries, insurers, administrative services providers, plan brokers and consultants involved in health plan design, funding, or administration to get serious about their group health plans’ compliance with the MHPAEA federal group health plan mental health and substance abuse coverage and benefit requirements, as supplemented by the ACA and the Cures Act without running afoul of the Privacy Rules of HIPAA.
Building upon federal group health plan mental health parity mandates originally implemented under the Mental Health Parity Act, the MHPAEA generally requires that any financial requirements or treatment limitations group health plans impose on mental health and substance use disorder (MH/SUD) benefits not be restrictive than the predominant financial requirements and treatment limitations that apply to substantially all medical and surgical benefits. MHPAEA also imposes several disclosure requirements on group health plans and health insurance issuers. Not satisfied with the MHPAEA coverage and disclosure protections, however, Congress subsequently broadened federal MH/SUD benefit rights under group health plans through the enactment of the ACA and the Cures Act. Congress also has imposed special requirements and protections for mental health treatment records adds additional responsibilities for group health plans and their service providers when dealing with information and records in connection with the administration of MH/SUD benefits.
After a long period of lax oversight and enforcement of these federal group health plan mental health rules, the Departments of Labor (DOL), Health and Human Services (HHS), and the Treasury (collectively, the Departments) since October, 2016 have begun both tightening the rules and acting to increase oversight and enforcement. The Departments have issued a series of joint guidance clarifying and broadening their interpretations of these MH/SUD benefit and disclosure mandates while simultaneously taking steps to increase awareness and enforcement of these rights. As part of these ongoing efforts, Departments’ on June 16, 2017 expanded this guidance with their publication of new Mental Health Parity Implementation FAQs Part 38 discussing their joint interpretation of the broadening effect of the enactment of the ACA and the Cure Act on these plan requirements. Concurrently, the Departments signaled their intention to add additional responsibilities for group health plans and insurers by publishing along with FAQ Part 38 a Draft MHPAEA Disclosure Template and request for comments. This latest guidance package reaffirms that the Departments are continuing efforts to increase oversight of and enforcement of MH/SUD compliance against group health plans, their sponsors, fiduciaries, insurers, and their administrative and other service providers. In the face of these developments and the reported initiation of enforcement actions by the Departments, the group health plans, their employer and other sponsors, fiduciaries, insurers, and their administrative and other service providers should move quickly to understand and update their plans and practices to comply with these recent developments while bracing for the likely need to deal with further expanded disclosure and other additional responsibilities under the MHPAEA jointly proposed by the Departments on June 16, 2017.
Beyond fulfilling these expanding MHPAEA responsibilities, health plan fiduciaries, administrators, insurers and sponsors also must ensure their health plan and its business associates comply with special rules concerning the protection, use and disclosure of mental health treatment records and information that may impact certain mental health treatment and other records received, used, retained or disclosed in the course of administering mental health, substance abuse or other provisions of their group health plans under the HIPAA Privacy Rules. Keeping in mind that HHS audit and enforcement of compliance by health plans and other HIPAA covered entities with HIPAA’s medical privacy and data security rules, health plan sponsors, fiduciaries, insurers and administrative and other service providers also should take the opportunity to verify that their plans and practices comply with special HIPAA rules impacting authorizations and other dealings with certain mental health and substance abuse health information and records and other HIPAA medical privacy and security requirements.
Given these developments, group health plans, their sponsors, fiduciaries, insurers and administrator must take steps to verify and maintain compliance with these federal MH/SUD requirements. Ensuring proper compliance with these federal rules is particularly important to avoid triggering the substantial liability that health plans, their employer and other sponsors, insurers, and administrators can incur if their health plan violates these mandates. Obviously, plans and their sponsors, insurers and fiduciaries can expect to pay additional plan expenses necessary to pay wrongfully denied benefits and other expenditures these plan or its fiduciaries expend to investigate, defend and resolve claims or compliance audits, investigations, litigation or actions brought by the Departments, state insurance regulators with respect to state governments or insurers, or private litigation by participants or beneficiaries. Many employer or other plan sponsors may be unaware that these violations also generally expose employers and other health plan sponsors to liability to self identify, self-report on Internal Revenue Service Form 8928 and self-pay and excise tax of up to $100 per participant per day per uncorrected violation by the due date for filing of their annual corporate tax return.
With oversight and enforcement already rising and the Departments proposing to expand further both disclosure duties and enforcement, group health plans, their employer and other sponsors, insurers, fiduciaries and administrators clearly need to take prompt action to verify their existing health plan provisions and administrative practices are up-to-date and administered to withstand challenge from the Departments, participants, beneficiaries, health care providers and others. Consequently, employer and other group health plan sponsors, fiduciaries, insurers, administrative services providers, plan brokers and consultants involved in health plan design, funding, or administration should act quickly to verify their plan terms and practices are updated to comply with existing rules and share their input in response to the Departments June 16, 2017 requests for comments.
ABOUT CYNTHIA MARCOTTE STAMER
Recognized as “Legal Leader™ Texas Top Rated Lawyer” in both Health Care Law and Labor and Employment Law, a “Texas Top Lawyer,” and an “AV-Preeminent” and “Top Rated Lawyer” by Martindale-Hubble, singled out as among the “Best Lawyers In Dallas” in employee benefits by D Magazine; Cynthia Marcotte Stamer is a practicing attorney and management consultant, author, public policy advocate and lecturer widely recognized for her nearly 30 years’ of work and pragmatic thought leadership, publications and training on health coverage and health care, health plan and employee benefits, workforce and related regulatory and other compliance, performance management, risk management, product and process development, public policy, operations and other concerns.
Throughout her legal and consulting career, Ms. Stamer has drawn recognition for combining extensive knowledge and experience with her talents as an insightful innovator and problem solver when advising, representing and defending employer and other plan sponsors, insurers, fiduciaries, insurers, electronic and other technology, plan administrators and other service providers, governments and others about health coverage, benefit program design, funding, documentation, administration, data security and use, contracting, plan, public and regulatory reforms and enforcement, and other risk management and operations matters as well as for her work and thought leadership on a broad range of other health, employee benefits, human resources and other workforce, insurance, tax, compliance and other matters. Her experience encompasses leading and supporting the development and defense of innovative new programs, practices and solutions; advising and representing clients on routine plan establishment, plan documentation and contract drafting and review, administration, change and other compliance and operations crisis prevention and response, compliance and risk management audits and investigations, enforcement actions and other dealings with the US Congress, Departments of Labor, Treasury, Health & Human Services, Federal Trade Commission, Justice, state legislatures, attorneys general, insurance, labor, worker’s compensation, and other agencies and regulators, She also provides strategic and other supports clients in defending litigation as lead strategy counsel, special counsel and as an expert witness.
A Fellow in the American College of Employee Benefit Counsel, the American Bar Foundation and the Texas Bar Foundation, Ms. Stamer also shares shared her thought leadership, experience and advocacy on these and other concerns by her service in the leadership of a broad range of other professional and civic organization including her involvement as Executive Director of the Coalition on Responsible Health Policy and its PROJECT COPE; Coalition on Patient Empowerment, a founding Board Member and past President of the Alliance for Healthcare Excellence, past Board Member and Board Compliance Committee Chair for the National Kidney Foundation of North Texas; former Board President of the early childhood development intervention agency, The Richardson Development Center for Children; current Vice Chair of the ABA Tort & Insurance Practice Section Employee Benefits Committee, current Vice Chair of Policy for the Life Sciences Committee of the ABA International Section, Past Chair of the ABA Health Law Section Managed Care & Insurance Section, Past Group Chair, current Defined Contribution Plan Committee Co-Chair, former Welfare Committee Chair and Co-Chair of the ABA RPTE Section Employee Benefits Group, immediate past RPTE Representative to ABA Joint Committee on Employee Benefits Council Representative and current RPTE Representative to the ABA Health Law Coordinating Counsel, former Coordinator and a Vice-Chair of the Gulf Coast TEGE Council TE Division, past Chair of the Dallas Bar Association Employee Benefits & Executive Compensation Committee, former member of the Board of Directors of the Southwest Benefits Association and others.
Ms. Stamer also is a highly popular lecturer, symposia chair and author, who publishes and speaks extensively on health and managed care industry, human resources, employment and other privacy, data security and other technology, regulatory and operational risk management for the American Bar Association, ALI-ABA, American Health Lawyers, Society of Human Resources Professionals, the Southwest Benefits Association, the Society of Employee Benefits Administrators, the American Law Institute, Lexis-Nexis, Atlantic Information Services, The Bureau of National Affairs (BNA), InsuranceThoughtLeaders.com, the Society of Professional Benefits Administrators, Benefits Magazine, Employee Benefit News, Texas CEO Magazine, HealthLeaders, the HCCA, ISSA, HIMSS, Modern Healthcare, Managed Healthcare, Institute of Internal Auditors, Society of CPAs, Business Insurance, Employee Benefits News, World At Work, Benefits Magazine, the Wall Street Journal, the Dallas Morning News, the Dallas Business Journal, the Houston Business Journal, and many other symposia and publications. She also has served as an Editorial Advisory Board Member for human resources, employee benefit and other management focused publications of BNA, HR.com, Employee Benefit News, InsuranceThoughtLeadership.com and many other prominent publications and speaks and conducts training for a broad range of professional organizations and for clients, serves on the faculty and planning committee of many workshops, seminars, and symposia, and on the Advisory Boards of InsuranceThoughtLeadership.com, HR.com, Employee Benefit News, and many other publications. For additional information about Ms. Stamer, see CynthiaStamer.com or contact Ms. Stamer via email to here or via telephone to (469) 767-8872.
About Solutions Law Press
Solutions Law Press, Inc.™ provides human resources and employee benefit and other business risk management, legal compliance, management effectiveness and other coaching, tools and other resources, training and education on leadership, governance, human resources, employee benefits, data security and privacy, insurance, health care and other key compliance, risk management, internal controls and operational concerns. If you find this of interest, you also be interested reviewing some of our other Solutions Law Press, Inc.™ resources at www.SolutionsLawPress.com.
If you or someone else you know would like to receive future updates and notices about other upcoming Solutions Law Press™ events, please be sure that we have your current contact information – including your preferred e-mail by creating or updating your profile here. For important information concerning this communication, see here.
NOTICE: Any party accessing or using any content obtained from or through Solutions Law Press, Inc.™ acknowledges and agrees that any and all programs, publications, statements and materials presented or published by Solutions Law Press, Inc.™ and any statements or other contents made or contained therein are for general informational and educational purposes only. They are generic in nature and not tailored or intended to be relied upon by any person, business, entity or other party for purposes for determining the legal, financial or other appropriateness, defensibility, suitability, outcome or consequences of any strategy, action, course of action, or any other facts, circumstances, event or conduct. Users of these resources are responsible at all times for independently evluating the suitability of any content, materials, tools or other materials or information accessed from or through Solutions Law Press, Inc. directly or indirectly.
Solutions Law Press, Inc.™ and its authors and contributors do not represent or warrant in any form or manner, and expressly disclaim and deny the appropriateness of the use or reliance of any person or entity on any content, tools or resources accessed or obtained from or through Solutions Law Press, Inc.™ for any general or particular use or purpose by any party under any circumstances.
Likewise, they do not establish an attorney-client relationship or other fiduciary, contractual or other relationship between Solutions Law Press, Inc. and/or any of its authors or contributors and any other party. They are not, and do not serve as a substitute for legal, accounting, tax or other advice. They don’t create or otherwise give rise to any duty, obligation, responsibility on behalf of Solutions Law Press, Inc™ or any provider or offeree of content, tools or services to any party.
Parties accessing or using any of Solutions Law Press, Inc.™ competent legal counsel for consultation and representation in light of the specific facts and circumstances presented in their unique circumstance at any particular time. No comment or statement in this publication is to be construed as an admission. The author reserves the right to qualify or retract any of these statements at any time. Likewise, the content is not tailored to any particular situation and does not necessarily address all relevant issues. Because the law is rapidly evolving and rapidly evolving rules makes it highly likely that subsequent developments could impact the currency and completeness of this discussion. The publisher and the author expressly disclaim all liability for this content and any responsibility to provide any update or otherwise notify anyone of any such change, limitation, or other condition that might affect the suitability of reliance upon these materials or information otherwise conveyed in connection with this program. Readers may not rely upon, are solely responsible for, and assume the risk and all liabilities resulting from their use of this publication.
©2017 Solutions Law Press. All rights reserved.
 Comments Off on Learn About Rising Group Health Plan Mental Health Mandate Risks From 6/27 “2017 Federal Group Health Plan Mental Health Rules Update” |
Comments Off on Learn About Rising Group Health Plan Mental Health Mandate Risks From 6/27 “2017 Federal Group Health Plan Mental Health Rules Update” |  4980D, 6039D, ACA, Affordable Care Act, Appeals, Attorney-Client Privilege, board of directors, Brokers, Cafeteria Plans, church plan, Civil Monetary Penalties, Civil Rights, Claims, Claims Administration, compensation, compliance, conflict of interest, Corporate Compliance, corporate governance, Data Breach, Data Security, EBSA, employee, Employee Benefits, Employer, Employers, Employment, Employment Tax, ERISA, Excepted Benefits, exchange, Excise Tax, Excise Taxes, Exempt, fiduciary duty, Fiduciary Responsibility, H.R. 4872, health reform, HIPAA, HR, Human Resources, Identity Theft, Income Tax, Insurance, insurers, Internal Revenue Code, IRC, Labor Management Relations, Management, Mental Health, Mental Health Parity, MEWA, Obamacare, Patient Protection & Affordable Care Act, Pay, Physician, Plan Admistrator, preventive care, Privacy, Professional Liability, Protected Health Information, Provider, Risk Management, SBC, Tax Credit, Uncategorized, Union | Tagged: ACA, Brokers, CCIIO, Corporate Compliance, EBSA, Employers, enforcement, Essential health benefits, Fiduciary, Fiduciary Duties, Health Benefits, health coverage, Health Plans, health reform, HHS, Mental Health, Mental Health Parity, mental health records, substance abuse, Third party Administrators |
4980D, 6039D, ACA, Affordable Care Act, Appeals, Attorney-Client Privilege, board of directors, Brokers, Cafeteria Plans, church plan, Civil Monetary Penalties, Civil Rights, Claims, Claims Administration, compensation, compliance, conflict of interest, Corporate Compliance, corporate governance, Data Breach, Data Security, EBSA, employee, Employee Benefits, Employer, Employers, Employment, Employment Tax, ERISA, Excepted Benefits, exchange, Excise Tax, Excise Taxes, Exempt, fiduciary duty, Fiduciary Responsibility, H.R. 4872, health reform, HIPAA, HR, Human Resources, Identity Theft, Income Tax, Insurance, insurers, Internal Revenue Code, IRC, Labor Management Relations, Management, Mental Health, Mental Health Parity, MEWA, Obamacare, Patient Protection & Affordable Care Act, Pay, Physician, Plan Admistrator, preventive care, Privacy, Professional Liability, Protected Health Information, Provider, Risk Management, SBC, Tax Credit, Uncategorized, Union | Tagged: ACA, Brokers, CCIIO, Corporate Compliance, EBSA, Employers, enforcement, Essential health benefits, Fiduciary, Fiduciary Duties, Health Benefits, health coverage, Health Plans, health reform, HHS, Mental Health, Mental Health Parity, mental health records, substance abuse, Third party Administrators |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer
May 12, 2017
Solutions Law Press, Inc. editor and attorney Cynthia Marcotte Stamer will speak and moderate two key panel programs on health care privacy and data security scheduled at the Healthcare Privacy & Security Form hosted on May 19, 2017 by the Information Security Systems Association of Los Angeles County (ISSA-LA) as a component of its 9th Annual ISSA-LA Information Security Summit. The presentations of Ms. Stamer and others at the conference are particularly timely coming on the heels of the May 12 Cyber alerts to U.S. health industry and other businesses about the urgent need to defend against the spread of an epidemic international malware threat targeting U.S. healthcare and other businesses. See Urgent WannaCry Ransomware Cyber Warning Issued; Alert: Guard Health E-Mail, Other IT Against WannaCry Malware Attack.
The Medical Privacy & Security Summit is part of the 9th Annual ISSA-LA Information Security Summit scheduled for May 18-19, 2017 at the Universal City Hilton in Los Angeles. Recognized as a premier information security education and networking event, the Summit is expected to bring together 1000 or more health industry and other IT and InfoSec executives, leaders, analysts, and practitioners to learn from the experts, exchange ideas with their peers, and enjoy conversations with the community.
The Healthcare Privacy & Security Forum offered for the 5th year as a component of the annual Summit on May 19 specifically focuses on leading challenges, issues and opportunities confronted by health industry privacy and security professionals and their organizations. Ms. Stamer has served on the steering committee, moderator and popular faculty member for the 2017 Forum for the 5th consecutive year. During the 2017 Forum, she will moderate and speak on two panels:
- “Finding & Negotiating The Mine Fields: CISO, CIO & Privacy Officer’s Playbook for Promoting Compliance & Security Without Getting Fired,” a luncheon interactive panel discussion with the audience exploring the challenging mission CISOs, CIOs and Privacy Officers face to ensure their healthcare, financial and other critical information, data and systems continue to support the patient care and operating functions of their organizations, while at the same time defending these systems, operations and their sensitive, but mission critical data against malicious or innocent misappropriation, use, access or destruction; and
- The closing panel on “What Initiatives Are on the Horizon in Healthcare, and How Can We Secure Them?”, which will explore likely future emerging privacy and security threats and technologies, regulatory challenges and enforcement, and other trends that Privacy and Security professionals are likely to face and tips and strategies for preparing to leverage these likely new opportunities and manage new challenges.
Register or get the full schedule of programs and other events scheduled at the Healthcare Privacy & Security Forum specifically along with the overall Information Security Summit here.
About Ms. Stamer
Cynthia Marcotte Stamer is a Martindale-Hubble “AV-Preeminent (Top 1%) rated practicing attorney and management consultant, health industry public policy advocate, widely published author and lecturer, recognized for her nearly 30 years’ of work on health industry and other privacy and data security and other health care, health benefit, health policy and regulatory affairs and other health industry legal and operational as a LexisNexis® Martindale-Hubbell® “LEGAL LEADER™ and “Top Rated Lawyer,” in Health Care Law and Labor and Employment Law; a D Magazine “Best Lawyers In Dallas” in the fields of “Health Care,” “Labor & Employment,” “Tax: Erisa & Employee Benefits” and “Business and Commercial Law,” a Fellow in the American Bar Foundation, the Texas Bar Foundation and the American College of Employee Benefit Counsel.
Scribe for ABA JCEB annual agency meeting with OCR for many years, Ms. Stamer is well-known for her extensive work and leadership throughout her career on HIPAA, FACTA, PCI, IRC and other tax, Social Security, GLB, trade secret, physician and other medical confidentiality and privacy, federal and state data security and data breach and other information privacy and data security rules and concerns. Ms. Stamer has worked extensively throughout her career with health care providers, health plans, health care clearinghouses, their business associates, employers and other plan sponsors, banks, insurers and other financial institutions, and others on trade secret confidentiality, privacy, data security and other risk management and compliance including design, establishment, documentation, implementation, audit and enforcement of policies, procedures, systems and safeguards, drafting and negotiation of business associate, chain of custody, confidentiality, and other contracting; risk assessments, audits and other risk prevention and mitigation; investigation, reporting, mitigation and resolution of known or suspected breaches, violations or other incidents; and defending investigations or other actions by plaintiffs, OCR, FTC, state attorneys’ general and other federal or state agencies, other business partners, patients and others; reporting known or suspected violations; commenting or obtaining other clarification of guidance and other regulatory affairs, training and enforcement, and a host of other related concerns.
Her clients include public and private health care providers, health insurers, health plans, employers, payroll, staffing, recruitment, insurance and financial services, health and other technology and other vendors, and others.
Author of a multitude of highly-regarded works and training programs on HIPAA and other data security, privacy and use published by BNA, the ABA and other premier legal industry publishers In addition to representing and advising these organizations, she also speaks extensively and conducts training on health care and other privacy and data security and many other matters Privacy & The Pandemic for the Association of State & Territorial Health Plans, as well as HIPAA, FACTA, PCI, medical confidentiality, insurance confidentiality and other privacy and data security compliance and risk management for Los Angeles County Health Department, ISSA, HIMMS, the ABA, SHRM, schools, medical societies, government and private health care and health plan organizations, their business associates, trade associations and others.
Beyond these involvements, Ms. Stamer also is active in the leadership of a broad range of other professional and civic organizations. Through these and other involvements, she helps develop and build solutions, build consensus, garner funding and other resources, manage compliance and other operations, and take other actions to identify promote tangible improvements in health care and other policy and operational areas.
For additional information about Ms. Stamer, see here or contact Ms. Stamer directly by e-mail here or by telephone at (469) 767-8872. ©2017 Cynthia Marcotte Stamer. Limited, non-exclusive right to republish granted to Solutions Law Press, Inc. All other rights reserved.
 Comments Off on Stamer To Moderate, Talk Medical CyberSecurity At 5/19 ISSA-LA IT Security Meedical Privacy Forum |
Comments Off on Stamer To Moderate, Talk Medical CyberSecurity At 5/19 ISSA-LA IT Security Meedical Privacy Forum |  ADA, ARRA, board of directors, Brokers, Child Safety, Civil Monetary Penalties, compliance, Consumer Protection, Corporate Compliance, corporate governance, Cybercrime, Data Breach, Data Security, EBSA, Educational Privacy, Electronic Medical Record, employee, Employee Benefits, Employer, Employers, EMR, ERISA, FACTA, Fair Credit Reporting Act, FICA, fiduciary duty, FINRA, Government Contractors, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, health plan, Health Plans, HIPAA, HIPAA, HR, Human Resources, Identity Theft, Insurance, insurers, Internal Controls, Internal Investigations, Internet, Management, Mental Health, officers, Physician, Plan Admistrator, Privacy, Professional Liability, Protected Health Information, Provider, Public Policy, Security, Technology, third party administrators, Uncategorized | Tagged: Cyber Security, Cybercrime, Data Security, Information Security, IT, medical data, Medical Privacy, medical security, Protected Health Information, speech |
ADA, ARRA, board of directors, Brokers, Child Safety, Civil Monetary Penalties, compliance, Consumer Protection, Corporate Compliance, corporate governance, Cybercrime, Data Breach, Data Security, EBSA, Educational Privacy, Electronic Medical Record, employee, Employee Benefits, Employer, Employers, EMR, ERISA, FACTA, Fair Credit Reporting Act, FICA, fiduciary duty, FINRA, Government Contractors, health benefit, Health Benefits, health Care, health insurance, health insurance marketplace, health plan, Health Plans, HIPAA, HIPAA, HR, Human Resources, Identity Theft, Insurance, insurers, Internal Controls, Internal Investigations, Internet, Management, Mental Health, officers, Physician, Plan Admistrator, Privacy, Professional Liability, Protected Health Information, Provider, Public Policy, Security, Technology, third party administrators, Uncategorized | Tagged: Cyber Security, Cybercrime, Data Security, Information Security, IT, medical data, Medical Privacy, medical security, Protected Health Information, speech |  Permalink
Permalink
 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer



 Posted by Cynthia Marcotte Stamer
Posted by Cynthia Marcotte Stamer 
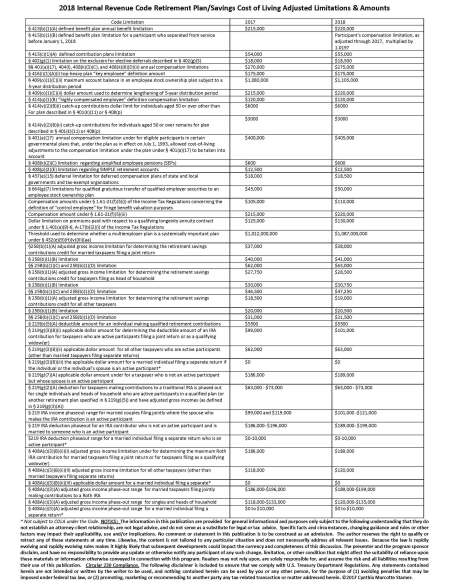
 Teamwork is a valuable and necessary to organizational performance in most workplaces. However management undermines team performance and effectiveness by giving participation trophies to team members that don’t give their best when working on teams.
Teamwork is a valuable and necessary to organizational performance in most workplaces. However management undermines team performance and effectiveness by giving participation trophies to team members that don’t give their best when working on teams.
You must be logged in to post a comment.